Percutaneous Transhepatic Biliary Stones Removal — An Effective and Safe Alternative
ORIGINAL ARTICLE
Percutaneous Transhepatic Biliary Stones Removal — An Effective and Safe Alternative
JHM Cheng, WKW Leung, AHC Wong, BKH Lee, BST Leung, CY Chu, WK Kan
Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
Correspondence: Dr JHM Cheng, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong. Email: chm915@ha.org.hk
Submitted: 21 Nov 2017; Accepted: 22 Jan 2018.
Contributors: JHMC and WKWL designed the study. JHMC, BKHL and BSTL acquired the data. JHMC analysed the data. JHMC and AHCW
drafted the manuscript. WKWL, CYC and WKK critically revised the manuscript for important intellectual content. All authors had full access
to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflict of interest to declare.
Declaration: This study was presented as poster presentation in Annual Scientific Meeting of Hong Kong College of Radiologists 2017, 18-19 November 2017.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: Ethics approval was granted by the Hong Kong East Cluster Research Ethics Committee (Ref HKECREC-2019-088).
Abstract
Introduction
Percutaneous transhepatic biliary stone removal is a well-established treatment for biliary stone disease,
as an alternative to the standard endoscopic or surgical approaches. We present our experience in biliary stone
removal via the percutaneous transhepatic route, focusing on the techniques, clinical success rate, and complications.
Methods
Data on all percutaneous transhepatic biliary stone removals performed at our institution between
January 2014 and May 2017 were extracted from patient records. Clinical outcomes, procedure success rate, and
complication rate were analysed.
Results
In total, 33 procedures were performed in 27 consecutive patients (24 men, 3 women, median age = 78.0
years; range, 55-92 years). Reasons for percutaneous transhepatic biliary stone removal included contra-indication
to or failure of endoscopic removal (prior gastrectomy or duodenal surgery, n = 19; failed endoscopic retrograde
cholangiopancreatography cannulation, n = 3; duodenal stenosis, n = 3; and hepaticojejunostomy stricture, n = 1),
and one patient had intrahepatic ductal stones not amenable to endoscopic removal. The overall clinical success rate
was 90.9%, with an initial procedure success of complete ductal clearance achieved in 24 cases (72.7%) after the
first attempt. Stone removal was unsuccessful in two cases, and incomplete stone removal was present in one case,
which were all related to unfavourable biliary anatomy. There were no significant complications (0%) or mortality
(0%). The mild complication rate was 15.2% (mild haemobilia, n = 5).
Conclusion
Percutaneous transhepatic biliary stone removal is an effective and safe procedure. It is a reliable
alternative for patients when endoscopic or surgical approaches are not feasible or unsuccessful.
Key Words: Catheters; Choledocholithiasis/TH; Radiology, interventional/IS; Safety; Surgical endoscopy
中文摘要
經皮經肝膽道結石切除術:有效且安全的替代方法
鄭希敏、梁錦榮、黃可澄、李家灝、梁肇庭、朱志揚、簡偉權
引言
經皮肝穿刺膽道結石切除術是一種公認的膽道結石治療方法,可替代標準內窺鏡或手術方法。本文介紹通過經皮經肝切除膽管結石的經驗,其中重點包括技術、臨床成功率和併發症。
方法
從患者記錄中提取2014年1月至2017年5月期間在本院進行所有經皮經肝穿刺膽道結石切除術的數據。分析臨床結果、手術成功率和併發症發生率。
結果
共27例患者進行33次手術(男24例,女3例,年齡介乎55-92歲,中位年齡78.0歲)。進行經皮經肝膽管結石切除術原因包括內鏡切除術禁忌或失敗(19例曾進行胃切除術或十二指腸手術、3例內鏡逆行胰膽管造影插管失敗、3例十二指腸狹窄以及1例肝空腸造口狹窄),1名患者的肝內導管結石不適合內鏡下摘除。總體臨床成功率為90.9%,首次嘗試後的24例(72.7%)患者成功完成導管清除術。結石清除不成功2例,結石清除不完全1例,均與膽道解剖結構不良有關。沒有嚴重併發症(0%)或死亡(0%)。輕度併發症發生率為15.2%(輕度血友病5例)。
結論
經皮經肝膽道結石切除術是一種安全有效的方法。當內窺鏡或手術方法不可行或不成功時,它是患者的可靠選擇。
INTRODUCTION
Biliary duct stone disease, or choledocholithiasis, is the
commonest cause of non-malignant biliary obstruction,
occurring in 10% of the adult population and up to 14.7%
of post-cholecystectomy patients.[1] [2] [3] [4] Recommended
first-line treatments for choledocholithiasis include
endoscopic retrograde cholangiopancreatography with
sphincterotomy, and laparoscopic common bile duct
exploration.[5] In Hong Kong, the endoscopic approach is
the primary modality in the current standard of practice,
followed by surgical exploration of common bile duct.
However, there are situations where endoscopic or
surgical approaches are not feasible or unsuccessful,
and the percutaneous transhepatic approach offers an
invaluable alternative for biliary stone removal.
