Young Adult Hip Dysplasia: An Important and Under-recognised Clinical Cause of Hip Pain on Plain Radiographs
ORIGINAL ARTICLE
Young Adult Hip Dysplasia: An Important and Under-recognised Clinical Cause of Hip Pain on Plain Radiographs
SK Wong, KH Tse, NY Pan
Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong
Correspondence: Dr SK Wong, Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong. Email: wkh731@ha.org.hk
Submitted: 26 Apr 2018; Accepted: 6 Aug 2018.
Contributors: All authors designed the study, acquired and analysed the data, drafted the manuscript, and had critical revision of the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: This research was approved by the Kowloon West Cluster Research Ethics Committee (Ref KW/EX-18-071(123-10)).
Abstract
Objective
Hip pain is the main indication for hip radiographs, which comprise a significant proportion of outpatient radiograph examinations. Our objective was to identify the level of commonality of hip dysplasia among patients with hip pain in our institution.
Methods
All hip and pelvic radiographs with reports including keywords “hip pain” during the period from December 2016 to November 2017 were reviewed. The lateral centre-edge angle and the Tonnis angle were used for reference. Severity of positive findings was also graded. Interpretations of radiographs were made by three musculoskeletal radiologists followed by calculation of its incidence.
Results
A total of 145 pelvic radiographs from 145 patients were included for analysis. Radiographs of 25 out of 145 (17.2%) patients revealed the presence of hip dysplasia.
Conclusion
Young adult hip dysplasia is a common cause of hip pain.
Key Word: Hip dislocation
中文摘要
年輕人髖臼發育不良:一個重要但在X光片上被忽視的髖關節疼痛成因
黃家漢、謝家熙、潘寧遠
引言
髖部疼痛是髖部X光片的主要適應症,佔門診X光片檢查很大比例。本研究旨在評估本院中髖臼發育不良在有髖關節疼痛病人中的發生率。
方法
回顧所有於2016年12月至2017年11月期間於本院因髖關節疼痛照髖關節或盤骨X光片的病人。X光片由3名骨骼放射科醫生進行閱片,用側中心邊角(lateral centre-edge angle)及Tonnis角作指標,並對其嚴重性作評估。
結果
共145名患者攝了髖部X光片。其中25人(17.2%)被發現患有髖臼發育不良。
結論
年輕人髖臼發育不良是髖關節疼痛其中一個常見的成因。
INTRODUCTION
Hip pain is the main indication for hip radiographs, which comprise a significant proportion of outpatient radiograph examinations. Acetabular dysplasia is a common but often under-recognised finding in patients presenting with non-traumatic hip pain, especially in the young adult age-group (<60 years). Patients may present with pain before secondary osteoarthritis develops; thus, it is important to recognise this disease entity to enable timely intervention before irreversible damage occurs.
A true frontal pelvic radiograph is required to diagnose hip dysplasia. Two of the most widely used measurements are the lateral centre-edge angle and the Tonnis angle, both of which have high inter-observer reliability.[1]
Treatment options are available for adults with hip dysplasia with the main aim of prevention of premature osteoarthritis.[2] Therefore, it is important to raise clinical suspicion of this disease entity among radiologists to enable timely diagnosis and intervention.
This study aimed to assess the incidence of young adults with hip dysplasia in the local population who are referred for hip radiography.
METHODS
Our local hospital’s radiology database was accessed via the RIS3 system using the free-text search function. All hip and pelvic radiographs with reports including the keywords “hip pain” during the period from December 2016 to November 2017 were retrieved. Patients aged <18 years, >60 years, or with a history of hip surgery and fracture were excluded. Patients who only received localised radiographic views of either hip with no concomitant anteroposterior pelvic radiograph and those without a true frontal pelvic radiograph were also excluded.
