Inverted Meckel’s Diverticulum — A Rare Complication of a Common Congenital Anomaly: A Case Report
CASE REPORT
Inverted Meckel’s Diverticulum — A Rare Complication of a
Common Congenital Anomaly: A Case Report
KKF Fung1; JHF Chiu2; KK Cheng1
1 Department of Diagnostic and Interventional Radiology, Kwong Wah Hospital, Yaumatei, Hong Kong
2 Department of Surgery, Kwong Wah Hospital, Yaumatei, Hong Kong
Correspondence: Dr KKF Fung, Department of Diagnostic and Interventional Radiology, Kwong Wah Hospital, Yaumatei, Hong Kong. Email: gwevin@gmail.com
Submitted: 15 Jul 2018; Accepted: 10 Aug 2018.
Contributors: All authors contributed to the concept of study, acquisition and analysis of data, drafting of the manuscript, and had critical revision of the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: Informed consent was obtained from the patient. The study was conducted in accordance with the Declaration of Helsinki
INTRODUCTION
Meckel’s diverticulum is the most common congenital
anomaly of the gastrointestinal tract and found in
approximately 2% of the population. Most Meckel’s
diverticula remain clinically silent with an estimated
lifetime risk of complications reported to be about
4% to 40%.[1] Inversion of Meckel’s diverticulum is a
rare phenomenon that occurs when the diverticulum
invaginates upon itself into the lumen of the terminal
ileum. This can be further complicated by small bowel
haemorrhage and intussusception, where the inverted
diverticulum acts as a lead point.[2] We describe a case
of inverted Meckel’s diverticulum presenting with acute
small bowel haemorrhage.
CASE REPORT
A 43-year-old man presented with a 2-week history
of recurrent central abdominal pain and an episode of
haematochezia. On admission, he was clinically stable
and clinical examination did not reveal any mass or
tenderness in the abdomen. Per rectal examination found
a trace amount of fresh blood. However, six episodes of
massive fresh per rectal bleeding developed subsequently
