At-home Chemotherapy Infusion for Patients with Advanced Cancer in Hong Kong
PERSPECTIVE
At-home Chemotherapy Infusion for Patients with Advanced Cancer in Hong Kong
SSS Mak1, PE Hui1, WMR Wan1, CLP Yih2
1 Department of Clinical Oncology, Prince of Wales Hospital, New Territories East Cluster, Shatin, Hong Kong
2 Department of Surgery, Prince of Wales Hospital, New Territories East Cluster, Shatin, Hong Kong
Correspondence: Dr Ms SSS Mak, Department of Clinical Oncology, Prince of Wales Hospital, New Territories East Cluster, Shatin, Hong Kong. Email: mss692@ha.org.hk
Submitted: 14 Dec 2019; Accepted: 25 Mar 2020.
Contributors: All authors designed the study. SSSM acquired the data. All authors analysed the data analysis, drafted the manuscript, and
critically revised the manuscript for intellectual content. All authors had full access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Acjknowledgement: This article is based on a presentation given at the 8th Joint Scientific Meeting of The Royal College of Radiologists & Hong Kong College of Radiologists and 27th Annual Scientific Meeting of Hong Kong College of Radiologists 2019, held in Hong Kong, China.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Abstract
This article reviews the development of home-based chemotherapy for patients with advanced cancer in Hong Kong,
highlighting the evolution of chemotherapy infusion devices, practice, and service provision over the past decades.
Further, we provide directions regarding service provision, practice, and training. At-home delivery of chemotherapy
infusions has been used in the treatment of advanced colorectal and pancreatic cancers. It received positive feedback
from patients and had a positive impact on the healthcare system. The model for at-home chemotherapy infusion
could be further promoted and developed in patients with advanced cancer through several means. These could
include exploring the feasibility of more ambulatory home chemotherapy treatment; developing protocols and
selection criteria to guide who should be treated where, how to manage drug toxicity and the expected side-effects,
and assessment of the self-care capabilities of patient and family; and establishing logistics through multidisciplinary
collaboration, chemotherapy nursing clinics, and development of expertise to more efficiently provide resources and
staffing to support at-home chemotherapy infusion. Recognising these challenges, in the future, it would be helpful
to identify new and more advanced practice foci and training initiatives to meet the increased needs of the rising
service load and the population’s need for ongoing access to chemotherapy service.
Key Words: Catheterization, central venous; Chemotherapy, adjuvant / methods; Home infusion therapy; Infusion
pumps; Nurses
中文摘要
香港晚期癌症患者居家化療輸注
麥素珊、許斌、溫偉文、葉春菱
本文回顧在香港為晚期癌症患者提供以居家為基礎的化學治療之發展,強調過去數十年在化療藥物輸注儀器、技術實踐及提供服務的發展。此外,本文描述有關服務、實踐和培訓的發展方向。居家輸注化療的方式已用於治療晚期結直腸癌和胰腺癌,並得到了患者正面的反饋,同時對醫療保健系統產生正面的影響。可通過多種途徑進一步推廣及發展晚期癌症患者居家化療輸注模式。這些途徑包括探究更多流動性居家化學治療的可行性;制定規程及選擇標準以指導誰應該在哪裡進行治療,如何處理藥物毒性及預期副作用,以及評估患者及家庭的自我護理能力;並通過多學科合作、化療護士診所及專門技術構建後勤保障,以更有效地提供資源和人員配備以支援居家化療輸注。認識到這些挑戰將有助於今後確定新的和更先進的實踐目標以及培訓舉措,以滿足正在上升的服務負荷及民眾對持續獲得化療服務不斷增加之需求。
INTRODUCTION
Historically, infusional chemotherapy for patients
with cancer has been delivered in hospitals. Over
the past two decades, chemotherapy practice in
Hong Kong has undergone a shift from inpatient to
outpatient chemotherapy, including delivery of home
chemotherapy. This shift has been partly driven by the
increasing incidence of cancer, with new cases hitting
a record high of 33 075 in 2017[1] and is projected to
increase by around 35% to more than 42 000 new cases
per annum by 2030.[2] Inpatient chemotherapy treatment
may be required for intensive, complex chemotherapy
regimens that can induce severe complications. Such
complications can include bone marrow failure,
prolonged neutropenia, renal toxicity, and tumour lysis
syndrome in bulky tumours. Inpatient treatment may also
be required for unstable disease that imminently requires
chemotherapy or in situations that require hospitalisation
for rigorous monitoring and intervention. However,
most other chemotherapy treatments are implemented
on an outpatient basis, and the proportion of outpatient
treatment is increasing rapidly over time. This has
resulted in an overwhelming demand for oncology
services and hospital beds.
