Retrievable Inferior Vena Cava Filters: A 10-Year Retrospective Analysis
ORIGINAL ARTICLE
Hong Kong J Radiol 2023 Jun;26(2):120-6 | Epub 17 May 2023
Retrievable Inferior Vena Cava Filters: A 10-Year Retrospective Analysis
R Sum, KKP Lau
Department of Radiology, Monash Medical Centre, Melbourne, Australia
Correspondence: Dr R Sum, Department of Radiology, Monash Medical Centre, Melbourne, Australia. Email: r.rm.sum@gmail.com
Submitted: 23 Feb 2021; Accepted: 2 Jul 2021.
Contributors: KKPL designed the study. RS acquired and analysed the data, and drafted the manuscript. KKPL critically revised the manuscript for important intellectual content. Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: Both authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This research was approved by the Human Research Ethics Committee of Monash Medical Centre, Melbourne, Australia (Ref No.: 76899). The patients were treated in accordance with the tenets of the Declaration of Helsinki and provided written informed consent for all treatments and procedures.
Abstract
Introduction
Inferior vena cava (IVC) filters are an effective form of venous thromboembolism prophylaxis when treatment with anticoagulation is contraindicated. In recent times, the retrievable IVC filter has gained favour in clinical practice as it circumvents the consequences of permanent filters, such as deep venous thrombosis. This study is a retrospective review of the retrievability of IVC filters since their introduction in our department.
Methods
Retrospective analysis was conducted on 118 consecutive adult patients (mean age 63.6 years) who underwent IVC filter insertion over a 10-year period. Patient data, including underlying medical condition, indication for filter insertion, number of retrievals, and filter complications, were recorded. Dwell time was calculated using Kaplan-Meier survival analysis.
Results
Among the 118 patients, the most common indication for filter insertion was bleeding due to anticoagulation therapy. Mean dwell time for IVC filters was 101.7 days. One patient died before retrieval. The overall successful retrieval rate was 89.0%. Among the 13 patients whose filters could not be retrieved, nine required lifelong anticoagulation and four were lost to follow-up. Three patients developed lower limb deep venous thrombosis due to delayed filter retrieval.
Conclusion
The majority of these filters can be retrieved successfully within the first year of insertion. Retrievable IVC filters are a feasible alternative to traditional permanent IVC filters. Complicating factors occur in a small percentage of these patients, which may prevent successful retrieval.
Key Words: Pulmonary embolism; Radiology, interventional; Vena cava filters; Venous thromboembolism; Venous thrombosis
中文摘要
可回取下腔靜脈濾器的經驗:10 年回顧性分析
R Sum、KKP Lau
簡介
當有抗凝治療禁忌時,下腔靜脈濾器是預防靜脈血栓栓塞的一種有效方法。近年來,可回取下腔靜脈濾器在臨床實踐中獲得了青睞,因為它規避了永久性過濾器的後果,例如深靜脈血栓形成。本研究回顧本部門引入可回取下腔靜脈濾器的經驗。
方法
我們對10年間接受下腔靜脈濾器置入的118名連續成年患者(平均年齡63.6歲)進行回顧性分析。本研究記錄了患者數據,包括基礎疾病、濾器置入的指徵、濾器回取次數和濾器併發症,並使用 Kaplan-Meier生存分析計算濾器置留時間。
結果
在該118名患者中,濾器置入最常見適應症為抗凝治療導致出血。下腔靜脈濾器平均置留時間為101.7天。一名患者在濾器回取前死亡。濾器回取整體成功率為89.0%。在濾器無法回取的13名患者中,9人需要終生抗凝,4人失訪。三名患者由於濾器回取延遲而出現下肢深靜脈血栓形成。
結論
大多數濾器可在置入第一年內成功回取。可回取下腔靜脈濾器是傳統永久性下腔靜脈濾器的可行替代方案。小部分患者出現併發因素,或會阻礙濾器成功回取。
INTRODUCTION
The use of inferior vena cava (IVC) filters to prevent
venous thromboembolism (VTE) is a proven and
effective treatment for patients with a contraindication
to standard anticoagulation therapy or refractory
VTE that has failed anticoagulation.[1] There have been
significant developments in IVC filters over recent
years. Permanent IVC filters were first introduced into
clinical practice over 30 years ago — these remain inside