We present our experience in biliary stone removal via
the percutaneous transhepatic route, with the discussion
focusing on the techniques, clinical success rate, and
complications.
METHODS
All 27 consecutive patients with symptomatic
choledocholithiasis who underwent a total of 33 sessions
of percutaneous transhepatic removal of biliary stones in
our department from January 2014 to May 2017 were
included and retrospectively reviewed.
The electronic patient records, laboratory results, and
interventional procedure records were evaluated. The
computed tomography and interventional procedure
fluoroscopic images were reviewed through the
PACS system. The patients were followed up for
a mean (±standard deviation) period of 19.5±10.8
months. Procedure success was defined as achieving
ductal clearance, and clinical success was defined as
improvement in clinical condition and liver function.
Procedure-related complications were defined as adverse
events occurring within 30 days after the procedure.
Technique
A percutaneous transhepatic biliary drainage (PTBD)
catheter was usually inserted for bile drainage and
decompression of the biliary tree 1 to 2 weeks before
the procedure. This aided in reducing ductal wall and
sphincter of Oddi oedema, aiding the subsequent stone
removal procedure.
Just as with other interventional biliary procedures, all
patients were administered prophylactic parental broad-spectrum
antibiotics, given 24 hours prior and on the day of
the procedure. A dose of 25 to 100 μg of intravenous
fentanyl was administered to achieve adequate
analgesic effect, especially during balloon dilatation
for sphincteroplasty. Preprocedural blood tests included a complete blood count and clotting profile. Any
coagulopathy was corrected based on the Consensus
Guidelines for Coagulation Status and Hemostasis Risk
for category 3 procedures, i.e., international normalised
ratio ≤1.5 and platelets ≥50 × 109/L.[6]
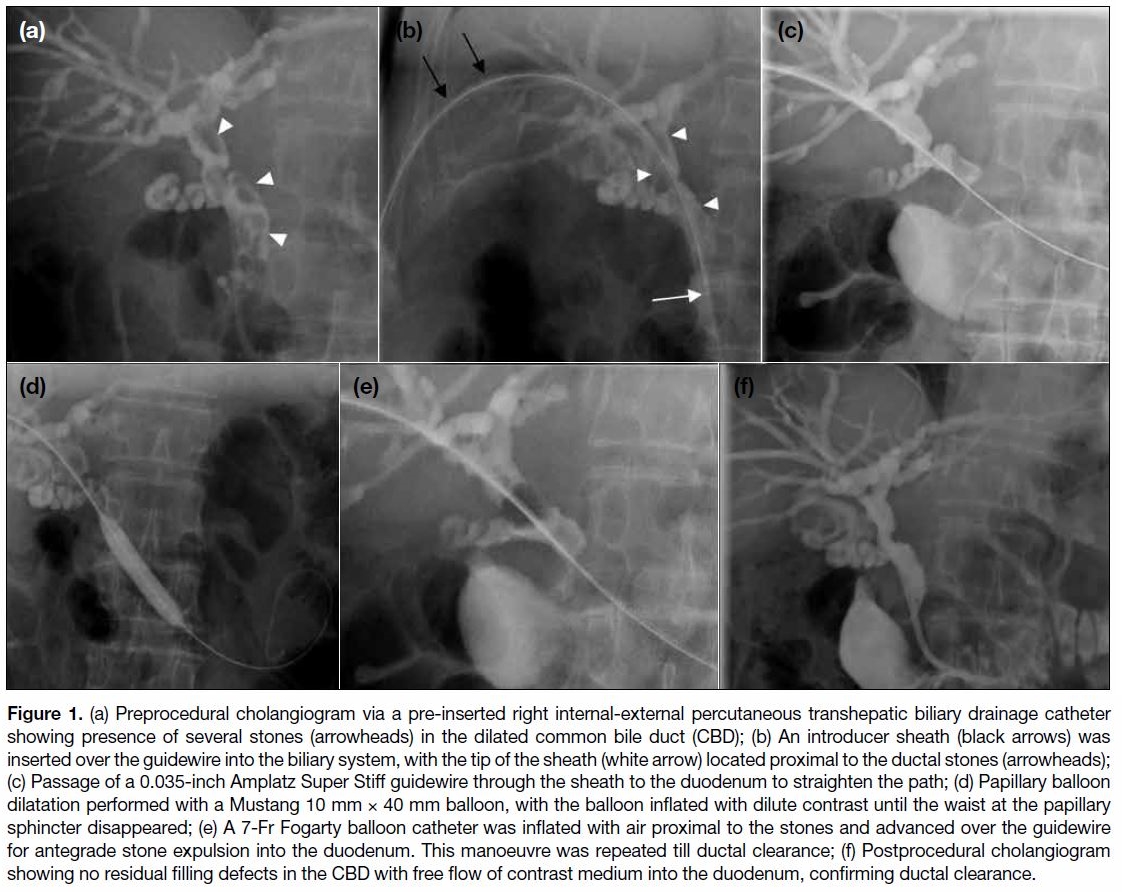
A preprocedural cholangiogram was performed via the
PTBD catheter, confirming the presence, number, and
location of biliary stones, as well as the status of the
papilla of Vater and the anatomy of the biliary drainage
pathway. A flexible introducer sheath (8-Fr Super
Arrow-Flex sheath, Teleflex Medical, Athlone, Ireland)
was introduced into the biliary tree after exchange over
a 0.035-inch stiff guidewire (UltraStiff guidewire, Cook
Medical, Bloomington [IN], US; Super Stiff guidewire,
Boston Scientific, Natwick [MA], US). Passage of a stiff
guidewire through the sheath to the duodenum followed,
to straighten the path and facilitate stone removal.