As oncology centres across some clusters are already
delivering chemotherapy services at full capacity, the
increasing demand for services is straining the Hospital
Authority’s service capacity. Future demand for
services is likely to increase further; improving access
to anticancer drugs, improving cancer survival, and an
ageing population are likely to be the key factors causing
this increase. For hospitals without the resources to
appropriately expand their capacity in terms of either
staffing levels or physical space, it is likely that future
patients will face longer waiting lists or reduced service.
Reducing the use of both inpatient beds and ambulatory
day beds for long infusions may help to create capacity
and enhance the cost-effectiveness of the health system.[3] [4]
Home infusion of certain medications such as chemotherapy,[5] opioids,[6] and antibiotics[7] [8] is becoming
a widely used alternative to in-hospital treatment.
Especially in patients with advanced cancer who tend
to be physically fit but receive prolonged chemotherapy,
home chemotherapy provides an opportunity to receive
treatment in the comfort of their homes and the feasibility
to interact much more freely with relatives.
Despite its early use in a few local settings, the development of home chemotherapy infusion is still limited. The 27th
Annual Scientific Meeting of Hong Kong College of
Radiologists 2019 warranted a review of home-based
chemotherapy for patients with advanced cancer in
Hong Kong. The focus of this article is the evolution
of chemotherapy infusion devices, practice, and service
provision in Hong Kong. We aim to present a picture of
the developments in the field and provide directions for
future service provision, practice, and training.
CHEMOTHERAPY INFUSION AT HOME MODEL
There are two commonly cited definitions of
‘chemotherapy at home’. One refers to any type of
administration of chemotherapeutic agents at home (eg,
intravenous, subcutaneous, oral), with or without on-site
supervision by a nurse.[9] The other definition refers to a
service package of chemotherapy-related care provided
by specialist healthcare professionals (usually nurses) at
the patient’s home.[10]
Home chemotherapy can be further categorised as totally
at-home or partially at-home service. For totally at-home
service, the entire process is carried out in the home
setting, for example, short-term infusions delivered at
home by a nurse or injections delivered by parents to
a child with cancer. For partially at-home service, the
first chemotherapy infusion is given in the hospital or
clinic, and later courses or cycles are completed at home
and/or when some hospital or clinic visits are still
required to initiate chemotherapy and disconnect the
infusion pump.
The partially at-home service model is more applicable
for home chemotherapy infusion in Hong Kong because
of the city’s geographical size and the fact that no nurses
currently administer chemotherapy at patients’ homes.
An example of partially at-home service is multi-day
continuous infusion started by a nurse at the hospital,
continued without the nurse’s presence at home, and
finished with disconnection of the pump at the hospital,
which is the common practice of oncology centres in
Hong Kong.
The partially at-home service model is more applicable
for home chemotherapy infusion in Hong Kong because
of the city’s geographical size and the fact that no nurses
currently administer chemotherapy at patients’ homes.
An example of partially at-home service is multi-day
continuous infusion started by a nurse at the hospital,
continued without the nurse’s presence at home, and
finished with disconnection of the pump at the hospital,
which is the common practice of oncology centres in
Hong Kong.
A recent review[5] supported the provision of home-based
chemotherapy as a safe and patient-centred alternative
to hospital and outpatient-based service. Even though
home-based chemotherapy has been proven feasible,
and is facilitated by means of policies in a few countries,
consensus on the best and most cost effective way of
its administration is still lacking.[11] [12] [13] [14] [5] Administration of
chemotherapy in the home setting varies across different
regions of the country, and there is no standard model
that suits all situations. Successful services are tailored to
match local requirements and available resources.
DEVELOPMENT OF HOME
CHEMOTHERAPY INFUSION
SERVICE IN HONG KONG
Early Experience
Implantable long-term venous, epidural, or intrathecal
catheters and electronic ambulatory pumps with
injection ports either totally implanted or tunnelled under
the skin to convenient sites, are commercially available.
Thus, at-home infusion of various medications such as
chemotherapy agents or spinal morphine[6] for patients
with cancer has become feasible. In the 1990s, individual
oncology centres used these devices for continuous
infusion of chemotherapeutic agents via the portal vein
for treatment of colorectal cancer with liver metastases
and for intravenous infusion of the VAD combination
chemotherapy regimen (vincristine, doxorubicin,
dexamethasone) in the treatment of multiple myeloma.