the patient for life. However, evidence in the current
literature demonstrates that the rate of complications
increases with extended dwell times of IVC filters.[2] [3]
These complications can have significant detrimental
clinical implications, including filter thrombosis and
an increased risk of developing subsequent deep
venous thrombosis (DVT) which may require lifelong
anticoagulation.[3] For this reason, the retrievable filter
was developed as an attractive alternative that avoids
the long-term implications of permanent filters while
still being able to provide protection against VTE in the
relevant setting. However, retrievable filters are also
subject to a series of complicating factors that can prevent
their successful removal. Certain filter elements such
as the hook, struts, and barbs are prone to endothelial
overgrowth. Misalignment, migration, and fractures
are also commonly encountered issues.[4] Retrieval can
be delayed be trapped emboli within the filter itself.[5]
According to the current literature, the incidence rates of these complications can vary significantly between
institutions.[4]
Because the risk of VTE requires individual assessment
and the intention of filtration is to prevent pulmonary
embolism (PE), discontinuation is recommended as soon
as the perceived risk of developing clinically significant
PE is acceptably low.[2] There is no consensus on the
recommended duration for filter dwell time. This study
is a retrospective review of the retrievability of an IVC
filter (Celect Platinum; Cook Medical, Bjaeverskov,
Denmark) since its introduction in our department more
than a decade ago.
METHODS
We reviewed 118 consecutive cases of adult patients
who underwent IVC filter insertion and retrieval at a
tertiary referral centre between 1 January 2008 and
1 August 2018. We excluded eight other patients as their
IVC filters were inserted external to our institution. One
patient died before any attempt at retrieval was feasible
and this patient was excluded from data analysis.
Patients’ age, sex, underlying medical conditions, and
indications for IVC filter insertion were recorded. Details
of the insertion, including approach and dates, were
noted. Details of subsequent retrieval attempts including
the date, number of attempts, reasons for failure (if any),
and complications were also recorded.
Filter insertion was undertaken either through a right
jugular or right or left femoral venous puncture approach.
The IVC filter was chosen for insertion through a 7-Fr
introducer sheath. A cavagram was routinely performed
after deployment to confirm its position.
As part of our department’s filter retrieval procedure, an initial cavagram was performed through a right internal
jugular venous puncture to exclude filter thrombus
and other complicating factors. Filter retrieval was
performed using a retrieval set (Günther Tulip; Cook
Medical, Bjaeverskov, Denmark) through a right internal
jugular venous approach. An 11-F introducer sheath was
used for venous access. A 6.3-F retrieval loop system
using the loop-snare technique was used to engage the
filter hook. Kaplan-Meier analysis comparing successful
and unsuccessful retrieval was performed with SPSS
(Windows version 24.0; IBM Corp, Armonk [NY],
United States). Statistical significance was calculated
using Fisher’s exact test. A p value of < 0.05 was
considered to be statistically significant.
This study was prepared in accordance with STROBE
(Strengthening the Reporting of Observational Studies
in Epidemiology) reporting guidelines. Ethics approval
in accordance with the National Health and Medical
Research Council of Australia was obtained from the
Human Research Ethics Committee of Monash Medical
Centre, Melbourne, Australia.