with a witnessed episode of syncope. Haemoglobin dropped from 94 g/L on admission to 63 g/L and urgent
oesophagogastroduodenoscopy and colonoscopy were
performed. No obvious source of bleeding could be
identified although a large amount of old blood product
was seen in the terminal ileum on colonoscopy, raising a
suspicion of small bowel haemorrhage.
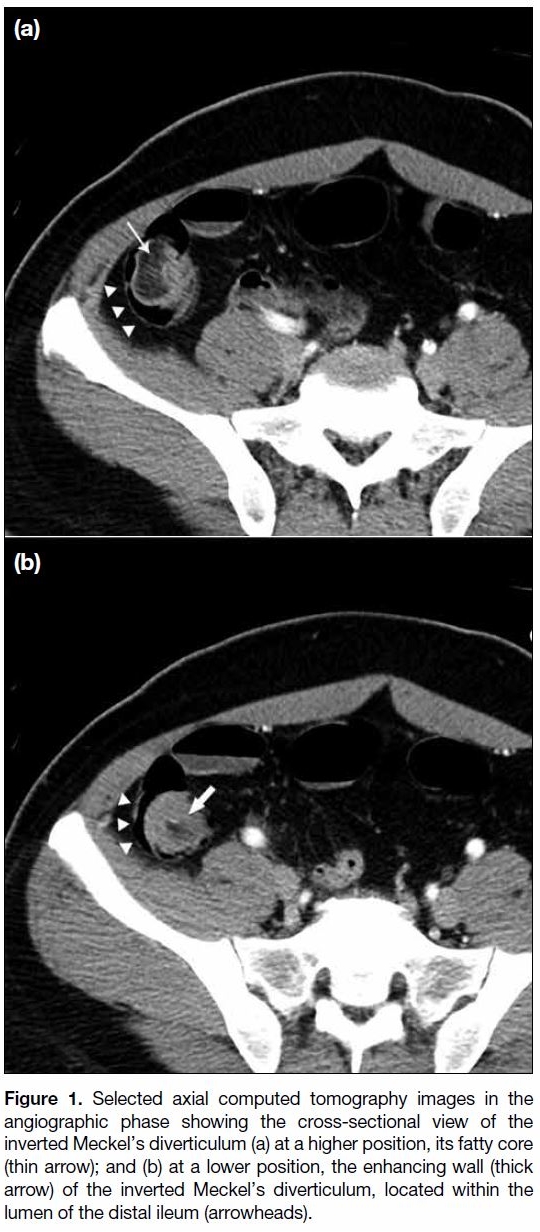
Computed tomographic angiography of the abdomen and
pelvis was arranged and revealed an elongated tubular
fat-containing lesion within the lumen of the distal ileum,
about 60 cm from the ileocaecal junction. The lesion
contained a central fatty core surrounded by a collar of
enhancing soft tissue (Figure 1). There was continuity
between mesenteric fat and the fatty core. Strand-like
densities were also observed within the fatty core and
appeared to be connected to branches of the mesenteric
vessels (Figure 2). No active contrast extravasation was
detected. Inverted Meckel’s diverticulum was the main
differential diagnosis given the morphology and location
of the lesion and its continuity with mesenteric fat.
Figure 1. Selected axial computed tomography images in the
angiographic phase showing the cross-sectional view of the
inverted Meckel’s diverticulum (a) at a higher position, its fatty core
(thin arrow); and (b) at a lower position, the enhancing wall (thick
arrow) of the inverted Meckel’s diverticulum, located within the
lumen of the distal ileum (arrowheads).
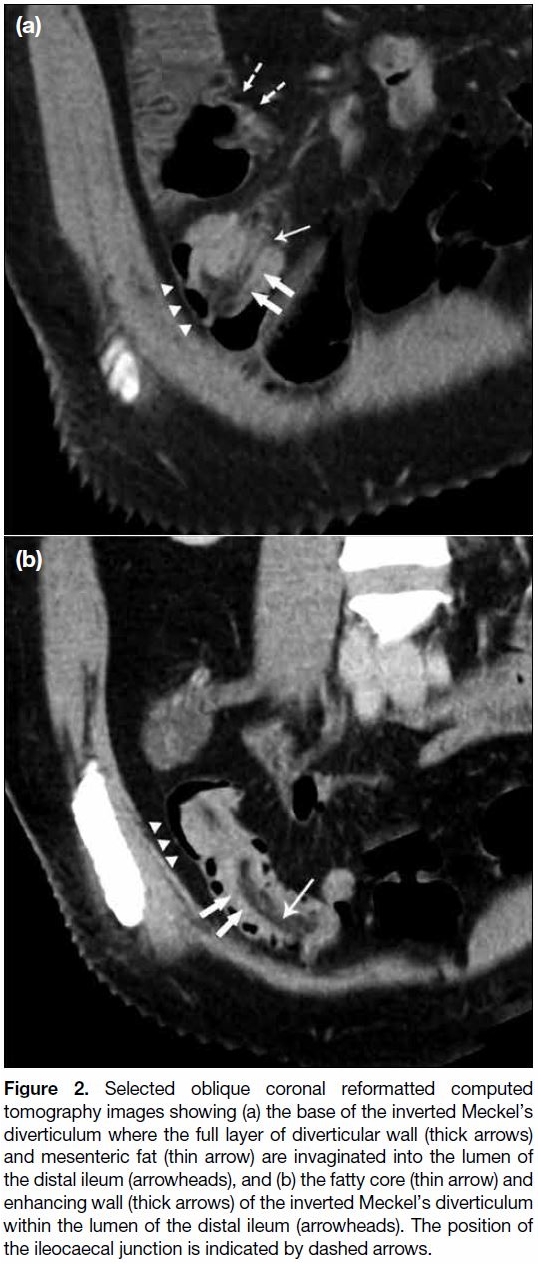
Figure 2. Selected oblique coronal reformatted computed
tomography images showing (a) the base of the inverted Meckel’s
diverticulum where the full layer of diverticular wall (thick arrows)
and mesenteric fat (thin arrow) are invaginated into the lumen of
the distal ileum (arrowheads), and (b) the fatty core (thin arrow) and
enhancing wall (thick arrows) of the inverted Meckel’s diverticulum
within the lumen of the distal ileum (arrowheads). The position of
the ileocaecal junction is indicated by dashed arrows.