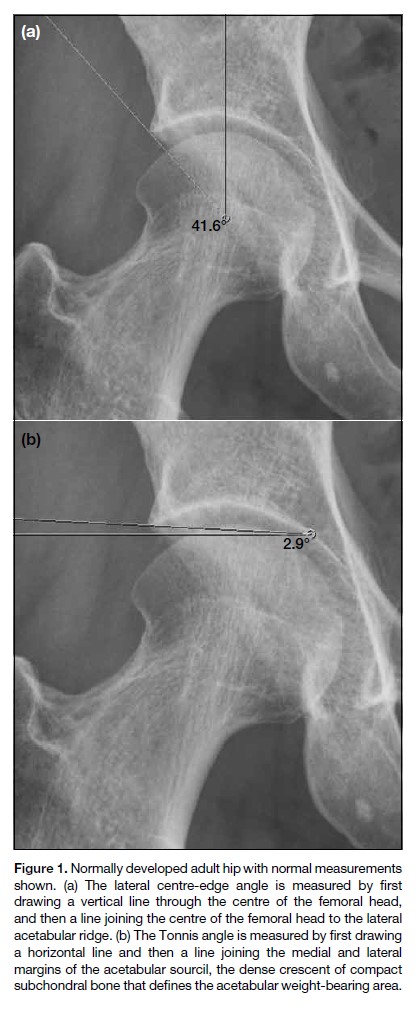
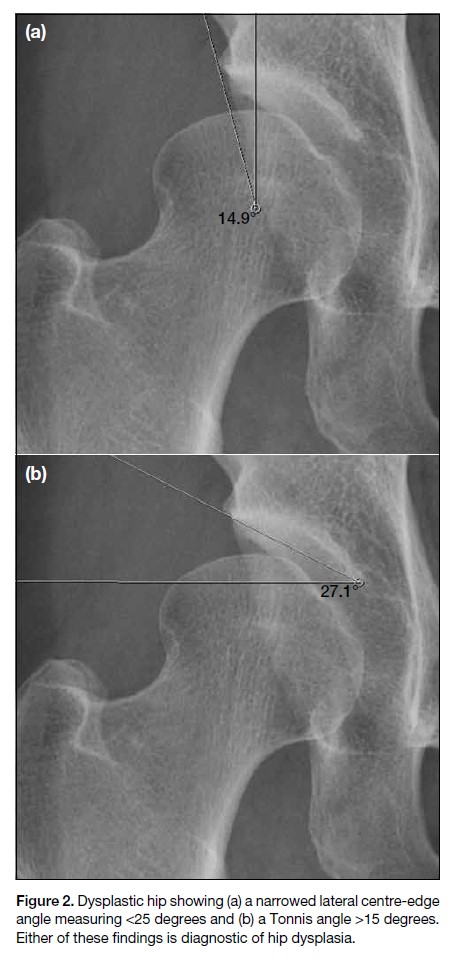
Quantitative measurements were made using true anteroposterior radiographs of the pelvis. A true frontal pelvic radiograph should not have excessive craniocaudal tilt and is defined as acceptable if the distance between the coccyx and symphysis pubis is <3 cm. The lateral centre-edge angle is the angle between a vertical line through the centre of the femoral head and a line drawn from the centre of the femoral head to the acetabular ridge (Figure 1a). The Tonnis angle is the angle between a horizontal line and a line joining the medial and lateral margins of the acetabular sourcil (Figure 1b). The positive finding of either a lateral centre-edge angle of <25 degrees or a Tonnis angle of >15 degrees is regarded as abnormal and diagnostic of acetabular dysplasia (Figure 2).[3] The severity of positive findings is also categorised into grade I to grade IV according to Crowe classification.
Figure 1. Normally developed adult hip with normal measurements shown. (a) The lateral centre-edge angle is measured by first drawing a vertical line through the centre of the femoral head, and then a line joining the centre of the femoral head to the lateral acetabular ridge. (b) The Tonnis angle is measured by first drawing a horizontal line and then a line joining the medial and lateral margins of the acetabular sourcil, the dense crescent of compact subchondral bone that defines the acetabular weight-bearing area.
Figure 2. Dysplastic hip showing (a) a narrowed lateral centre-edge angle measuring <25 degrees and (b) a Tonnis angle >15 degrees. Either of these findings is diagnostic of hip dysplasia.
Interpretations of radiographs were made by three musculoskeletal radiologists with 10 years, 8 years and 6 years of experience, respectively in interpreting musculoskeletal radiographs. The three radiologists were blinded to clinical history apart from the indication of hip pain. The initial interpretation was made independently by each radiologist. Disagreement was resolved by consensus.
RESULTS
A total of 145 pelvic radiographs from 145 patients were retrieved after applying the inclusion and exclusion criteria. Minor discrepancies among the three radiologists regarding the measurements were found in 16 out of 145 (11%) radiographs, and they were all resolved by consensus. The radiographs of 25 out of 145 (17.2%) patients revealed the presence of hip dysplasia. Of them, 24 (96%) were Chinese and one (4%) was from South Asia, 17 (68%) were women, and eight (32%) were men. Bilateral hip involvement was observed in 15 (60%) of patients; the remaining 10 (40%) had unilateral involvement. All of the patients with hip dysplasia were classified as grade I according to Crowe classification, which is the least severe type. None of them had complications such as fracture or advanced degeneration as evidenced by visual assessment of significant joint space narrowing and osteophytes.