Papillary balloon dilatation (sphincteroplasty) was then performed with an angioplasty balloon (Mustang
balloon dilatation catheter; Boston Scientific, Natwick
[MA], US), with balloon size ranging from 8 to 12 mm.
The balloon was inflated with diluted contrast material
until the waist at the papillary sphincter disappeared.
The balloon catheter was then deflated and removed
with care to avoid retraction of stones into the peripheral
ducts. A 6- to 7-Fr Fogarty balloon catheter (Edwards
Lifesciences, Irvine [CA], US) was introduced over
the guidewire with the balloon inflated proximal to the
biliary stones. The Fogarty balloon was inflated with
air and advanced further over the guidewire to expel the
biliary stones into the duodenum. Air was used instead of
contrast material to provide negative contrast within the
contrast-filled biliary tree. In addition, inflation with air
renders the balloon more easily compressible so that it
can more easily cross the sphincter during stone removal.
This manoeuvre was repeated several times if necessary
to achieve complete ductal clearance (Figure 1).
Figure 1. (a) Preprocedural cholangiogram via a pre-inserted right internal-external percutaneous transhepatic biliary drainage catheter
showing presence of several stones (arrowheads) in the dilated common bile duct (CBD); (b) An introducer sheath (black arrows) was
inserted over the guidewire into the biliary system, with the tip of the sheath (white arrow) located proximal to the ductal stones (arrowheads);
(c) Passage of a 0.035-inch Amplatz Super Stiff guidewire through the sheath to the duodenum to straighten the path; (d) Papillary balloon
dilatation performed with a Mustang 10 mm × 40 mm balloon, with the balloon inflated with dilute contrast until the waist at the papillary
sphincter disappeared; (e) A 7-Fr Fogarty balloon catheter was inflated with air proximal to the stones and advanced over the guidewire
for antegrade stone expulsion into the duodenum. This manoeuvre was repeated till ductal clearance; (f) Postprocedural cholangiogram
showing no residual filling defects in the CBD with free flow of contrast medium into the duodenum, confirming ductal clearance.
At the end of each procedure, cholangiography was
performed to evaluate for any residual stones. After
ductal clearance of stones, an internal-external PTBD
catheter was then inserted for temporary biliary
drainage. A follow-up cholangiogram in about 2 to 4
weeks after the procedure was scheduled for all patients,
and removal of the PTBD catheter could be considered if
ductal clearance was confirmed.
RESULTS
In total, 33 procedures were performed in 27 consecutive patients (24 men, 3 women, median age, 78.0 years;
range, 55-92 years) and data on these procedures were
retrospectively reviewed.
The most common presenting symptom in our cases was
cholangitis (n = 21), followed by biliary pancreatitis (n = 4),
biliary colic (n = 1), and persistently abnormal liver
function (n = 1).
The reasons for percutaneous transhepatic biliary stone
removal in our cases were mainly related to endoscopic
contra-indications or failures, including prior gastrectomy
or duodenal surgery (n = 19), failed endoscopic retrograde
cholangiopancreatography cannulation (n = 3), duodenal
stenosis (n = 3), or hepaticojejunostomy stricture (n = 1);
and intrahepatic duct (IHD) stones not amenable to
endoscopic removal (n = 1).
The locations of calculi included extrahepatic (n = 28), intrahepatic (n = 1), mixed intra- and extra-hepatic (n = 3)
and cystic duct remnant (n = 1). The mean diameter of
calculi was 11.7±5.4 mm.
Complete removal of stones was achieved in 24 cases
(72.7%) after the first attempt. Six patients had residual
stones after the first procedure and were scheduled
for a second session after several days to weeks, and
subsequent complete ductal clearance were achieved in
five additional cases (87.9%). One case had tiny residual
stones in the left IHD, which spontaneously passed,
giving an overall clinical success rate of 90.9%. Stone
removal was unsuccessful in two cases and partial ductal
clearance was achieved in one case.
Preprocedural obstructive derangement of liver function
tests was present in 12 cases, with improvement noted
after biliary stone removal in 10 cases, while the
remaining two cases showed static results.
There were no adverse events such as bile duct or
duodenal perforation, cholangitis, pancreatitis, vascular injury, or mortality encountered in any of our cases. Mild
haemobilia was encountered in five cases (15.2%), which
were detected during the procedure and spontaneously
resolved without further intervention. The median
procedure time was 45 minutes (range, 20-140 minutes).