RESULTS
Patient Demographics
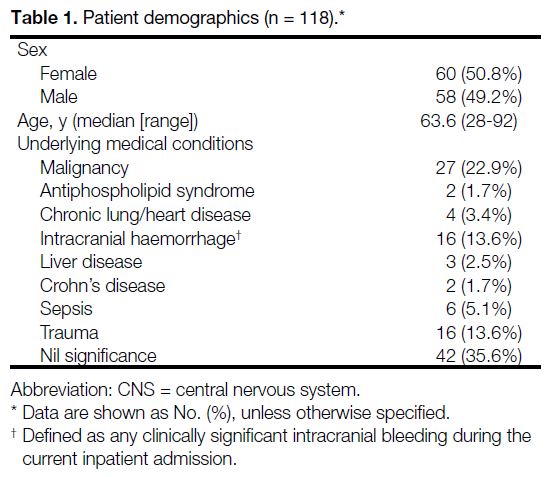
Most patients had had an underlying medical condition
predisposing them to developing VTE (64.4%). The most
common underlying condition was malignancy (22.9%),
followed by intracranial haemorrhage (13.6%), trauma
(13.6%), sepsis (5.1%), chronic heart and lung disease
(3.4%), liver disease (2.5%), and antiphospholipid
syndrome (1.7%) [Table 1].
Table 1. Patient demographics (n = 118).
Indications for Inferior Vena Cava Filter
Insertion
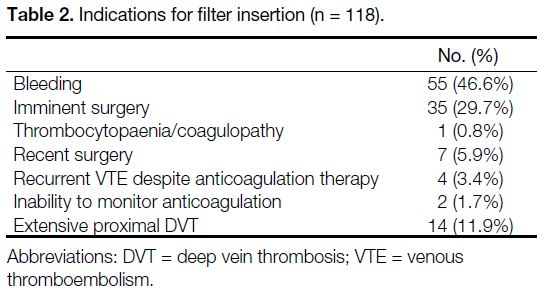
Consultation and approval by our institution’s
haematology unit was required prior to filter insertion.
In all, 118 patients required IVC filters because
anticoagulation was contraindicated. The most
common reason for filter insertion was bleeding due to
anticoagulation (46.6%), followed by imminent surgery
(29.7%), extensive proximal DVT (11.9%), recent
surgery (5.9%), recurrent VTE despite anticoagulation
(3.4%), inability to monitor anticoagulation (1.7%), and thrombocytopaenia/coagulopathy (0.9%) [Table 2].
Table 2. Indications for filter insertion (n = 118).
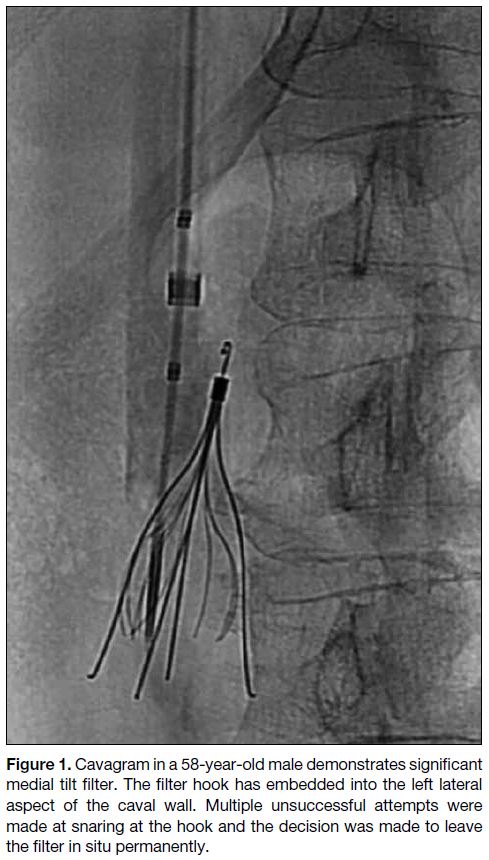
There were 79 filters inserted through a femoral approach
and 39 inserted through a jugular approach. A total of
117 filters were successfully inserted without immediate