As experience accumulated, the technique was piloted in
Prince of Wales Hospital in 2005 for adjuvant treatment
with a 5-fluorouracil (5FU)–based long-infusion
regimen. A cohort study[16] in 102 patients with colorectal
cancer demonstrated considerable quality-of-life benefits
with ambulatory home infusion via an electronic pump as
compared with inpatient infusion of chemotherapy. That
study also observed reduced treatment delays due to the
lack of inpatient beds, giving cancer patients the option
of receiving chemotherapy at home in Hong Kong.
Promising Benefits and Impact of Current
Service
The use of implantable venous ports and portable infusion
devices in home chemotherapy has become part of the
standard treatment with 5FU-based regimens for various
types of cancer, including colorectal and pancreatic cancer.
These include combination chemotherapy regimens,
such as FOLFOX (folinic acid, 5FU, oxaliplatin) or
FOLFIRI (folinic acid, 5FU, irinotecan), with or without
anti–epidermal growth factor receptor antibodies such
as cetuximab, or panitumumab, or vascular endothelial
growth factor A inhibitor such as bevacizumab.
Both inpatient and outpatient bed days can be saved by
modifying the drug delivery of FOLFOX/FOLFIRI to
occur in the outpatient setting. The 3-hour infusion of
oxaliplatin/irinotecan±cetuximab and 5FU+folinic acid
can be administered in a day centre, followed by a 46-to-
48-hour infusion of 5FU at home using an ambulatory
pump. This obviates the need for hospitalisation and
reducing bed occupancy in day centres, which could
help to reduce hospital workload and related costs.[3] The
number of saved inpatient bed days is at least 2 days per
cycle of FOLFOX/FOLFIRI. This could make a large
impact given the accumulating numbers of patients
requiring this treatment. Increasing day chemotherapy
attendance for home chemotherapy infusion has been
demonstrated with the implementation of the ambulatory
home chemotherapy programme at an oncology centre.[17]
Reduced inpatient and outpatient bed occupancy
enables hospital beds to be reallocated to patients with
a greater need for inpatient care, such as those requiring
more intensive care, palliative care, or chemotherapy
treatments not indicated for home infusion.
Home chemotherapy has been increasingly employed
in oncology centres that have been able to establish
adequate logistics and technical support, and staff
training. A study conducted between 2017 and 2019
involving 24 cancer patients at Pamela Youde Nethersole
Eastern Hospital[18] described the authors’ experience
with home ambulatory chemotherapy using elastomeric
infusion pumps. They concluded that home ambulatory
chemotherapy is safe and effective, that patients enjoy
high levels of satisfaction during treatment, and that such
a valuable service should be promoted more liberally in
hospitals to improve the quality of patient service.
Home Chemotherapy Infusion for Advanced
Cancers
Chemotherapy remains the mainstay treatment for patients with advanced malignancy in developed
countries. Patients with advanced cancer survive longer,
have more treatment options, and adhere to treatment
much longer on new generations of chemotherapy,
targeted therapy, and immunotherapy than they did
before. Home-based oncological care is generally
reserved for end-of-life patients in Hong Kong. Because
management of chemotherapy-related side-effects
has improved and new, safe treatment schedules and
administration tools have been introduced, home-based
chemotherapy is becoming a valid alternative to hospital-based
treatment for patients with advanced cancers.
Additionally, with hospitalisation, patients tend to
participate less in their own care and are less ambulant
because of the lack of spacing, thus disrupting the patients’
normal daily hygiene and exercise routine. Patients with
advanced cancer, who are at particularly high risk for
nosocomial infections[19] and thromboembolism,[20] tend to
benefit tremendously from home-based chemotherapy,
as those conditions are likely to be exacerbated by
hospitalisation. In addition, many patients prefer to
spend time with their families rather than in hospitals.
In 2018, a survey of 22 patients with metastatic
colorectal or pancreatic cancers receiving 5FU-based
home infusion revealed a high level of satisfaction in
the patient group.[17] Two of the patients encountered
minor equipment troubles during one treatment cycle,
which were solved before they left the hospital. None
experienced adverse events during chemotherapy
infusion at home. Moreover, advantages expressed by
the patients and their caregivers included the ability to
continue many daily activities and to participate in their
own care, giving them a greater sense of control over
their treatment.