DISCUSSION
Adult hip dysplasia describes undercoverage of the acetabulum, which is an important cause of hip pain. It is also one of the most important contributors to premature hip osteoarthritis.[4]
The risk factors for developmental hip dysplasia include female sex, primiparity, breech position, and a positive family history of hip dysplasia.[5,6] However, not all adult hip dysplasia is due to developmental hip dysplasia, and they may be different disease entities.[7] A concave acetabulum cannot develop properly in the absence of normal concentric force from the femoral head. Therefore, conditions such as cerebral palsy, hereditary motor and sensory neuropathy, poliomyelitis, and hyperlaxity can all cause abnormal acetabular coverage.[8] Lateral acetabular growth may also be affected by growth of triradiate cartilage due to skeletal dysplasia, Perthes disease, and proximal femoral focal deficiency.[8]
An underdeveloped and shallow acetabulum induces compensatory hypertrophy of the labrum to improve acetabular coverage. Therefore, symptoms may be masked initially and only present in late adulthood. When stress increases and exceeds its limit, labral tears and stress fractures of the acetabular rim may occur. Acetabular dysplasia is also associated with proximal femoral abnormalities, including asymmetrical femoral head, increased anteversion, and valgus deformity.[9] Eventually, with disturbance of the hip joint’s normal weight bearing mechanisms, secondary osteoarthritis develops.
Patients with hip dysplasia usually present with insidious groin pain, which usually worsens with activity.[10] Physical examination demonstrates limping gait and signs of positive impingement, but the joint itself may have a normal range of movement. Its overall clinical picture simulates femoral acetabular impingement and therefore may cause diagnostic confusion unless radiographs are carefully evaluated.
An anteroposterior pelvic radiograph remains the mainstay of initial investigation of hip dysplasia. Multiple radiographic measurements of hip dysplasia are available, including the lateral centre-edge angle, the Tonnis angle, anterior centre-edge angle, femoral headneck- shaft angle, and fovea capitis position. The lateral centre-edge and Tonnis angles were selected for this study because they are two of the most commonly used and most easily measured quantities on frontal pelvic radiographs. Moreover, as acetabular undercoverage and underdevelopment are considered as the hallmarks of hip dysplasia, primary importance was placed on diagnostic measurements of the acetabulum rather than measurements of the femur, i.e. femoral head-neck-shaft angle and fovea capitis position. The anterior centreedge angle is another measurement used to diagnose hip dysplasia with good inter-observer reliability. It measures anterior acetabular coverage but requires a false profile radiograph, which is not routinely performed in our institution. Computed tomography scan of the hip enables a three-dimensional assessment of the severity of acetabular dysplasia and bone deficiency and is thus beneficial for preoperative planning. However, due to radiation dose concerns, the role of computed tomography has been partially replaced by magnetic resonance imaging (MRI). Additional information about the status of soft tissues such as the labrum and articular cartilage is provided by MRI. The addition of arthrogram to MRI would further increase its sensitivity in identifying labral tears.[11]
Treatment of hip dysplasia depends on symptom severity. Hip arthroscopy can be an option for early and mild dysplasia, and it may provide short-term pain control.[12] However, evidence has been limited, and some case reports have also suggested that without correcting the underlying pathology, labral surgery may increase instability and lead to further progression of symptoms.[13] Corrective surgeries such as pelvic osteotomies with or without femoral osteotomy are more evidence-based and decrease the rate of developing osteoarthritis with correction of the underlying acetabular undercoverage hip joint malalignment. Total hip arthroplasty is a more definitive treatment option, but preoperative imaging is mandatory, and the treatment is generally reserved for patients with advanced secondary osteoarthritis or after previously failed corrective osteotomies.
Our study has shown that in our institution, adult hip dysplasia is a common disease entity in patients with hip pain.
The prevalence of hip dysplasia reported in the literature ranges from 4% to 12%,[14,15] which is slightly lower than that in our study population (17.2%). This may be accountable to a few reasons. First, different studies have used different cut-offs for the diagnosis of hip dysplasia. Moreover, our study focused on patients presenting symptoms of hip pain rather than the general asymptomatic population. Finally, because our study focused on patients with hip pain rather than the general population, incidence (rather than prevalence) was calculated.
Our study has several limitations. As mentioned above, the detected incidence of hip dysplasia may not reflect its actual prevalence in our local population. Further studies with larger sample sizes and inclusion of those who are completely asymptomatic is warranted. Second, as this is a retrospective study, physical examinations including relevant impingement and range of motion tests were often not performed or recorded at the time of clinical assessment. Moreover, the source of referral was not limited to orthopaedic surgeons and included other clinical specialties such as family medicine and internal medicine, the practitioners in some of which may not be familiar with diagnosing hip dysplasia and may be unable to suggest the possibility of this diagnosis on the request form.
In summary, our study findings illustrate a relatively high incidence of adult hip dysplasia among patients who presented with hip pain. Radiographic diagnosis of adult hip dysplasia is objective and simple, with readily applicable measurement methods that can be obtained in frontal pelvic radiographs. It is anticipated that early diagnosis of such disease entity facilitated by increased awareness could facilitate the provision of timely treatment regimes to yield better clinical outcomes.
REFERENCES
1. Nelitz M, Guenther KP, Gunkel S, Puhl W. Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol. 1999;72:331-4. Crossref