Patient Satisfaction with a Multidisciplinary Team Approach to Uterine Artery Embolisation: Preliminary Results
ORIGINAL ARTICLE
Patient Satisfaction with a Multidisciplinary Team Approach to Uterine Artery Embolisation: Preliminary Results
SY Lam1, HL Wong1, TSC Ling2, HF Hui2, S Sasaki3, YL Ho3, OC Leung1, JCW Siu1, CB Tan1
1 Department of Radiology, Tuen Mun Hospital, Hong Kong
2 Department of Obstetrics and Gynaecology, Tuen Mun Hospital, Hong Kong
3 Department of Anaesthesiology and Intensive Care, Tuen Mun Hospital, Hong Kong
Correspondence: Dr SY Lam, Department of Radiology, Tuen Mun Hospital, Hong Kong. Email: pikapat@yahoo.com
Submitted: 6 Oct 2018; Accepted: 11 Dec 2018.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Clinical and Research Ethics Committee of New Territories West Cluster (Ref 18037). All
patients provided written informed consent for the procedures and to participate in the survey.
Abstract
Objective
To evaluate patients’ experience of uterine artery embolisation (UAE) using a multidisciplinary team
approach to treat symptomatic fibroids, as well as clinical outcome and radiological outcome, in our local institution.
Methods
This was a single-centre retrospective follow-up study involving the departments of gynaecology,
anaesthesiology, and radiology. All women who underwent UAE for symptomatic uterine fibroids from October
2014 to November 2017 were included. Patients received periprocedural monitored anaesthesia care (MAC) and
postprocedural anaesthetic care including patient-controlled analgesia. Questionnaires were given to all patients
3 months after UAE to assess their experience in terms of pain control, length of hospital stay, and length of time until
return to work. Magnetic resonance imaging was performed before and after UAE to assess radiological outcomes.
Results
Periprocedural pain control with MAC and postprocedural pain control with patient-controlled analgesia
had mean numeric rating scale pain scores (where 0 represented no pain and 10 represented worst pain imaginable)
of 2.0 and 6.4, respectively. Of 26 patients, 14 (53.8%) had length of hospital stay of 2 nights, and 10 (38.5%) took
15 to 20 days to recover after the procedure and return to work. Significant reduction of uterine and fibroid volume
was seen on MRIs after UAE (p < 0.001).
Conclusion
Preliminary results of our multidisciplinary team approach to UAE are promising in terms of patient
experience, and radiological outcomes are consistent with the literature. Further studies are required for continuing
clinical appraisal and improvement at our institution.
Key Words: Leiomyoma; Pain management; Patient satisfaction; Surveys and questionnaires; Uterine artery
embolization
中文摘要
子宮動脈栓塞患者對多學科診療模式的滿意度:初步結果
林晨裕、黃皓廉、凌霄志、許海鋒、佐佐木純麗、何有良、梁安祥、蕭志偉、陳崇文
目的
評估子宮動脈栓塞(UAE)患者對多學科診療模式治療有症狀肌瘤的滿意度,以及臨床和放射學結果。
方法
這項單中心回顧性隨訪研究涉及婦科、麻醉科和放射科,納入2014年10月至2017年11月期間因徵狀子宮肌瘤接受UAE治療的女性。患者接受圍手術期監測麻醉護理(periprocedural monitored anaesthesia care,MAC)以及包括病人自控鎮痛(patient-controlled analgesia,PCA)的術後麻醉護理。UAE術後 3 個月對所有患者進行問卷調查,評估他們在疼痛控制的體驗、住院時間和康復後重返工作所需時間。於UAE前和UAE後進行磁共振成像以評估放射學結果。
結果
圍手術期MAC和術後PCA疼痛控制的平均疼痛評分分別為2.0和6.4(其中0表示沒有疼痛,10表示可以想像的最嚴重疼痛)。平均住院時間約為2.5晚。在26 名患者中,14名(53.8%)留院2晚,10名(38.5%)在手術後15至20天康復後重返工作。MRI顯示UAE後子宮和肌瘤體積顯著縮小(p < 0.001)。
結論
患者對多學科診療模式治療UAE的滿意度初步結果令人鼓舞,放射學結果與文獻一致。需要進一步研究臨床評估和進行持續的相關改進。
INTRODUCTION
Uterine artery embolisation (UAE) is an alternative to
surgery for patients with symptomatic fibroids. Compared
with surgery, UAE is a less-invasive procedure with
reduced complication and anaesthetic risks.[1] Few cases
of UAE had been performed in our institution before
implementation of our study, largely limited by patient
pain intolerance during and after the procedure.