CORE ELEMENTS OF
IMPLEMENTING AMBULATORY
HOME CHEMOTHERAPY
Multidisciplinary Collaboration
The outpatient and home settings are not necessarily
panaceas for cost savings and efficiency because of
the growing number of toxic treatments and complex
interventions. The emphasis must be on high-quality
multidisciplinary collaboration, especially in high-volume
centres.
Multidisciplinary collaboration is crucial for the provision
of ambulatory home chemotherapy to patients. Smooth
service delivery requires the establishment of protocols and guidelines that provide a well-structured mechanism
with clearly defined workflow involving oncologists,
vascular surgeons, nurses and pharmacists, together with
good communication among team members.
The most common problems during chemotherapy
delivered via peripheral cannulation are thrombophlebitis
and pain. Reliable central venous access is crucial for
patients who need continuous infusion of chemotherapy at
home. To facilitate home chemotherapy, implantation of
a central venous catheter is needed to allow concentrated
drugs to directly enter a central vein and become rapidly
diluted by blood. This protects the peripheral blood
vessel walls from drug irritation, solving the problems of
drug extravasation and pain. Support from other teams
such as vascular surgery or interventional radiology for
placement of central venous access devices (CVADs) is
crucial for this service.
Portable Infusion Devices
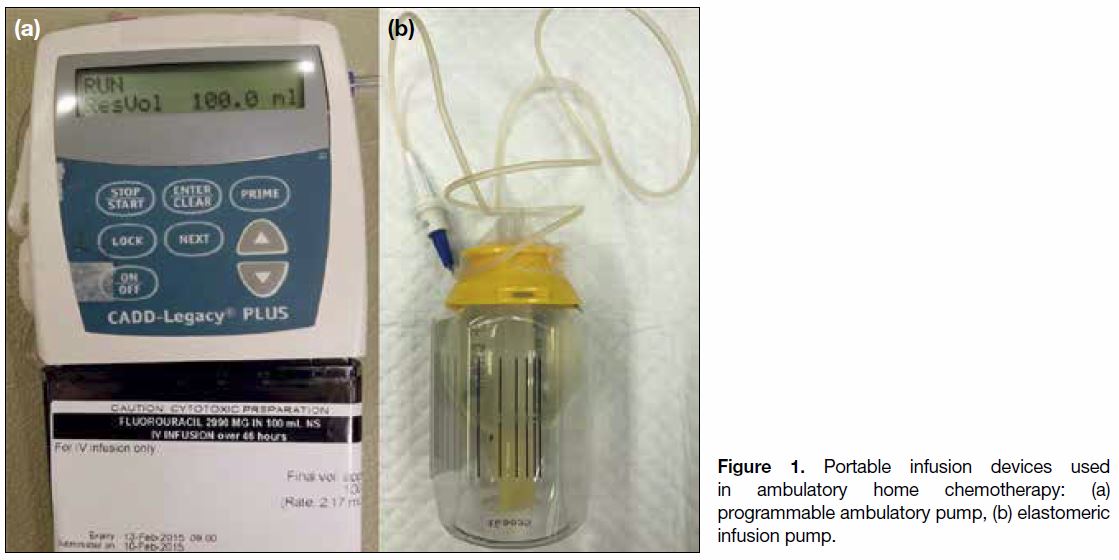
There are two types of portable infusion devices:
programmable infusion pumps (electronic) and
elastomeric infusion pumps (non-electronic) [Figure 1].
Figure 1. Portable infusion devices used in ambulatory home chemotherapy: (a) programmable ambulatory pump, (b) elastomeric infusion pump.
Electronic pumps usually operate via peristaltic
mechanisms that propel the infusion forward via
appendages that move in waves. Decimal rate values are
programmed into the pump to provide either intermittent
or continuous infusions, imparting additional flexibility
to the delivery of various medications and chemotherapy
regimens to treat many diseases and conditions, from
haematological malignancy to chronic pain. These pumps
usually contain audible and visual alarms to alert users
about errors such as occlusion, low battery status, and
pump malfunction. The programming of these pumps
is considered to be one of the procedure’s risks because
of the potential for user error. In addition, electronic
pumps are often sensitive to radiation exposure and can
result in pump malfunction for patients on concurrent
chemoirradiation therapy.[21]
Elastomeric pumps have no buttons for programming
and rely on an elastomeric membrane to generate
pressure that moves the fluid out of the membrane. The
single rate of infusion is controlled by an inline orifice
or flow restrictor. These pumps have benefits over the
electronic ones, such as minimised risks related to pump
programming, lack of noise, lightweight design, and
simplified use. However, the lack of an alarm system can
be risky. Besides, the accuracy of the infusion time can
fluctuate greatly because of factors like temperature and viscosity: one study[22] showed that 40% of elastomeric
pumps had excess solution left upon disconnection.