complications. One filter demonstrated tilt immediately
after being deployed but no attempts were made to
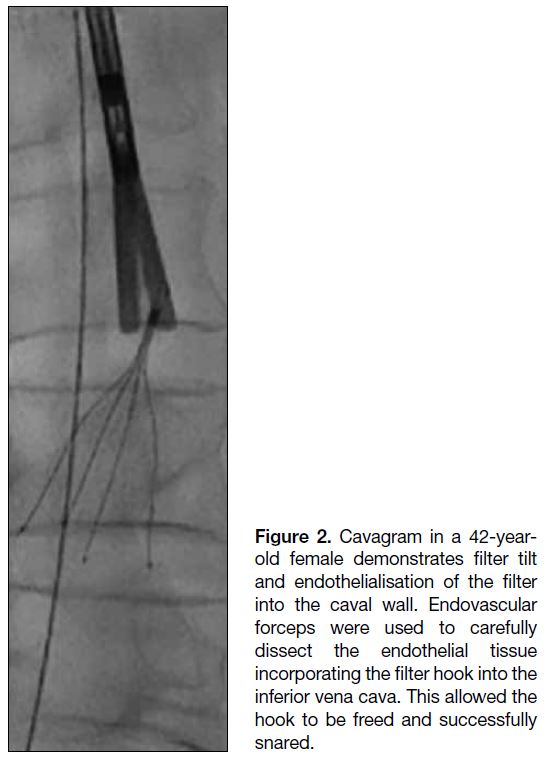
reposition it thereafter (Figure 1).
Figure 1. Cavagram in a 58-year-old male demonstrates significant
medial tilt filter. The filter hook has embedded into the left lateral
aspect of the caval wall. Multiple unsuccessful attempts were
made at snaring at the hook and the decision was made to leave
the filter in situ permanently.
In all successful retrievals, there were no immediate
complications identified on routine post-retrieval
cavagram. All retrievals were attempted through a right
jugular approach.
Rates of Inferior Vena Cava Filter Retrieval
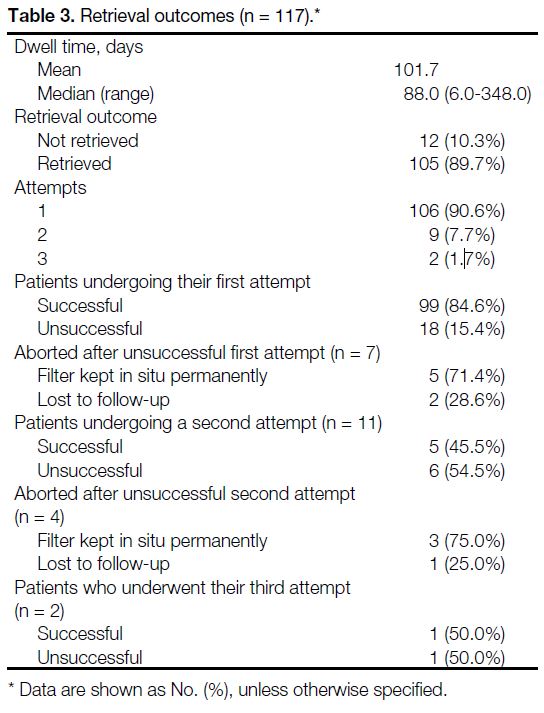
The indwelling time for filters was calculated using
Kaplan-Meier product limit estimation (median = 88.0
days; range, 6.0-348.0). Out of the 117 retrieval attempts,
105 were successful (90.0%) with six of these 105 filters requiring more than one attempt (5.7%) [Table 3]. Thirteen filters could not be retrieved (11.1%); their reasons are outlined below. A single retrieval attempt was
conducted in 106 patients. Two attempts were performed
in nine patients. Two patients underwent three retrieval
attempts [Table 3].
Table 3. Retrieval outcomes (n = 117).