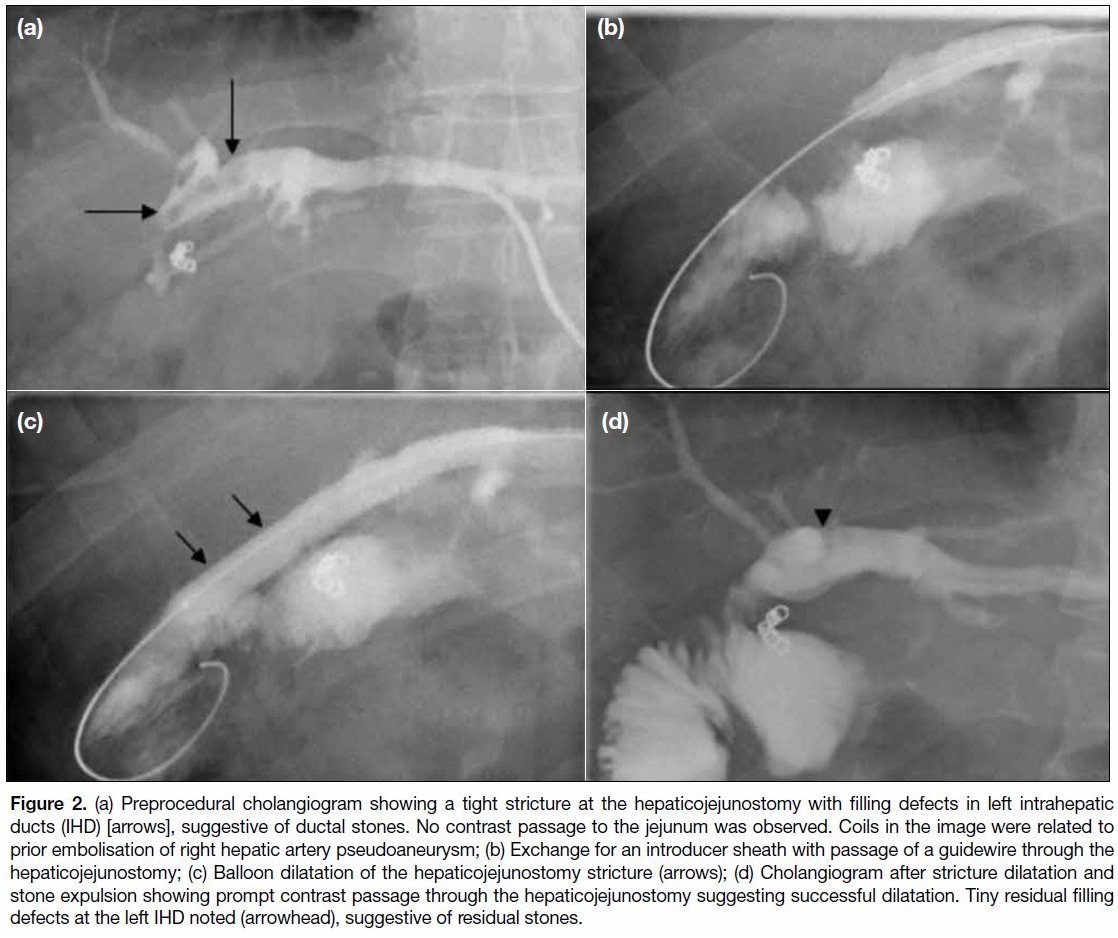
In one case with a hepaticojejunostomy anastomosis
stricture complicated by biliary stones, the same
technique was performed with balloon catheters placed
across the stricture for dilatation (9 mm × 40 mm Mustang
balloon catheter, Boston Scientific, Natwick [MA],
US). Subsequent antegrade stone expulsion through
the hepaticojejunostomy into the jejunum was similarly
performed with a Fogarty balloon catheter. Small residual
stones in the left IHD were noted on postprocedural
cholangiography, with spontaneous passage confirmed
on subsequent cholangiography (Figure 2).
Figure 2. (a) Preprocedural cholangiogram showing a tight stricture at the hepaticojejunostomy with filling defects in left intrahepatic
ducts (IHD) [arrows], suggestive of ductal stones. No contrast passage to the jejunum was observed. Coils in the image were related to
prior embolisation of right hepatic artery pseudoaneurysm; (b) Exchange for an introducer sheath with passage of a guidewire through the
hepaticojejunostomy; (c) Balloon dilatation of the hepaticojejunostomy stricture (arrows); (d) Cholangiogram after stricture dilatation and
stone expulsion showing prompt contrast passage through the hepaticojejunostomy suggesting successful dilatation. Tiny residual filling
defects at the left IHD noted (arrowhead), suggestive of residual stones.