Neither type of pump is absolutely free of risk nor
universally fit across different regimens. Important factors
for the decision of pump type include the complexity of
chemotherapy, patients’ pump troubleshooting ability,
and the pump’s weight, availability, and cost.
Chemotherapy Nurse Training and Practice
Review
Chemotherapy nurses[23] are usually the staff members
who assess and ensure venous access and deliver
chemotherapy to patients. Appropriate pretreatment
assessment, patient education, and infusion monitoring
are critical to patients on chemotherapy. Their
duties include handling the portable infusion device,
manipulating the CVAD, troubleshooting, emergency
management, and the removal of chemotherapy
materials. Although chemotherapy nurses handle the
bulk of patient care, they also need to ensure that patients
always adhere to care and safety policies. To ensure the
smooth operation of the ambulatory home chemotherapy
service, the relevant extra training, audits, practice
review, and updates on related issues are indispensable.
Patient and Caregiver Counselling and
Education
Chemotherapy nurses are not typically present at the patient’s home throughout the infusion. To enable
patients and their caregivers to better cope with
home chemotherapy administration, assessment and
counselling are provided at the chemotherapy nurse
clinic. Topics include management of treatment-induced
side-effects and symptoms, at-home care of
the implanted CVAD and ambulatory infusion device,
simple troubleshooting, and management of emergencies
such as drug spillage or disconnection of the tubes. The
nurses also provide patients with a list of ‘do’s and don’ts’
to follow while on home chemotherapy.
The major concern raised by patients and their caregivers
has been the availability of support and consultation to
help them when they encounter problems during at-home
chemotherapy administration. Patients and caregivers
should be educated about when to call, the total dose they
are receiving, how long the infusion should last, the need
to occasionally check the remaining drug volume in the
pump, how to protect their devices while showering, and
where to position the pump and catheter while sleeping.
Importantly, a dedicated number is provided for patients
to call in case of emergencies, and a nurse from a day
centre or ward will respond anytime, even during non-office
hours, to address any enquiries about the pump.
Selection of Patient and Vascular Access
Device
Many patients receiving chemotherapy regimens involving 5FU may be eligible for home infusion
therapy. The patients or their caregivers need to have
sufficient mental and cognitive fitness and demonstrable
self-care capabilities. There is no financial means
assessment. Home chemotherapy is generally not
advisable for patients who have poor cognitive function,
learning problems, poor/unstable living environments,
or no telephone access. Elderly patients living alone are
eligible as long as they meet the aforementioned criteria
and have access to phone calls in case of emergencies.
Several factors can guide the selection of the most
appropriate CVAD for each clinical situation. If frequent
blood taking is required, a double-lumen catheter is
more appropriate. The Hickman catheter is preferred for
haematology-oncology patients. If patients require stem
cell apheresis, catheters with a wider lumen are needed.
The implantable port (Figure 2) is inserted completely
under the skin. Hence, it allows patients to carry out
normal daily activities, such as showering, more
conveniently, although it requires surgical insertion and
stitching of the incision wound. The peripherally inserted
central catheter (PICC) has the advantage that insertion
can be performed at the patient’s bedside, which provides
greater flexibility in scheduling. The PICCS are designed
to be used up to 12 months, and most PICCs may stay in
place and in use for several months.
Figure 2. Implantable port must be accessed with a non-coring needle for infusion therapy.
Patients who are prescribed chemotherapy using the
home infusion model are sent to a chemotherapy nurse
clinic for pre-chemotherapy assessment and counselling.
During pre-chemotherapy assessment at the nurse clinic,
patients are assessed on whether they understand and are
suitable for home chemotherapy.