A successful UAE procedure is not determined by
radiological outcome only; patients’ experience and
satisfaction also play a key role. With this in mind, our
institution established a multidisciplinary team approach
for patients undergoing UAE, with collaboration among
the departments of gynaecology, anaesthesiology, and
radiology. Since October 2014, UAE in our institution
is performed under monitored anaesthesia care (MAC),
and the goal of anaesthesia care after UAE is satisfactory
patient pain control. Magnetic resonance imaging (MRI)
is performed before and after UAE to assess the outcome
of embolisation.
The objective of this study was to evaluate patients’
experience of a multidisciplinary team approach to
UAE in terms of pain control, length of hospital stay,
and length of time until return to work. This study may provide useful information on the validity of the
anaesthesia methods for UAE and possibly guide future
implementation in our practice.
METHODS
Our study was a single-centre retrospective follow-up
study involving the departments of gynaecology,
anaesthesiology, and radiology for patients with
symptomatic fibroids undergoing UAE. Patients
experiencing symptoms including menorrhagia,
dysmenorrhoea and pressure effects that were diagnosed
with fibroids with ultrasound were referred from the
gynaecology clinic. The risks and benefits of surgery and
UAE were explained to the patients, and patients made
the final decision to opt for UAE or surgery. Patients with
active pelvic inflammatory disease, renal insufficiency,
endometrial carcinoma, undiagnosed pelvic mass, or
pregnancy were excluded from this study. Preprocedural
MRI was performed to delineate the location of fibroids
and the anatomy of uterine arteries.
All patients who underwent UAE for symptomatic
uterine fibroids from October 2014 to November 2017
were included in the study. All patients received MAC
during UAE, and pain management after UAE was
provided by the anaesthetic team, including patient-controlled analgesia (PCA) and oral medication. All
UAE procedures were performed by one of five principal
interventional radiologists in our centre with specialist
fellowship qualification. Superselective catheterisation
of uterine artery branches was performed. Embolic agents
used included polyvinyl alcohol particles (Contour;
Ivalon, Boston Scientific Inc., Natick [MA], US) and
trisacryl gelatin microspheres (Embosphere; Biosphere
Medical, Rockland [MA], US). Upon discharge from
hospital, patients were scheduled for a gynaecology
clinic follow-up examination at 3 months after UAE.
Radiological outcome, in terms of uterine fibroid
volume reduction, was assessed by MRI at 6 months
after UAE.
Uterine Artery Embolisation for Symptomatic Fibroids
All patients in the study were from the gynaecology unit
for symptomatic fibroids with the initial diagnosis made
by a gynaecologist using ultrasonography. The option
of UAE was offered and preferred over conservative
treatment or surgery. Informed consent was obtained
from patients for UAE with the 3-month follow-up
questionnaires. Preprocedural MRI was performed
to evaluate the anatomy of the fibroids. Pedunculated
subserosal and submucosal fibroids were of concern due
to the risk of detachment after UAE and the possible need
for subsequent endoscopic intervention for removal.[1]
The vascular anatomy depicted on MRI provided a
roadmap for planning UAE. Multidisciplinary team
meetings were held to discuss each case before UAE for
feasibility, mode of anaesthesia and pain control, MRI
findings, and anticipation of potential risk factors and
complications. All patients were performed as elective
cases with antibiotics coverage before UAE. There
were five principal interventional radiologists who
performed all the UAE procedures, two had more than
15 years, one had more than 10 years and two had more
than 5 years of experience as specialist radiologists,
respectively. Under fluoroscopic and digital subtraction
angiography guidance (AlluraClarity FD20; Philips,
Eindhoven, the Netherlands), the internal iliac arteries
were catheterised with 4-French (Fr) Cobra-1 or 4-Fr
Sim-1 (Cordis Inc., Bridgewater [NJ], US) catheters.