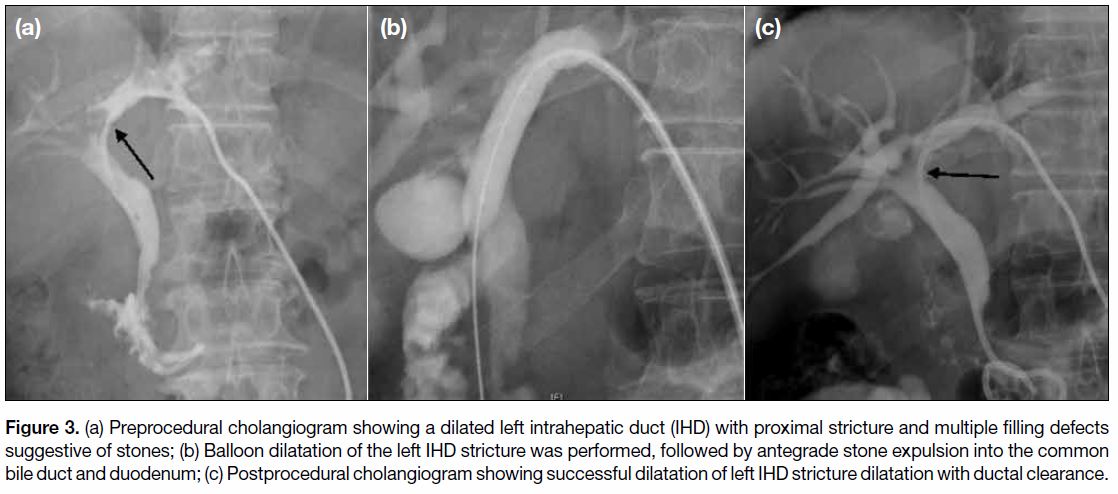
A case of known recurrent pyogenic cholangitis
complicated by a left IHD stricture and multiple IHD
stones had stricture dilatation and antegrade stone
expulsion performed in a similar manner (Figure 3).
Figure 3. a) Preprocedural cholangiogram showing a dilated left intrahepatic duct (IHD) with proximal stricture and multiple filling defects
suggestive of stones; (b) Balloon dilatation of the left IHD stricture was performed, followed by antegrade stone expulsion into the common
bile duct and duodenum; (c) Postprocedural cholangiogram showing successful dilatation of left IHD stricture dilatation with ductal clearance.
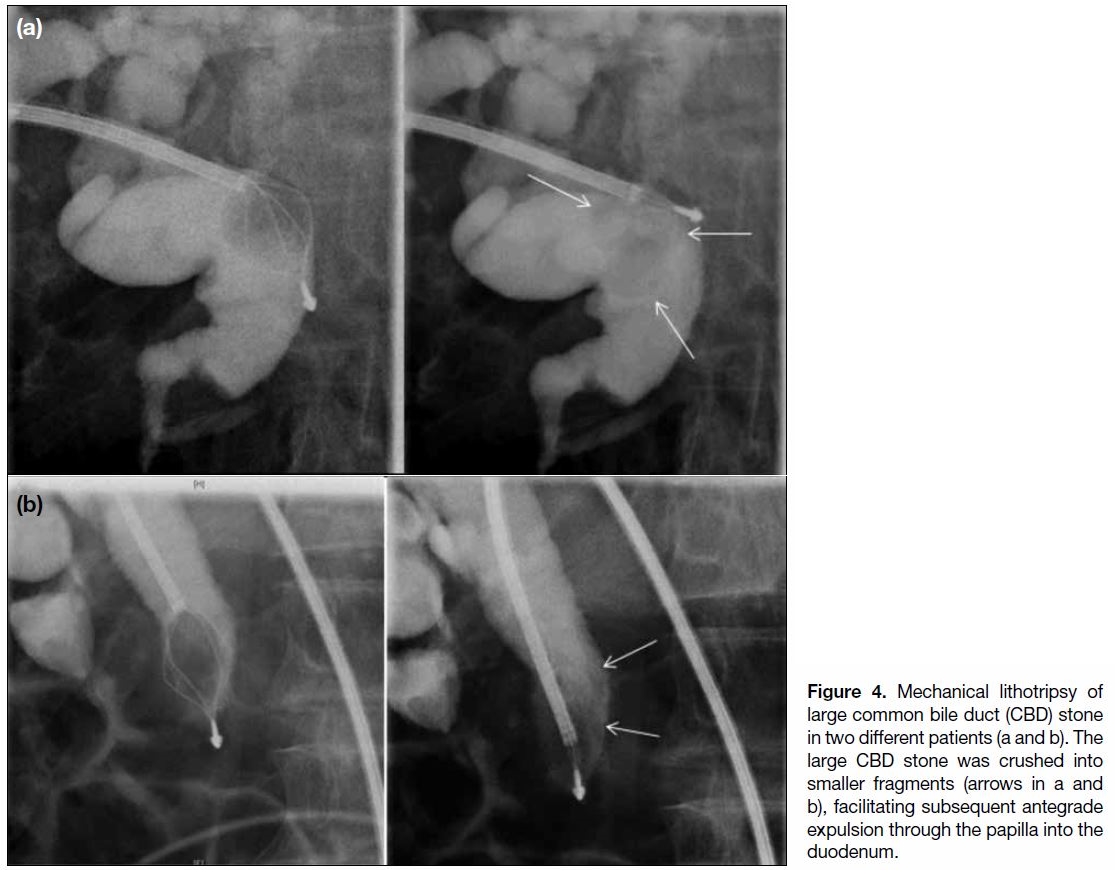
In addition to the stone expulsion procedures described
above, five cases required further manipulation with
stone fragmentation performed. With stones >12 mm
in diameter, we performed stone fragmentation by
mechanical lithotriptor (LithoCrushV, Olympus
Medical Systems, Tokyo, Japan) to facilitate antegrade
expulsion into the duodenum. An introducer sheath with
larger French size (9-10 Fr) was required to introduce
the mechanical lithotriptor. We used a mechanical
lithotriptor (LithoCrushV, Olympus) to capture and
crush the large stones. This device was intended to be
used via an endoscopic approach. However, it was not
user-friendly when used via a percutaneous approach,
with extensive length hanging outside the body. After
fragmentation of the large stones into smaller sizes, the
stones were expelled into the duodenum by the usual
Fogarty technique (Figure 4).