CHALLENGES TO OVERCOME AND
MOVING FORWARD
Availability of Additional Chemotherapy
Regimens for Home Infusion Delivery
Because of the positive feedback received from patients
and the positive impact on the healthcare system of the
chemotherapy infusion at home model, the feasibility
of including more drug regimens for ambulatory
home infusion could be explored. There are other
chemotherapy agents currently under investigation for
home infusion.[15] [24]
Under the partially at-home service model, agents that are
administered over one to several days, with long stability[25]
and manageable toxicities are targeted. The most widely
used agent is 5FU, as the typical treatment runs over 46 hours or continuously with the patient’s radiation
therapy. There is room for extending 5FU home infusion
to various other disease groups in addition to colorectal
and pancreatic cancers by modifying the drug delivery
procedures of inpatient infusion regimens. One possible
example is 4-day carboplatin-5FU for gastric cancer with
the 1-hour infusion of carboplatin administered in a day
centre, followed by a 48-hour at-home infusion of 5FU,
after which patients return to the day centre to resupply
the pump for another 48-hour infusion. Another option
is 5-day cisplatin-5FU for head and neck cancer, with
the first-day regimen including 3-hour inpatient cisplatin
infusion and rigorous hydration with mannitol, followed
by a 48-hour at-home infusion of 5FU, and then repetition
of the 48-hour infusion. Trabectedin[26] is an antineoplastic
agent that could potentially be switched from inpatient to
home administration because its administration requires
prolonged infusion over 24 hours. It has relatively low
toxicity despite the fact that it is a vesicant, and the
possibility of extravasation occurring at home has been
largely prevented by CVAD pre-insertion.
Other advances have led to the development of
further generations of multiple-channel and flexibly
programmable pumps that can deliver temporally
precise patterns of chemotherapy.[27] Such pumps could allow complex chemotherapy regimens to be
switched from the inpatient to the outpatient setting.
Certain patients, especially those with support at
home, can take home several doses of chemotherapy
to be delivered by a programmable digital pump via a
central line and then return for refills. In Europe, this
change in the management of complex treatments has
reduced the number of in-hospital days.[28] Examples
of patients who can benefit from this change include
those with acute leukaemia who receive induction, re-induction,
and consolidation chemotherapy infusions
and patients with lymphoma who are conditioned with
the BEAM regimen (carmustine [BCNU], etoposide,
cytarabine and melphalan) prior to haematopoietic
stem cell transplantation. Other initiatives could also be
undertaken to encourage at-home administration of such
treatments as pump-administered antibiotics. These facts
and products have resulted in the rapid growth of a new
home-care industry.
The possibility of chemotherapy infusion at home
could be increased by calling for extra community care.
Options for improvements include provision of at-home
chemotherapy by a chemotherapy homecare nurse or
community nurse after receiving training, at community
centres, or in a mobile bus for chemotherapy care.[29] Once
the appropriate infrastructure is available, the totally at-home
model that is already popular for chemotherapy
delivery in rural areas of some Western countries (eg,
the United Kingdom, Canada) can be more widely
implemented in Hong Kong. More chemotherapy drugs
with relatively few toxicities and manageable sideeffects
could be included for administration at home or
community centres by chemotherapy nurses regardless
of infusion duration.[9]
Availability of Vascular Access Devices
Throughout the management of at-home chemotherapy
infusion, CVADs have a paramount role. The lack
of a dedicated support team to provide reliable and
adequate vascular access may be one of the reasons
why some hospitals do not offer home chemotherapy.
Besides vascular surgeons, other specialties could
also be involved in performing CVAD placement, for
example, interventional radiologists could perform PICC
insertion, and general surgeons could place implantable
ports. However, the specialties of general surgery and
radiology also face increased pressure due to elevated
demand for their services.
In many Western countries, mainland China, and Taiwan, PICC insertion is commonly done by a properly trained
nurse or PICC nurse in the day centre setting, which
can free physicians for other clinical tasks while still
maintaining quality service.[30] Compared with the other
CVAD types, insertion of a PICC is less invasive and
relatively easy to perform, mainly requiring expertise in
handling needles and guide wires and inserting catheters,
which can be imparted through supervised training.[31]
Strengthening Home Backup Support
The centres that have implemented ambulatory
home chemotherapy service in Hong Kong have not
encountered major problems so far, as the centres
continuously review and share their practices and have
taken measures to prevent potential issues. In the future,
to further expand services to more agents or regimens with
wider toxicity coverage, more intensive and structured
telephone follow-up with patients and their families is
required. Accordingly, patients are always encouraged
to get in touch over the phone if they have problems.
Further, telehealth interventions for remote monitoring
and management of chemotherapy side-effects may help
providers to connect with patients at home.[32] Moreover,
such interventions could help primary healthcare
professionals or community/home care nurses with
chemotherapy training to take on additional roles such
as monitoring, supervising therapy, or home care support.