Subsequent catheterisation of both uterine arteries using
a microcatheter (2.4-Fr Maestro; Merit Medical Systems,
South Jordan [UT], US) were performed with guidance
into the ascending branches (distal to horizontal).
Embolisations were performed until stasis of contrast
material was noted in the uterine arteries. Embolic agents
included polyvinyl alcohol (Contour) of 355 to 500 μm and trisacryl gelatin microspheres (Embosphere) of 500 to 700 μm in size.
Pain Control
All UAE were performed under MAC in the presence
of an anaesthetist. Patients were premedicated with
90 mg etoricoxib (or 1 g paracetamol if etoricoxib
was contra-indicated), 300 mg gabapentin, and 8 mg
ondansetron. Drugs used for sedation included target-controlled
infusion of propofol (0.5-1.5 μg/mL) or
dexmedetomidine (0.2-1 μg/kg/h), fentanyl (25-200 μg),
and/or morphine boluses (3-9 mg) for opioid loading to
achieve an effective concentration prior to the use of PCA.
The drugs used for PCA included fentanyl or morphine
and were started as soon as the patient returned to the
ward and were continued for 1 to 3 days. For fentanyl
PCA, the drug concentration was 20 μg/mL, bolus dose
10 to 24 mg, lock out 5 to 6 minutes, 1-hour limit 100
to 220 μg. For morphine PCA, the drug concentration
was 1 mg/mL, bolus dose 1 mg, lock out between bolus
injections 8 to 10 minutes, 4-hour limit 18 to 30 mg.
Additional oral analgesics including paracetamol 1 g 4
times per day and etoricoxib 90 mg per day (or gabapentin
300 mg nightly if etoricoxib was contra-indicated) were
prescribed on a regular basis for 3 days, then as required
for an additional 2 to 4 days. Rescue drugs included
tramadol 50 mg every 6 hours orally or intramuscularly
and metoclopramide 10 mg every 8 hours intravenously.
Each patient was reviewed daily by the pain team until
cessation of the use of PCA.
Follow-up Questionnaires
Follow-up questionnaires (online supplementary Appendix) were used to assess patients’ experience with
UAE in terms of periprocedural and postprocedural pain
control, length of hospital stay, symptoms during hospital
stay, and length of time until return to work (recovery
time). The questionnaires were given to and completed
by the patients during the gynaecology clinic follow-up
examination at 3 months after UAE. Periprocedural and
postprocedural pain control was self-rated by patients
using a numeric rating scale (NRS), an 11-point (0 to
10) discrete score in determining pain severity, where 0
represented no pain and 10 represented the worst pain
imaginable. Scores of 1 to 3, 4 to 6, and 7 to 9 represented
mild, moderate, and severe pain, respectively.[2] The
questionnaire also included a list of signs and symptoms
that may have been experienced during hospital stay,
including pain, nausea, vomiting, fever, elevated blood
pressure, shortness of breath, aspiration pneumonia, and pleural effusion. Nursing staff or doctors explained the
signs and symptoms to patients, who were then asked in
the questionnaire to select those that were experienced.
Patients also self-reported length of hospital stay and
length of time until return to work in the questionnaire.