Figure 4. Mechanical lithotripsy of large common bile duct (CBD) stone in two different patients (a and b). The large CBD stone was crushed into smaller fragments (arrows in a and b), facilitating subsequent antegrade expulsion through the papilla into the duodenum.
DISCUSSION
Endoscopic management of biliary stone disease in
combination with endoscopic sphincterotomy is a well-established
treatment and often the first-line modality for
stone removal, with a high success rate up to 90% in the
hands of experienced endoscopists.[4] However, in situations
where the endoscopic approach is unfeasible (e.g., patients
with prior gastrectomy, duodenal stenosis, IHD stones),
or when endoscopic biliary access is unsuccessful,
percutaneous stone removal is another well-known non-operative
technique for treatment of biliary stones.
The percutaneous approach to biliary stone removal was
first introduced by Mondet in 1962[7] and Mazzariello in
1970[8] using articulated forceps, and later modified by
Burhenne et al[9] with the additional use of biliary baskets.
Their methods were effective with success rates up to
95%, however, their approaches required substantial
tract dilatation. A modified technique of percutaneous
stone removal with aid of balloon papillary dilatation
was later proposed by Centola et al in 1981.[10] This
approach was also confirmed to be safe and effective by
several studies.[11] [12] [13] [14] [15] [16] [17] [18] [19]
In our institution, we were able to achieve a high success
rate with a high safety profile in the percutaneous
transhepatic approach of biliary stone removal. The
overall clinical success rate was 90.9%. The initial
procedure success rate was 72.7% after the first attempt
and 87.9% after the second attempt in achieving complete ductal clearance. Our experience was comparable to
other studies, with reported success rates of 86.7% to
96%.[11] [12] [13] [14] [15] [16] [17] [18] [19]
We only had two cases of treatment failures and one case
of partial ductal clearance, all related to unfavourable
biliary ductal anatomy rendering difficult lithotripsy and
stone expulsion. One case had a capacious cystic duct
remnant leading to repeated migration of mobile stones
back to the remnant, and the other two cases were of
large stones (mean diameter = 20 mm) within a tortuous
biliary duct leading to ineffective mechanical lithotripsy
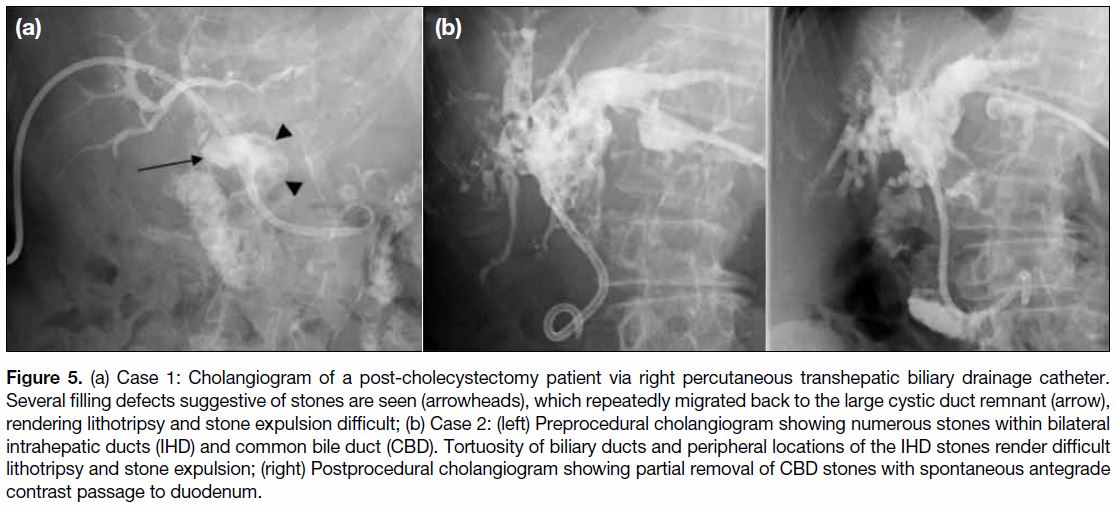
and antegrade stone expulsion (Figure 5).
Figure 5. (a) Case 1: Cholangiogram of a post-cholecystectomy patient via right percutaneous transhepatic biliary drainage catheter.