CONCLUSION
Modern chemotherapy using the ambulatory home
infusion model became widely accepted with the
development of CVADs and portable infusion
devices. Providing sustainable service and staffing
for ambulatory home chemotherapy requires several
components. Protocol development, patient counselling,
and emergency support are necessary. Such support
should account for drug toxicity, the treatment’s
expected side-effects, and the self-care capabilities of
the patient and family. Logistics should be established
through multidisciplinary collaboration, chemotherapy
nurse clinics, expertise development, and training. The
chemotherapy infusion at home model for advanced
cancer could be further promoted and developed by
exploring at-home chemotherapy administration of
additional drugs, identifying future opportunities for work
with newer and more advanced practice foci, and training
initiatives. Such training could involve CVAD placement
and usage, telehealth system support, programmable
digital pumps for complex chemotherapy regimens, and
chemotherapy administration by chemotherapy nurses at
the patient’s home or community centre. Our future goal is to meet the needs for increasing service load and on-going
chemotherapy access to populations who need it.
REFERENCES
1. Hong Kong Cancer Registry, Hospital Authority, Hong Kong SAR
Government. Overview of Hong Kong Cancer Statistics of 2017.
Available from: https://www3.ha.org.hk/cancereg/pdf/overview/
Summary%20of%20CanStat%202017.pdf. Accessed 13 Feb 2020.
2. Hospital Authority. Hospital Authority Strategic Service
Framework for Cancer Services 2019. Available from: https://www.
ha.org.hk/haho/ho/ap/HACANCERSSF_Eng.pdf. Accessed 6 Jun
2020.
3. Joo EH, Rha SY, Ahn JB, Kang HY. Economic and patient-reported
outcomes of outpatient home-based versus inpatient hospital-based
chemotherapy for patients with colorectal cancer. Support Care
Cancer. 2011;19:971-8. Crossref
4. Corrie PG, Moody AM, Armstrong G, Nolasco S, Lao-Sirieix SH,
Bavister L, et al. Is community treatment best? A randomized trial
comparing delivery of cancer treatment in the hospital, home and
GP surgery. Br J Cancer. 2013;109:1549-55. Crossref
5. Evans JM, Qiu M, MacKinnon M, Green E, Peterson K, Kaizer L.
A multi-method review of home-based chemotherapy. Eur J Cancer
Care (Engl). 2016;25:883-902. Crossref
6. Tsui SL, Ng KF, Chan WS, Chan TY, Lo JR, Yang JC. Cancer pain
management: experience of 702 consecutive cases in a teaching
hospital in Hong Kong. Hong Kong Med J. 1996;2:405-13.
7. Grayson ML, Silvers J, Turnidge J. Home intravenous antibiotic
therapy: a safe and effective alternative to inpatient care. Med J
Aust. 1995;162:249-53. Crossref
8. Hitchcock J, Jepson AP, Main J, Wickens HJ. Establishment of an
outpatient and home parenteral antimicrobial therapy service at a
London teaching hospital: a case series. J Antimicrob Chemother.
2009;64:630-4. Crossref
9. Boothroyd L, Lehoux P. Home-based chemotherapy for cancer:
issues for patients, caregivers and the health care system.
Montreal QC: Agence d’Evaluation des Technologies et des
Modes d’Intervention en Sante (AETMIS); 2004. Available
from: https://www.inesss.qc.ca/fileadmin/doc/AETMIS/Rapports/
Cancer/2004_02_en.pdf. Accessed 11 Feb 2020.
10. Young AM, Kerr DJ. Home delivery: chemotherapy and pizza?
BMJ. 2001;322:809-10. Crossref
11. Corbett M, Heirs M, Rose M, Smith A, Stirk L, Richardson G, et al.
The delivery of chemotherapy at home: an evidence synthesis.
Southampton (UK): NIHR Journals Library; 2015. Crossref
12. Anderson H, Addington-Hall JM, Peake MD, MKendrik J, Keane K,
Thatcher N. Domiciliary chemotherapy with gemcitabine is safe and
acceptable to advanced non-small-cell lung cancer patients: results
of a feasibility study. Br J Cancer. 2003;89:2190-6. Crossref
13. Polinski JM, Kowal MK, Gagnon M, Brennan TA, Shrank WH.
Home infusion: safe, clinically effective, patient preferred, and cost
saving. Healthc (Amst). 2017;5:68-80. Crossref
14. Haute Autorité de santé. Conditions du développement de la
chimiothérapie en hospitalisation à domicile: analyse économique
et organisationnelle, Haute Autorité de Santé. mise en ligne janvier
2015 [in French]. Available from: https://www.has-sante.fr/upload/
docs/application/pdf/2015-03/conditions_du_developpement_de_
la_chimiotherapie_en_hospitalisation_a_domicile_-_rapport.pdf.