During the first attempt, 99 filters were successfully
retrieved (84.6%) while 18 filters could not be removed
(15.4%). The barriers to retrieval in these 18 filters
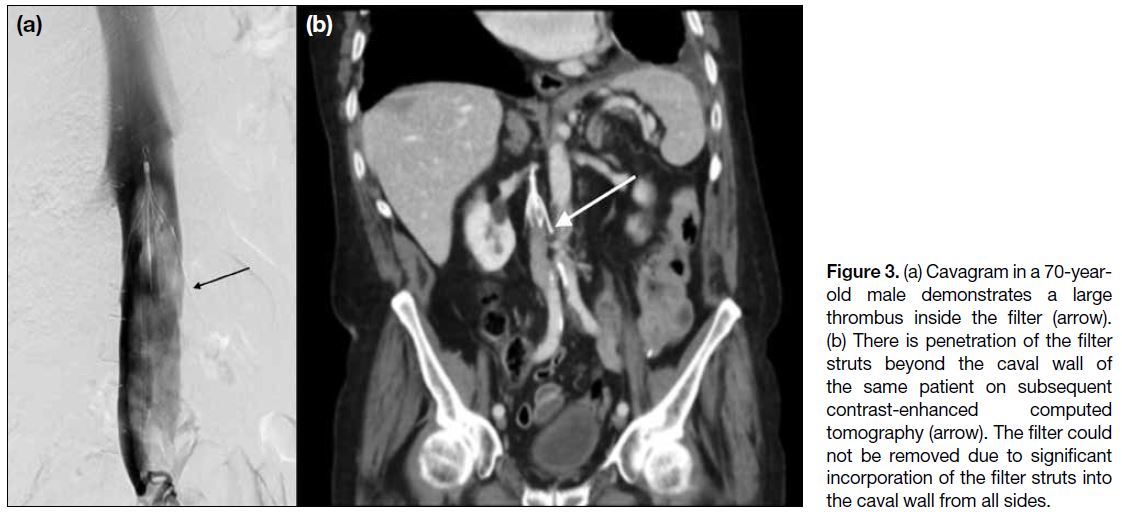
were endothelialisation of the filter hook in six patients
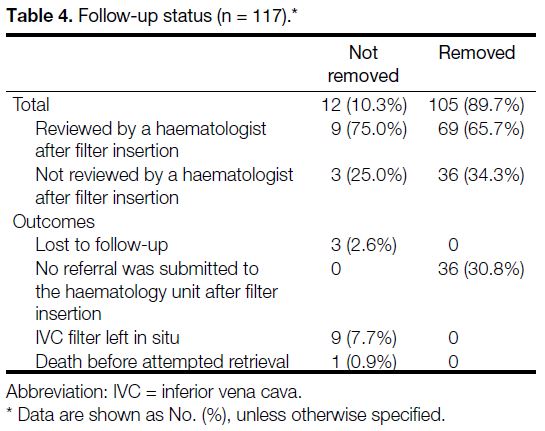
(33.3%) [Figure 2], a large trapped thrombus in another
six patients (33.3%) [Figure 3], thrombus formation
around the filter hook in four patients (22.2%), and
protrusion of the filter legs beyond the caval wall in two
patients (11.1%) [Figure 3]. A second attempt was not
performed in seven of these patients; in five, retrieval of the filter was deemed technically too difficult. The
clinical haematology unit decided to keep them as
permanent filters and these patients were started on long-term
anticoagulation with warfarin. The remaining two
patients were lost to follow-up (Table 3).
Figure 2. Cavagram in a 42-year-old female demonstrates filter tilt and endothelialisation of the filter into the caval wall. Endovascular forceps were used to carefully dissect the endothelial tissue incorporating the filter hook into the inferior vena cava. This allowed the hook to be freed and successfully snared.
Figure 3. (a) Cavagram in a 70-year-old male demonstrates a large thrombus inside the filter (arrow). (b) There is penetration of the filter struts beyond the caval wall of the same patient on subsequent contrast-enhanced computed tomography (arrow). The filter could not be removed due to significant incorporation of the filter struts into the caval wall from all sides.