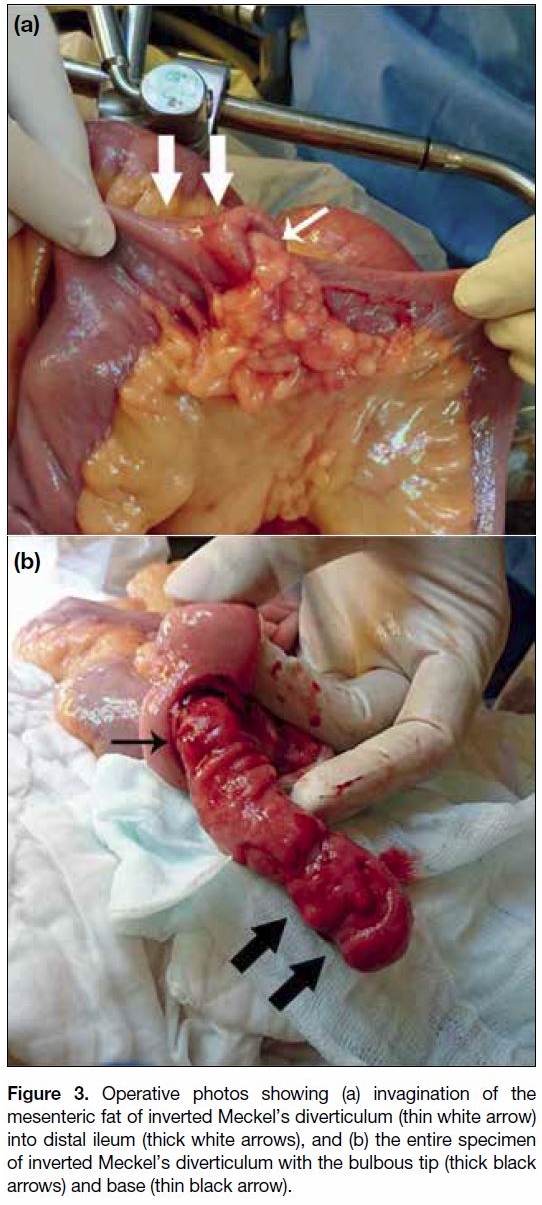
Urgent laparotomy was performed. Intraoperatively, a
mass was felt along the distal ileum, about two thirds
along the length of the small bowel from the ligament of Treitz. On the serosal side of the small bowel segment
where the mass was located, a focal point of invagination
of the bowel wall and mesenteric tissue into the luminal
side was identified. The finger-like intraluminal mass was
brought out via an enterostomy (Figure 3). Ulcerative
mucosa was seen along the inverted diverticular wall
with a pulsative spurter. The involved segment of small bowel was resected and an end-to-end ileoileal
anastomosis created. The procedure was uneventful.
Figure 3. Operative photos showing (a) invagination of the
mesenteric fat of inverted Meckel’s diverticulum (thin white arrow)
into distal ileum (thick white arrows), and (b) the entire specimen
of inverted Meckel’s diverticulum with the bulbous tip (thick black
arrows) and base (thin black arrow).