Accessed 13 Feb 2020.
15. Lüthi F, Fucina N, Divorne N, Santos-Eggimann B, Currat-Zweifel C,
Rollier P, et al. Home care — a safe and attractive alternative to inpatient administration of intensive chemotherapies. Support Care
Cancer. 2012;20:575-81. Crossref
16. Lee YM, Hung YK, Mo FK, Ho WM. Comparison between
ambulatory infusion mode and inpatient infusion mode from the
perspective of quality of life among colorectal cancer patients
receiving chemotherapy. Int J Nurs Pract. 2010;16:508-16. Crossref
17. Mak S, Yih P. Expert Opinion. Ambulatory home chemotherapy
programme — a success story. MIMS Oncology Hong Kong.
Available from: https://specialty.mims.com/topic/ambulatory-home-chemotherapy-programme-.... Accessed
11 Feb 2020.
18. Lee WM. Safety and acceptance of home ambulatory chemotherapy.
Paper presented at: Hospital Authority Convention 2019; 2019 May
14-15; Hong Kong.
19. Sydnor ER, Perl TM. Hospital epidemiology and infection control
in acute-care settings. Clin Microbiol Rev. 2011;24:141-73. Crossref
20. Eichinger S. Cancer associated thrombosis: Risk factors and
outcomes. Thromb Res. 2016;140 Suppl:S12-7. Crossref
21. Bak K, Gutierrez E, Lockhart E, Sharpe M, Green E, Costa S, et al.
Use of continuous infusion pumps during radiation treatment.
J Oncol Pract. 2013;9:107-11. Crossref
22. Salman D, Biliune J, Kayyali R, Ashton J, Brown P, McCarthy T, et al.
Evaluation of the performance of elastomeric pumps in practice:
are we under-delivering on chemotherapy treatments? Curr Med
Res Opin. 2017;33:2153-9. Crossref
23. Mak SS. Oncology nursing in Hong Kong: milestones over the past
20 years. Asia Pac J Oncol Nurs. 2019;6:10-6. Crossref
24. Lal R, Hillerdal GN, Shah RN, Crosse B, Thompsone J,
Nicolson M, et al. Feasibility of home delivery of pemetrexed in
patients with advanced non-squamous non-small cell lung cancer.
Lung Cancer. 2015;89:154-60. Crossref
25. Benizri F, Bonan B, Ferrio AL, Brandely ML, Castagné V,
Théou-Anton N, et al. Stability of antineoplastic agents in use
for home-based intravenous chemotherapy. Pharm World Sci.
2009;31:1-13. Crossref
26. Schöffski P, Cerbone L, Wolter P, De Wever I, Samson I, Dumez
H, et al. Administration of 24-h intravenous infusions of trabectedin
in ambulatory patients with mesenchymal tumors via disposable
elastomeric pumps: an effective and patient-friendly palliative
treatment option. Onkologie. 2012;35:14-7. Crossref
27. Hrushkesky WJ. Home-based circadian-optimized cancer
chemotherapy. In: Berner B, Dinh SM, editors. Electronically
Controlled Drug Delivery. Florida: CRC Press; 2019. p 9-46. Crossref
28. Fridthjof KS, Kampmann P, Dünweber A, Gørløv JS, Nexø C,
Friis LS, et al. Systematic patient involvement for homebased
outpatient administration of complex chemotherapy in acute
leukemia and lymphoma. Br J Haematol. 2018;181:637-41. Crossref
29. Chu H. Is Hong Kong ready for home chemotherapy? MIMS
Oncology Hong Kong. 13 Dec 2016. Available from: https://today.
mims.com/is-hong-kong-ready-for-home-chemotherapy. Accessed
17 Feb 2020.
30. Walker G, Todd A. Nurse-led PICC insertion: is it cost effective?
Br J Nurs. 2013;22(19 Suppl):S9-15. Crossref
31. Jenkins LC. PICC nurses in practice. Radiology Today Magazine.
2009;10:5.
32. Breen S, Ritchie D, Schofield P, Hsueh YS, Gough K, Santamaria N,
et al. The Patient Remote Intervention and Symptom Management
System (PRISMS) — a Telehealth-mediated intervention enabling
real-time monitoring of chemotherapy side-effects in patients with
haematological malignancies: study protocol for a randomised
controlled trial. Trials. 2015;16:472. Crossref