Of the 18 patients who failed first retrieval attempts, 11
underwent a second attempt while two of them had a
third attempt. Nine patients underwent a second attempt
only and the other two patients underwent three attempts
each. Among 11 patients who had the second retrieval
attempt, five were successfully removed (45.5%) and
six were not (54.5%). The reasons for a second failed
retrieval were an inability to snare due to thrombus
surrounding the filter hook (n = 3), filter thrombus
(n = 2), and protrusion of the filter legs beyond the
caval wall (n = 1). From these six unsuccessful second
retrieval attempts, three filters were kept permanently
and the patients were commenced on warfarin therapy.
One patient was lost to follow-up (Table 3).
In the two remaining patients who failed the second
retrieval attempt, a third retrieval attempt was
performed. One was successfully retrieved after a period
of anticoagulation for filter hook thrombus in addition to
the use of a loop wire snare to engage the filter hook. The
other retrieval was unsuccessful despite a third attempt
and the decision was made by the clinical haematology
unit to keep this as a permanent filter. The patient was subsequently commenced on long-term warfarin therapy
(Table 3).
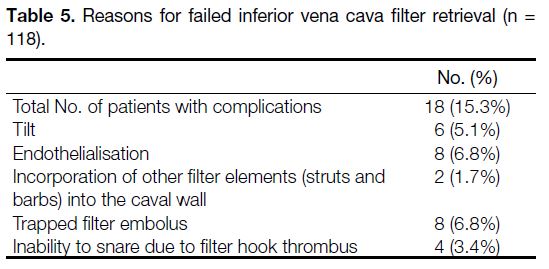
Rates of Follow-up
From the total cohort of 105 successful retrievals, 69 of
these patients (65.7%) were reviewed by haematology
while 36 patients (34.3%) were not. Among the 12
unsuccessful retrievals, nine patients were commenced
on anticoagulation and were managed by a haematologist
and three were lost to follow-up (Table 4).
Table 4. Follow-up status (n = 117).
Reasons for Failed Filter Retrieval
There were several factors complicating successful
filter retrieval (Table 5). Eighteen patients had had
complications with their filter at the time of attempted
retrieval (15.3%) with some patients having more than
one concurrent complication. Two of the most prevalent
factors were trapped embolus within the filter (n = 8) and
endothelialisation of the filter hook into the caval wall
(n = 8). Filter tilt was seen in six patients. In four patients,
the filter hook could not be snared despite multiple
attempts at passing the retrieval wire, presumably due to
the presence of thrombus surrounding the hook. There
were two filters where elements other than the hook
(such as the struts) were incorporated into the caval wall.
In one patient, there was a combination of filter tilt and
endothelialisation of the hook, which led to failure of
retrieval (Figure 1). No subsequent attempts at retrieval
were made for this patient.
Table 5. Reasons for failed inferior vena cava filter retrieval (n = 118).
In all cases where retrieval could not be performed due to
a trapped embolus, a period of therapeutic low molecular
weight heparin was commenced by the haematology
unit for 3 months to reduce the thromboembolic load
before further attempts at retrieval were considered. This
occurred in four filters, three of which were thereafter
successfully removed on the second attempt.
One patient had filter tilt and endothelialisation of the
hook into the left side of the caval wall. After multiple
attempts at manipulating the hook using a variety of
snares and balloon insufflation to correct the tilt, the filter
tip was eventually freed through blunt dissection of the
hook from the caval wall using endovascular forceps and
removed without immediate complications (Figure 2).
Three patients developed bilateral lower limb DVT as
a result of prolonged dwell time of the IVC filter and
multiple non-retrieval attempts, requiring a period of
anticoagulation before successful retrieval.
DISCUSSION
This retrospective study provides insight into the
management of retrievable IVC filters at our institution.
Specifically, the data confirm a high retrieval
performance in our department with 105 retrieved
(89.0%) successfully from a total of 118 filters inserted
over the 10-year study period.