Radiological Outcomes
MRIs were performed before and after UAE to assess
volume reduction of uterus and fibroids using a 3.0T MR
scanner (Achieva; Philips, Eindhoven, the Netherlands).
MRI sequences included T2-weighted, T2-weighted fat-suppressed,
T1-weighted, T1-weighted fat-suppressed
spectral presaturation with inversion recovery and post-contrast,
and magnetic resonance angiography scans.
Images were reviewed with a picture archiving and
communication system (IMPAX; Agfa-Gevaert Group,
Mortsel, Belgium). Imaging features, including number
of fibroids, location and size of the largest (dominant)
fibroid (intramural, subserosal, submucosal), and size of
uterus were recorded. Volumes were calculated assuming
an oblate ellipsoid shape of both uterus and fibroid
with the formula (AP × TD × CC) × 0.5233, with AP
denoting anteroposterior, TD denoting transverse, and
CC denoting craniocaudal diameters. The change in size
of the dominant fibroid was used to determine volume
reduction. Volume measurements and calculations
were conducted independently by two radiologists with
5 and 7 years of experience, respectively. Using SPSS
(Windows version 23.0; IBM Corp, Armonk [NY], US),
a paired t test was performed to determine if volume
reduction before and after UAE would be statistically
significant in terms of overall uterus and dominant
fibroid volume reductions. Kappa statistic was used to
measure interobserver variability. The degree of necrosis
and enhancement on MRIs before and after UAE were
also assessed and discussed in the multidisciplinary team
meeting in conjunction with uterus and dominant fibroid
volume reduction.
RESULTS
No periprocedural complications were encountered.
Questionnaires were completed by all 26 patients at the
follow-up examination 3 months after UAE.
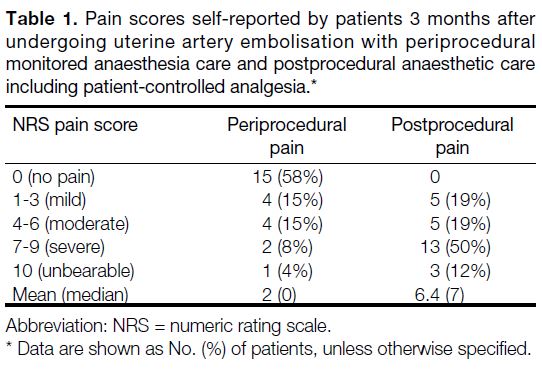
Patient-reported Pain
During UAE with MAC, the majority of patients
experienced no pain (n = 15, 58%). For periprocedural
pain, the mean NRS pain score was 2 and the median
NRS pain score was 0. After UAE with oral medication
and PCA, all patients experienced different degrees of
pain (Table 1).
Table 1. Pain scores self-reported by patients 3 months after undergoing uterine artery embolisation with periprocedural monitored anaesthesia care and postprocedural anaesthetic care
including patient-controlled analgesia.
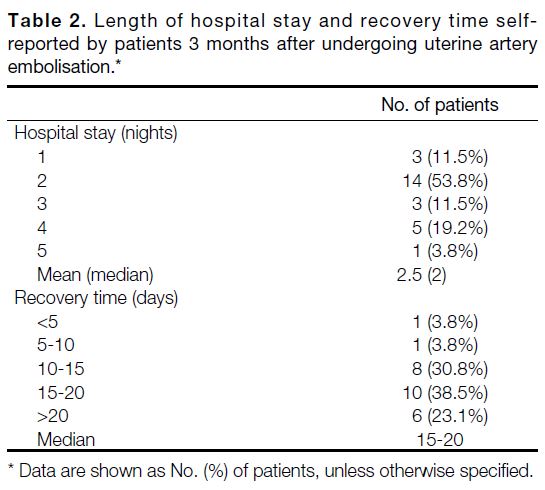
Length of Hospital Stay and Recovery Time
The majority of patients (n = 14, 54%) had two nights in
hospital after UAE and experienced pain (73%), fever
(4%), nausea (23%), vomiting (46%) and high blood
pressure (19%). One patient had a 5-night hospital stay
due to postprocedural bradycardia and hypertension. 10
patients (38.5%) took 15 to 20 days to recover after the
procedure and return to work (Table 2).