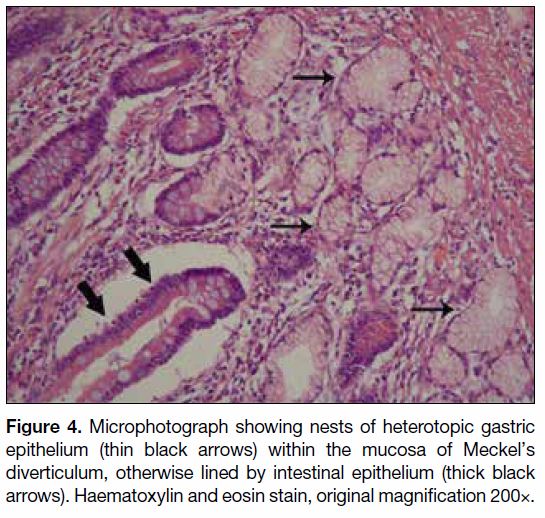
Gross examination of the resected specimen confirmed
an inverted diverticulum manifesting as a 7-cm long
tubular intraluminal mass. Histological examination
showed that the lesion contained all layers of the intestinal wall, as well as a core of fibroadipose tissue
that consisted of invaginated mesenteric tissue. The
mucosal surface of the lesion had focal ulcerations and
contained heterotopic gastric tissue (Figure 4).
Figure 4. Microphotograph showing nests of heterotopic gastric
epithelium (thin black arrows) within the mucosa of Meckel’s
diverticulum, otherwise lined by intestinal epithelium (thick black
arrows). Haematoxylin and eosin stain, original magnification 200×.
DISCUSSION
Meckel’s diverticulum results from failure of regression
of the omphalomesenteric duct that connects the yolk sac to the mid gut through the umbilical cord in the
embryo. This duct typically closes by the 5th to 8th week
of gestation. Meckel’s diverticulum arises from the
antimesenteric border of the distal ileum, typically within
100 cm of the ileocaecal valve. It usually measures up to
5 cm in length and 2 cm in diameter. Heterotopic mucosa,
most commonly gastric type (up to 60%), is found
in about half of Meckel’s diverticula. Although most
Meckel’s diverticula remain clinically asymptomatic,
they can be complicated by haemorrhage from peptic
ulceration, diverticulitis, intussusception, volvulus, or
development of neoplasm within the diverticulum and
inversion.[1]
Inversion of Meckel’s diverticulum is a rare phenomenon,
with about 70 cases reported in the English literature.[2,3] The condition occurs when the diverticulum inverts
upon itself and invaginates into the lumen of the terminal
ileum. The pathophysiology is not well understood. One
theory is that abnormal peristaltic movement at the base
of the diverticulum due to ectopic tissue or ulceration
causes the diverticulum to invert.[4] The most common
complications are intussusception, where the inverted
diverticulum acts as a lead point, and gastrointestinal
bleeding due to ulceration in the inverted diverticulum.
Although ulceration in Meckel’s diverticulum is most
commonly due to acid secretion by heterotopic gastric
mucosa, it also occurs in inverted Meckel’s diverticulum
that does not contain heterotopic gastric mucosa. This is
postulated to be due to repeated mucosal trauma due to
intermittent intussusception of the diverticulum and its potential ischaemic vulnerability as the diverticulum is
supplied by the remnant of the vitelline artery, an end
branch of the superior mesenteric artery, and has no
collateral arterial supply.[4,5]
Patients with an inverted Meckel’s diverticulum can
present with a constellation of symptoms consistent
with acute or chronic gastrointestinal bleeding, intestinal
obstruction or recurrent abdominal pain, depending on
the complications.[3] Computed tomography (CT) is an
important diagnostic tool since clinical diagnosis of
inverted Meckel’s diverticulum can often be challenging.