A review of the current literature demonstrates that
retrieval rates elsewhere are highly variable, ranging
from 49.6% to as high as 96.6%.[6] [7] [8] [9] Nearly 60.0% of
our IVC filter retrievals occurred within the first 100
days of insertion with the final retrieval rate of 89.0%
achieved by 350 days after insertion. Previous studies
reveal that the retrieval of Celect filters is most likely to
be successful within 3 to 4 months of placement which is
also in keeping with our results.[10]
Currently, there is no well-documented consensus on a
safe dwell time for retrievable filters. It is recommended
that filters should be removed as soon as the risk of PE
has resolved due to the risk of complications, although
others have suggested that removal times be guided by
manufacturers’ guidelines.[11] Further, additional delays
in retrieval can occur, especially if there are unforeseen
changes in the patient’s clinical trajectory during their
admission or follow-up.
Prolonged dwell times can be problematic and result in
a variety of complications as evidenced in our study.
Analyses have shown retrievable IVC filters to have an
overall complication rate ranging from 11.7% to 20.0%,
which is also consistent with our findings (15.3%).[6] [7] For
instance, strut penetration is reported at a higher rate
among conical filters such as the Celect filter.[12] [13] [14] [15] While
penetration is common among Celect filters, it is rarely
associated with breakthrough PE, retrieval failure, or
other local complications.[16] An example is seen in one
patient where retrieval could not be performed on two
attempts due to extensive trapped thrombus within the
filter and strut penetration (Figure 3). The third attempt
on the same patient was complicated by filter tilt and
hook embedment into the posterior caval wall that
prevented successful snaring.
The inherent morbidity implicated by long-term filter
implantation should not be dismissed. In the PREPIC
(Prevention of Recurrent Pulmonary Embolism by Vena
Cava Interruption) trial, permanent IVC filters were
associated with increased odds of developing recurrent DVT and a reliance on long-term anticoagulation.[3] [17]
This outcome was seen in seven patients who underwent
failed retrieval attempts and were subsequently subjected
to lifelong warfarin. Short-term anticoagulation therapy
was also required for three patients who experienced
delays in filter retrieval and subsequently developed new
lower limb DVT.
Currently, IVC filter insertion at our institution requires
formal approval from the haematology unit prior to the
procedure. However, there is no protocol for follow-up
after their insertion. As a result, three patients were lost
to follow-up and no clear anticoagulation plan or plan
for filter removal was documented in their medical
records. Delays in filter retrieval result in prolonged
dwell times, which are detrimental from the increased
risk of developing DVT and, in some cases, may subject
patients to lifelong anticoagulation. A dedicated follow-up
system is therefore required so that all patients
undergoing IVC filter insertion are monitored by both
interventional radiologists and haematologists to ensure
appropriate filter retrieval timing and the optimal use of
anticoagulation therapy.
Limitations
This study was from a single tertiary radiology centre,
which was its major limitation. Another limitation was
the lack of direct contact with those patients who were
not followed up by the haematology unit.
CONCLUSION
Retrievable IVC filters are a feasible and safe alternative
to permanent filters in VTE prevention. Our study
demonstrates that a high retrieval rate can be achieved
within 1 year of insertion. However, it is important
to be aware that a small percentage of filters may be
complicated by several factors that may warrant the use
of advanced retrieval techniques. Prompt removal of
the IVC filter when safe to do so is necessary due to the
increased risk of developing DVT.
REFERENCES
1. Kaufman JA, Barnes GD, Chaer RA, Cuschieri J, Eberhardt RT, Johnson MS, et al. Society of Interventional Radiology clinical
practice guideline for inferior vena cava filters in the treatment
of patients with venous thromboembolic disease: developed in
collaboration with the American College of Cardiology, American
College of Chest Physicians, American College of Surgeons
Committee on Trauma, American Heart Association, Society for
Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv
Radiol. 2020;31:1529-44. Crossref
2. Kaufman JA, Kinney TB, Streiff MB, Sing RF, Proctor MC, Becker D, et al. Guidelines for the use of retrievable and convertible vena cava filters: Report from the Society of Interventional
Radiology Multidisciplinary Consensus Conference. World J Surg.