Several filling defects suggestive of stones are seen (arrowheads), which repeatedly migrated back to the large cystic duct remnant (arrow),
rendering lithotripsy and stone expulsion difficult; (b) Case 2: (left) Preprocedural cholangiogram showing numerous stones within bilateral
intrahepatic ducts (IHD) and common bile duct (CBD). Tortuosity of biliary ducts and peripheral locations of the IHD stones render difficult
lithotripsy and stone expulsion; (right) Postprocedural cholangiogram showing partial removal of CBD stones with spontaneous antegrade
contrast passage to duodenum.
We did not have any significant procedure-related
complication (0%) or mortality (0%), including bile
duct or duodenal perforation, cholangitis, pancreatitis, or
vascular injury. The minor complication rate was 15.2%, which were all mild haemobilia encountered during the
procedure that spontaneously subsided without further
intervention.
The reported significant complication rates in other
studies range from 0% to 6.8%. The more common ones
were severe haemobilia resulting in organ failure or
death, cholangitis, and pancreatitis. Other rare significant
complications included liver abscess and vascular injury
(right hepatic artery transection, pancreaticoduodenal
artery pseudoaneurysm, common bile duct or duodenal
perforation, and mortality).[15] [16] [17] [18] [19]
Other Techniques
Various percutaneous techniques of biliary duct stones
removal have been described in the literature, including
stone extraction by forceps or baskets; antegrade
expulsion of stones into the duodenum by forceful
irrigation, or with the aid of various angioplasty
balloon catheters, with or without stone fragmentation;
chemolitholysis; papillary balloon dilatation
(sphincteroplasty); and stricture dilatation.[1] [3] [10] [20] [21]
We preferred the method of antegrade stone expulsion
over percutaneous transhepatic stone extraction, due to
the potential injury to the liver parenchyma adjacent to
the tract associated with the stone extraction procedure
and the high effectiveness of antegrade removal.[1]
All of our cases had PTBD performed several days
to weeks prior to the stone removal, to allow time for biliary sepsis and/or papillary sphincter oedema to
resolve.[1]
We also performed balloon sphincteroplasty in all cases,
which is reported to be highly effective in facilitating
subsequent stone removal.[11] [12] [13] [14] [15] Mechanical expulsion of
stones through the ampulla of Vater without sphincter
dilation has been reported; however, it was found
to be associated with higher rates of postprocedural
pancreatitis due to difficulty in pushing stones against the
non-dilated papilla resulting in buckling of angioplasty
balloons or baskets.[22] [23] [24] In addition, it was also less
traumatic as compared with the conventional endoscopic
sphincterotomy, with major advantages of lower risk
of sphincterotomy-induced bleeding and preservation
of sphincter function, which have been proven by
manometric studies.[25] Some studies also reported
lower rate of pancreatitis (0%-1.5%) as compared with
sphincterotomy or even retrograde sphincteroplasty
(4%-35%).[15] [18] [19]
The selection of angioplasty balloon diameter for
sphincteroplasty was based on the size of ductal stones
and the common bile duct itself. We avoided selection of
large balloon sizes and inflation of balloons exceeding
14 mm in diameter, in order to minimise the risk of
common bile duct perforation.[19]
In a few cases, the basic procedures described were
insufficient for complete stone removal, particularly
the larger stones. In these cases, we adopted additional manoeuvres, including advancement of the Fogarty
balloon catheter together with the introducer sheath to
strengthen the pushing force, and/or using a balloon
of larger size for sphincteroplasty. In several cases,
we also performed additional stone fragmentation by
mechanical lithotripsy. Other reported techniques of
stone size reduction include contact chemolitholysis
with monooctanoin, stone dissolution with methyl
tertbutylether, and other mechanical fragmentation
techniques such as electrohydraulic, laser, ultrasonic
shock waves, and electromagnetic waves.[1] [12] [15] [20] [26]
Finally, at the end of the procedure, due to the transient
oedema or spasm of the papilla after sphincteroplasty,
potential blockage of the biliary and pancreatic drainage
pathway might occur. Hence, an internal-external
PTBD catheter is inserted in all of our cases to ensure
satisfactory biliary drainage to minimise the risk of
cholangitis or pancreatitis.[16] [18]
The limitations of our study are the retrospective nature
and relatively small sample size, limiting the evaluation
of rare but significant complications that were reported
in the literature.[15] [16] [17] [18] [19]
CONCLUSION
In conclusion, our study demonstrated that percutaneous
transhepatic antegrade biliary stone removal with balloon
sphincteroplasty is an effective and safe procedure for
treatment of biliary stones. It is an alternative for patients
when the endoscopic or laparoscopic approach is not
feasible or unsuccessful, and we encourage the practice
of this technique, as a minimally invasive treatment
option before consideration of surgical exploration.
REFERENCES
1. Ilgit ET, Gürel K, Onal B. Percutaneous management of bile duct
stones. Eur J Radiol. 2002;43:237-45. Crossref
2. Schirmer BD, Winters KL, Edlich RF. Cholelithiasis and
cholecystitis. J Long Term Eff Med Implants. 2005;15:329-38. Crossref
3. Riciardi R, Islam S, Canete JJ, Arcand PL, Stoker ME. Effectiveness
and long-term results of laparoscopic common bile duct exploration.