Inverted Meckel’s diverticulum has characteristic
imaging features on CT. The inverted diverticulum
appears as a tubular intraluminal small bowel lesion
located in the distal small bowel with a central fatty core that demonstrates continuity with mesenteric fat. This
correlates with the invagination of mesenteric tissue
into the core of the inverted diverticulum. A thick rim of
enhancing soft tissue around the fatty core corresponds
to the full layer of the diverticular wall.[2,3,4] Intermittent
bleeding may cause false negative findings on CT
angiography.[6] Bowel-in-bowel appearance can be seen if
the diverticulum acts as the lead point for intussusception.[7]
These features readily allow differentiation from other
fat-containing small bowel lesions, namely lipoma and
ileal-ileal intussusception. A small bowel lipoma is
covered only by a thin layer of mucosa and lacks the thick
soft tissue collar seen in inverted Meckel’s diverticulum
(Figure 5). More importantly, the fat within the lipoma
does not demonstrate continuation with mesenteric
fat. In ileal-ileal intussusception, the central part of the
intussusceptum contains bowel lumen instead of fat and
the mesenteric fat lies between the intussusceptum and
intussuscipiens.
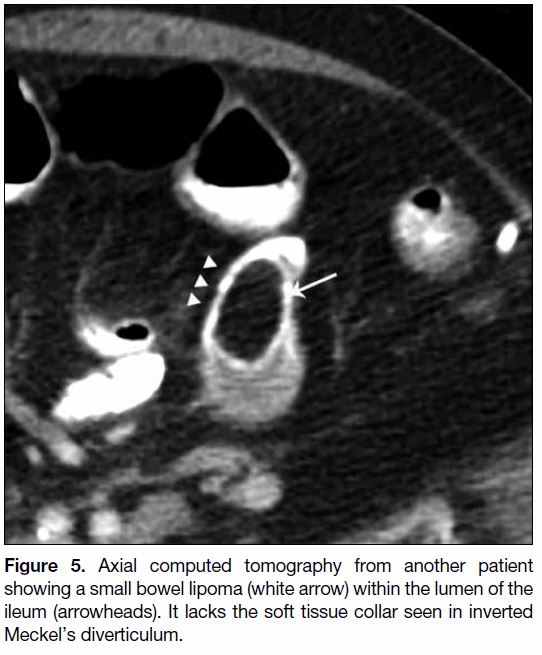
Figure 5. Axial computed tomography from another patient
showing a small bowel lipoma (white arrow) within the lumen of the
ileum (arrowheads). It lacks the soft tissue collar seen in inverted
Meckel’s diverticulum.
Definitive treatment of an inverted Meckel’s diverticulum
is surgical resection of the involved segment of small
bowel with subsequent anastomosis.[2]
REFERENCES
1. Levy AD, Hobbs CM. From the archives of the AFIP: Meckel
diverticulum: radiologic features with pathologic correlation.
Radiographics. 2004;24:565-87. Crossref
2. Pantongrag-Brown L, Levine MS, Elsayed AM, Buetow PC,
Agrons GA, Buck JL. Inverted Meckel diverticulum: clinical,
radiologic, and pathologic findings. Radiology. 1996:199;693-6. Crossref
3. Rashid OM, Ku JK, Nagahashi M, Yamada A, Takabe K. Inverted
Meckel’s diverticulum as a cause of occult lower gastrointestinal
hemorrhage. World J Gastroenterol. 2012;18:6155-9. Crossref
4. Blakeborough A, McWilliams RG, Raja U, Robinson PJ,
Reynolds JV, Chapman AH. Pseudolipoma of inverted Meckel’s
diverticulum: clinical, radiological and pathological correlation. Eur
Radiol. 1997;7:900-4. Crossref
5. Heider R, Warshauer DM, Behrns KE. Inverted Meckel’s
diverticulum as a source of chronic gastrointestinal blood loss.
Surgery. 2000;128:107-8. Crossref
6. Artigas JM, Martí M, Soto JA, Esteban H, Pinilla I, Guillén E. Multidetector CT angiography for acute gastrointestinal bleeding:
technique and findings. Radiographics. 2013;33:1453-70. Crossref
7. Kim JH, Park SH, Ha HK. Case 156: Inverted Meckel diverticulum. Radiology. 2010;255:303-6. Crossref