Table 2. Length of hospital stay and recovery time selfreported by patients 3 months after undergoing uterine artery embolisation.
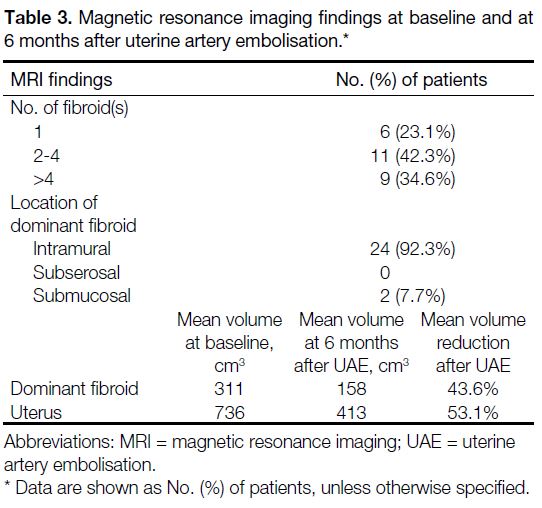
Most patients (76.9%) had multiple uterine fibroids
(Table 3). The dominant fibroids were mostly intramural
in location (92.3%). The mean volume reduction for the
dominant fibroid was 43.6%. The mean reduction of
uterine volume was 53.1% (p < 0.001). The inter-observer
variability (kappa score) for uterus and dominant fibroid
volume reductions were 0.64 and 0.60, respectively.
Table 3. Magnetic resonance imaging findings at baseline and at
6 months after uterine artery embolisation.
There was one case of fibroid expulsion after UAE,
which was known to be a risk because of the fibroid’s
submucosal location. For that particular patient, the
percentage reduction volume of fibroid was considered
as 100%.
DISCUSSION
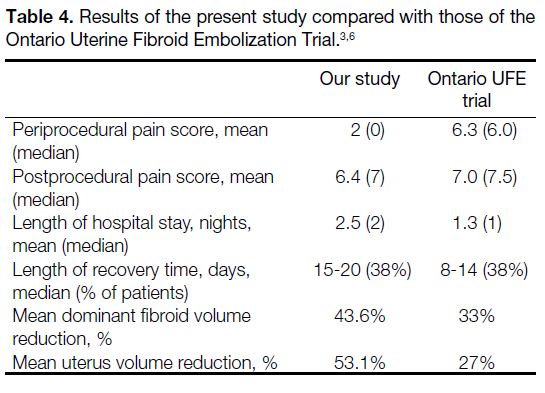
The Ontario Uterine Fibroid Embolization (UFE)
Trial[3] used periprocedural conscious sedation given by
radiologists and postprocedural PCA for pain control.
Compared with our study, the Ontario UFE trial used
similar questionnaire parameters and a similar pain
scale (NRS) for periprocedural and postprocedural pain
assessment. We compared our patient-reported pain
results with those of the Ontario UFE trial.
In terms of periprocedural pain control, our MAC
approach yielded consistently better pain score than
the Ontario UFE trial[3] (mean score of 2 vs. 6.3). The
majority of patients in our study experienced no (58%)
or mild (15%) pain (Table 1). This may reflect that
periprocedural pain control provided by MAC is better
than that provided by conscious sedation. However, an
on-site anaesthetist also provided expertise in terms of
monitoring patients under conscious sedation.