Surg Endosc. 2003;17:19-22. Crossref
4. Perissat J, Huibregtse K, Keane FB, Russell RC, Neoptolemos
JP. Management of bile duct stones in the era of laparoscopic
cholecystectomy. Br J Surg. 1994;81:799-810. Crossref
5. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R,
Webster G, et al. Updated guideline on the management of common
bile duct stones (CBDS). Gut. 2017;66:765-82. Crossref
6. Patel IJ, Davidson JC, Nikolic B, Salazar GM, Schwartzberg MS,
Walker TG, et al. Consensus guidelines for periprocedural
management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol.
2012;23:727-36. Crossref
7. Mondet AF. Technic of blood extraction of calculi in residual
lithiasis of the choledochus [in Spanish]. Bol Trab Soc Cir B Aires.
1962;46:278-90.
8. Mazzariello R. Removal of residual biliary tract calculi without
reoperation. Surgery. 1970;67:566-73.
9. Burhenne HJ. Nonoperative retained biliary tract stone extraction.
A new roentgenologic technique. Am J Roentgenol Radium Ther
Nucl Med. 1973;117:388-99. Crossref
10. Centola CA, Jander HP, Stauffer A, Russinovich NA. Balloon
dilatation of the papilla of Vater to allow biliary stone passage.
AJR Am J Roentgenol. 1981;136:613-4. Crossref
11. Meranze SG, Stein EJ, Burke DR, Hartz WH, McLean GK.
Removal of retained common bile duct stones with angiographic
occlusion balloons. AJR Am J Roentgenol. 1986;146:383-5. Crossref
12. Clouse ME, Stokes KR, Lee RG, Falchuk KR. Bile duct stones:
percutaneous transhepatic removal. Radiology. 1986;160:525-9. Crossref
13. Graziani L, Fabrizzi G, Manfrini E, Galeazzi R, Freddara U.
Percutaneous transhepatic Oddi-sphincter dilatation for bile duct
stone removal. AJR Am J Roentgenol. 1989;152:73-5. Crossref
14. Muchart J, Perendreu J, Casas JD, Díaz-Ruíz MJ. Balloon catheter
sphincteroplasty and biliary stone expulsion into the duodenum in
patients with an indwelling T tube. Abdom Imaging. 1999;24:69-71. Crossref
15. Gil S, de la Iglesia P, Verdú JF, de España F, Arenas J, Irurzun J.
Effectiveness and safety of balloon dilation of the papilla and the
use of an occlusion balloon for clearance of bile duct calculi. AJR
Am J Roentgenol. 2000;174:1455-60. Crossref
16. Szulman C, Giménez M, Sierre S. Antegrade papillary balloon
dilation for extrahepatic bile duct stone clearance: lessons learned
from treating 300 patients. J Vasc Interv Radiol. 2011;22:346-53. Crossref
17. Ozcan N, Kahriman G, Mavili E. Percutaneous transhepatic
removal of bile duct stones: results of 261 patients. Cardiovasc
Intervent Radiol. 2012;35:890-7. Crossref
18. García-García L, Lanciego C. Percutaneous treatment of biliary
stones: sphincteroplasty and occlusion balloon for the clearance
of bile duct calculi. AJR Am J Roentgenol. 2004;182:663-70. Crossref
19. Park YS, Kim JH, Choi YW, Lee TH, Hwang CM, Cho YJ, et al.
Percutaneous treatment of extrahepatic bile duct stones assisted by
balloon sphincteroplasty and occlusion balloon. Korean J Radiol.
2005;6:235-40. Crossref
20. Burhenne HJ. Garland lecture. Percutaneous extraction of
retained biliary tract stones: 661 patients. AJR Am J Roentgenol.
1980;134:889-98. Crossref
21. Raijman I. Intracorporeal lithotripsy in the management of biliary
stone disease. Semin Laparosc Surg. 2000;7:295-301. Crossref
22. Savader SJ, Venbrux AC, Robbins KV, Gittelsohn AM, Osterman FA.
Pancreatic response to percutaneous biliary drainage: a prospective
study. Radiology. 1991;178:343-6. Crossref
23. Lamis PA, Letton AH, Wilson JP. Retained common duct stones: a
new nonoperative technique for treatment. Surgery. 1969;66:291-6.
24. Clouse ME. Dormia basket modification for percutaneous
transhepatic common bile duct stone removal. AJR Am J
Roentgenol. 1983;140:395-7. Crossref
25. Sato H, Kodama T, Takaaki J, Tatsumi Y, Maeda T, Fujita S, et al.
Endoscopic papillary balloon dilatation may preserve sphincter
of Oddi function after common bile duct stone management:
evaluation from the viewpoint of endoscopic manometry. Gut.
1997;41:541-4. Crossref
26. Picus D. Intracorporeal biliary lithotripsy. Radiol Clin North Am.
1990;28:1241-9.