Percutaneous Repair of Inadvertent Brachiocephalic Arterial Puncture by Closure Device: A Case Report
CASE REPORT
Percutaneous Repair of Inadvertent Brachiocephalic Arterial Puncture by Closure Device: A Case Report
KTF Ng, CM Chau, HF Chan, LF Cheng, KF Ma, KM Chan
Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong
Correspondence: Dr KTF Ng, Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong. Email: ntf808@ha.org.hk
Submitted: 24 May 2019; Accepted: 29 Jul 2019.
Contributors: All authors contributed to the concept and design of the study, acquisition and interpretation of the data, drafting of the manuscript,
and critical revision of the manuscript for important intellectual content. All authors had full access to the data, approved the final version for
publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Funding/Support: This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: The patient was treated in accordance with the Declaration of Helsinki. The patient suffered from cognitive impairment after the traumatic event. Verbal consent was obtained from the patient’s sister.
INTRODUCTION
Central venous catheter (CVC) insertion is a common
bedside procedure and essential to the management of
critically ill patients. However, placement of a CVC is
not without risk, as a multitude of complications may
present during or after the procedure.[1] Accidental arterial
puncture is a common but serious complication during
CVC insertion. Timely detection and prompt vascular
repair may prevent potentially fatal complications
including active haemorrhage or cerebrovascular
thromboembolic events. We report a case of inadvertent
arterial puncture during CVC placement followed by
successful percutaneous repair using a suture-mediated
closure device.
CASE REPORT
A 65-year-old woman was admitted in a coma to our
hospital via the emergency department following a road
traffic accident. She had sustained multiple injuries
including a severe head injury, multiple rib fractures,
and pelvic fractures. Emergency surgery was performed
and the patient was transferred to the intensive care
unit for further management. Insertion of a 7-Fr CVC
was attempted through the subclavian vein. However,
following insertion, the return flow was noted to be pulsatile, and inadvertent arterial puncture was suspected.
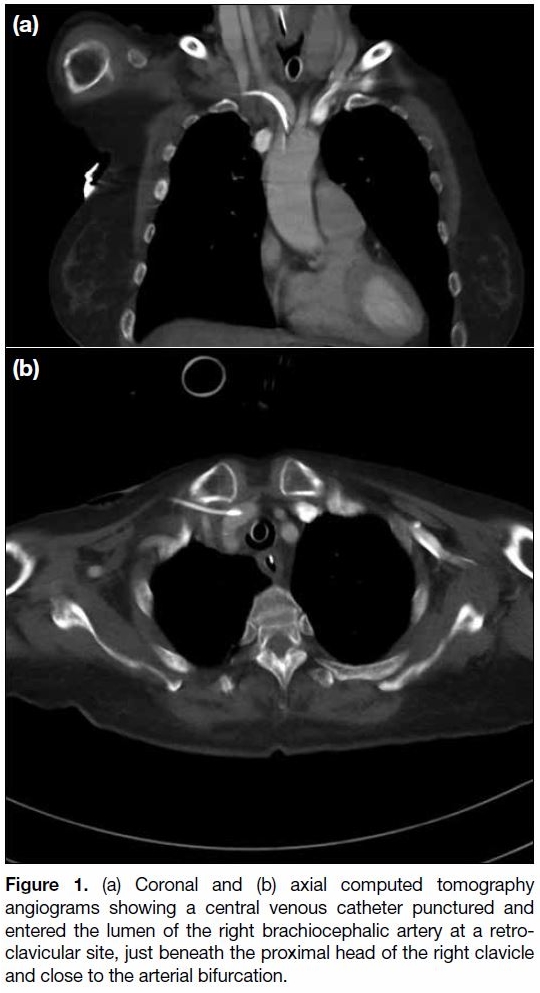
On computed tomography angiogram, the right
brachiocephalic artery was punctured by the CVC at a
retro-clavicular site, just beneath the proximal head of
the right clavicle and close to the arterial bifurcation
(Figure 1). It travelled retrogradely with the tip reaching
the origin of the artery at the aortic arch. No hematoma
or pseudoaneurysm was detected. Arterial flow was
preserved in the right brachiocephalic, vertebral and
subclavian arteries.
Figure 1. (a) Coronal and (b) axial computed tomography
angiograms showing a central venous catheter punctured and
entered the lumen of the right brachiocephalic artery at a retroclavicular
site, just beneath the proximal head of the right clavicle
and close to the arterial bifurcation.
The patient was transferred to a hybrid operating theatre
for fluoroscopic-guided intervention. The patient
underwent general anaesthesia. The right upper anterior
chest wall, right neck and bilateral groin regions were
prepared aseptically.
The CVC insertion site over the right upper chest wall was
dissected down and a 0.035-inch Glidewire® (Terumo,
Tokyo, Japan) was inserted through the right subclavian
catheter lumen. The CVC was then replaced with an 11-cm 6-Fr vascular sheath over the guidewire, securing the
vascular access.
Additional vascular accesses were created in both groins.