2007;31:251-64. Crossref
3. Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein
thrombosis. Prévention du Risque d’Embolie Pulmonaire par
Interruption Cave Study Group. N Engl J Med. 1998;338:409-15. Crossref
4. Deso SE, Idakoji I, Kuo WT. Evidence-based evaluation of inferior vena cava filter complications based on filter type. Semin Intervent Radiol. 2016;33:93-100. Crossref
5. Al-Hakim R, Kee ST, Olinger K, Lee EW, Moriarty JM, McWilliams JP. Inferior vena cava filter retrieval: effectiveness and complications of routine and advanced techniques. J Vasc Interv
Radiol. 2014;25:933-9 Crossref
6. Doody O, Given MF, Kavnoudias H, Street M, Thomson KR, Lyon SM. Initial experience in 115 patients with the retrievable
Cook Celect vena cava filter. J Med Imaging Radiat Oncol.
2009;53:64-8. Crossref
7. Lyon SM, Riojas GE, Uberoi R, Patel J, Lipp ME, Plant GR, et al. Short- and long-term retrievability of the Celect vena cava filter: results from a multi-institutional registry. J Vasc Interv Radiol. 2009;20:1441-8. Crossref
8. Tashbayev A, Belenky A, Litvin S, Knizhnik M, Bachar GN, Atar E. Retrievable inferior vena cava filters: indications, indwelling time, removal, success and complication rates. Isr Med Assoc J.
2016;18:104-7.
9. Lynch FC. A method for following patients with retrievable inferior vena cava filters: results and lessons learned from the first 1,100 patients. J Vasc Interv Radiol. 2011;22:1507-12. Crossref
10. Glocker RJ, Novak Z, Matthews TC, Patterson MA, Jordan WD, Pearce BJ, et al. Factors affecting Cook Günther Tulip and Cook
Celect inferior vena cava filter retrieval success. J Vasc Surg Venous
Lymphat Disord. 2014;2:21-5. Crossref
11. Sarosiek S, Crowther M, Sloan JM. Indications, complications, and management of inferior vena cava filters: the experience in 952 patients at an academic hospital with a level I trauma center. JAMA Inter Med. 2013;173:513-7. Crossref
12. Zhou D, Spain J, Moon E, Mclennan G, Sands MJ, Wang W. Retrospective review of 120 Celect inferior vena cava filter
retrievals: experience at a single institution. J Vasc Interv Radiol.
2012;23:1557-63. Crossref
13. Andreoli JM, Lewandowski RJ, Vogelzang RL, Ryu RK. Comparison of complication rates associated with permanent and
retrievable inferior vena cava filters: a review of the MAUDE
database. J Vasc Interv Radiol. 2014;25:1181-5. Crossref
14. McLoney ED, Krishnasamy VP, Castle JC, Yang X, Guy G. Complications of Celect, Günther Tulip, and Greenfield inferior
vena cava filters on CT follow-up: a single-institution experience.
J Vasc Interv Radiol. 2013;24:1723-9. Crossref
15. Wang SL, Siddiqui A, Rosenthal E. Long-term complications of inferior vena cava filters. J Vasc Surg Venous Lymphat Disord. 2017;5:33-41. Crossref
16. Bos A, Van Ha T, van Beek D, Ginsburg M, Zangan S, Navuluri R, et al. Strut penetration: local complications, breakthrough pulmonary embolism, and retrieval failure in patients with celect
vena cava filters. J Vasc Interv Radiol. 2015;26:101-6. Crossref
17. Bauer KA. Duration of anticoagulation: applying the guidelines and beyond. Haematology Am Soc Hematol Educ Program. 2010;2010:210-5. Crossref