Concerning postprocedural pain control, both our study
and the Ontario UFE trial[3] used PCA methods, which
yielded mean pain scores of 6.4 (moderate) and 7.0
(severe), respectively (Table 4). These relatively high
scores may be due to post-embolisation syndrome, the
symptoms of which include pain, nausea, vomiting,
fever, fatigue, and malaise.[4] Post-embolisation syndrome
is believed to be the primary source of postprocedural
pain for UAE. According to the study by Spencer et al,[5]
the symptoms are most severe during the first 2 to
3 hours after the procedure, in particular with pelvic
pain and cramping. Afterwards the pain will usually
subside to significantly lower level. Nevertheless, the
high postprocedural pain score from our study shows the
need for more multidisciplinary discussions to improve
our current MAC/PCA protocol.
Table 4. Results of the present study compared with those of the Ontario Uterine Fibroid Embolization Trial.[3] [6]
The mean length of hospital stay (2.5 vs. 1.3 nights)
and median recovery time (15-20 vs. 10 days) for our
study were longer than those for the Ontario UFE trial.[3]
This may be because UAE with a multidisciplinary team
is a relatively new approach in our hospital, resulting
in a conservative approach to ensure patient stability
and fitness (hemodynamically stable, symptom-free or
stable) for discharge.
Although shorter hospital stay is considered favourable,
in the Ontario UFE trial,[3] almost 12% of patients indicated
that they felt the length of hospital stay was inadequate.
This raised concern with regard to patient safety and
satisfaction, as well as clinician confidence for patient
discharge. We hope and expect the length of hospital
stay to improve and approach international standards
compared to the Ontario UFE trial in subsequent UAE
as our experience increases.
Our results show that UAE for symptomatic fibroids
results in significant uterus and fibroid volume reduction,
with mean reductions of 53.1% and 43.6%, respectively.
Our results are not inferior to those of the Ontario UFE trial,[3] which showed reductions of 27% and 33%
in uterus and dominant fibroid volume, respectively
(Table 4). Our results were consistent with previous
systematic reviews from international studies which
have shown reductions in mean uterine volume of 26%
to 59% and in dominant fibroid volume of 40% to 75%
in the first 6 months after UAE.[6] [7]
Limitations
Questionnaires were conducted after 3 months from
hospital discharge at outpatient clinic, which may have
resulted in recall bias. For surveys carried out during
hospital stay, patients may decline to give an honest
assessment if they feel that it might affect their ongoing
inpatient treatment or management. The 3-month delays
eliminate these possibilities, and allow adequate time for
assessment of length of hospital stay and return to work
after UAE.
CONCLUSION
Preliminary results of UAE with a multidisciplinary team approach are promising in terms of patient experience.
REFERENCES
1. Silberzweig JE, Powell DK, Matsumoto AH, Spies JB. Management of uterine fibroids: a focus on uterine-sparing interventional
techniques. Radiology. 2016;280:675-92. Crossref
2. Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, EK Hals, et al. Assessment of pain. Br J Anaesth.
2008;101:17-24. Crossref
3. Pron G, Mocarski E, Bennett J, Vilos G, Common A, Zaidi M, et al. Tolerance, hospital stay, and recovery after uterine artery
embolization for fibroids: the Ontario Uterine Fibroid Embolization
Trial. J Vasc Interv Radiol. 2003;14:1243-50. Crossref
4. Schirf BE, Vogelzang RL, Chrisman HB. Complications of uterine fibroid embolization. Semin Intervent Radiol. 2006;23:143-9. Crossref
5. Spencer E, Stratil P, Mizones H. Clinical and periprocedural pain management for uterine artery embolization. Semin Intervent
Radiol. 2013;30:354-63. Crossref
6. Pron G, Bennett J, Common J, Wall J, Asch M, Sniderman K, et al. The Ontario Uterine Fibroid Embolization Trial. Part 2.
Uterine fibroid reduction and symptom relief after uterine artery
embolization for fibroids. Fertil Steril. 2003;79:120-7. Crossref
7. Gupta JK, Sinha A, Lumsden MA, Hickey M. Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database
Syst Rev. 2012;(5):CD005073. Crossref