A 7-Fr and a 4-Fr sheath were inserted into the right
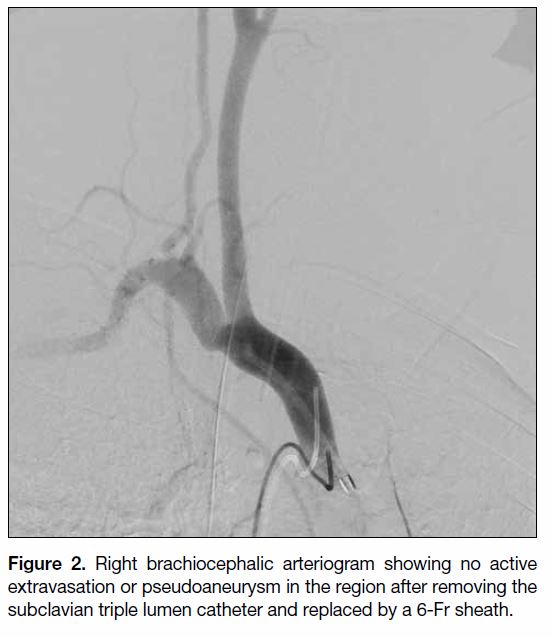
and left femoral artery, respectively. Left vertebral and
right brachiocephalic arteriograms were performed for
procedure planning, showing: (1) no active extravasation
or pseudoaneurysm in the innominate angiogram after
removal of the subclavian triple lumen catheter (Figure 2);
(2) right brachiocephalic artery, right subclavian artery,
right vertebral artery, and right common carotid artery
were patent without filling defects or dissections, and
(3) basilar artery was adequately supplied by the left
vertebral artery.
Figure 2. Right brachiocephalic arteriogram showing no active
extravasation or pseudoaneurysm in the region after removing the
subclavian triple lumen catheter and replaced by a 6-Fr sheath.
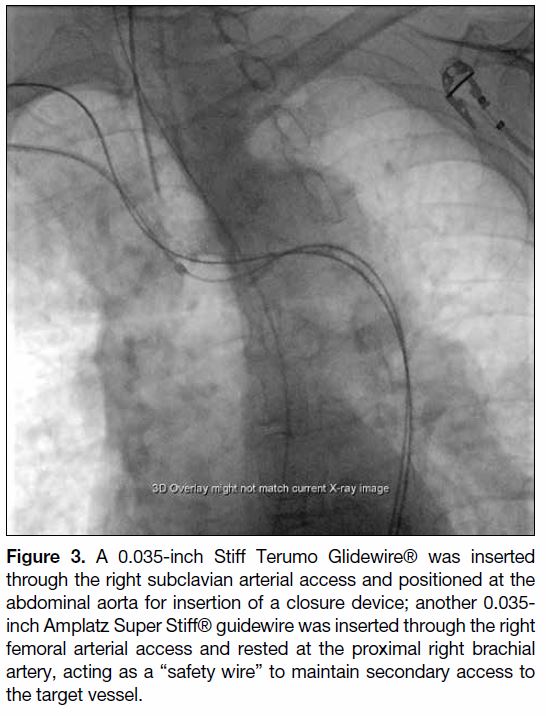
A 0.035-inch Stiff Terumo Glidewire® was inserted
through the right subclavian arterial access and positioned
at the abdominal aorta with the help of a 4-Fr catheter. Another 0.035-inch Amplatz Super Stiff® guidewire
(Boston Scientific, Marlborough [MA], United States)
was inserted through the right femoral arterial access and
rested at the proximal right brachial artery, with the help
of a 4-Fr catheter, acting as a “safety wire” to maintain
secondary access to the target vessel (Figure 3).
Figure 3. A 0.035-inch Stiff Terumo Glidewire® was inserted
through the right subclavian arterial access and positioned at the
abdominal aorta for insertion of a closure device; another 0.035-inch Amplatz Super Stiff® guidewire was inserted through the right
femoral arterial access and rested at the proximal right brachial
artery, acting as a “safety wire” to maintain secondary access to
the target vessel.
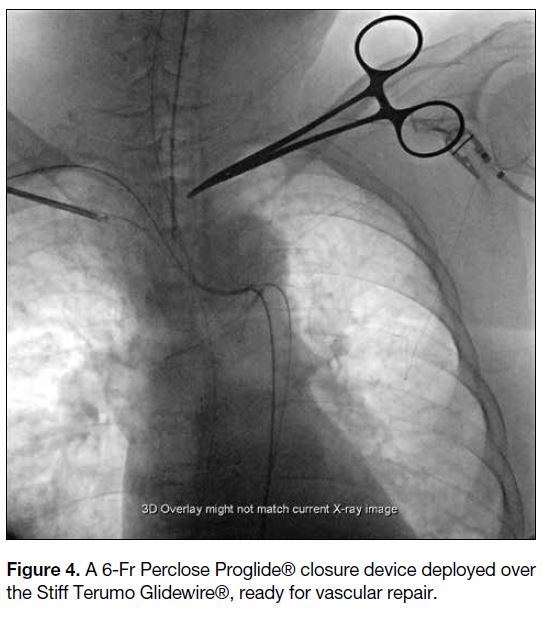
With guidewires confirmed in place, the 6-Fr sheath
at the right subclavian artery was removed and a 6-Fr
Perclose Proglide® (Abbott Vascular, Redwood [CA],
United States) closure device was deployed over the
Stiff Terumo Glidewire® (Figure 4). Subsequent right
subclavian angiogram confirmed successful repair of
the vessel with no extravasation, pseudoaneurysm or
stricture (Figure 5).
Figure 4. A 6-Fr Perclose Proglide® closure device deployed over the Stiff Terumo Glidewire®, ready for vascular repair.
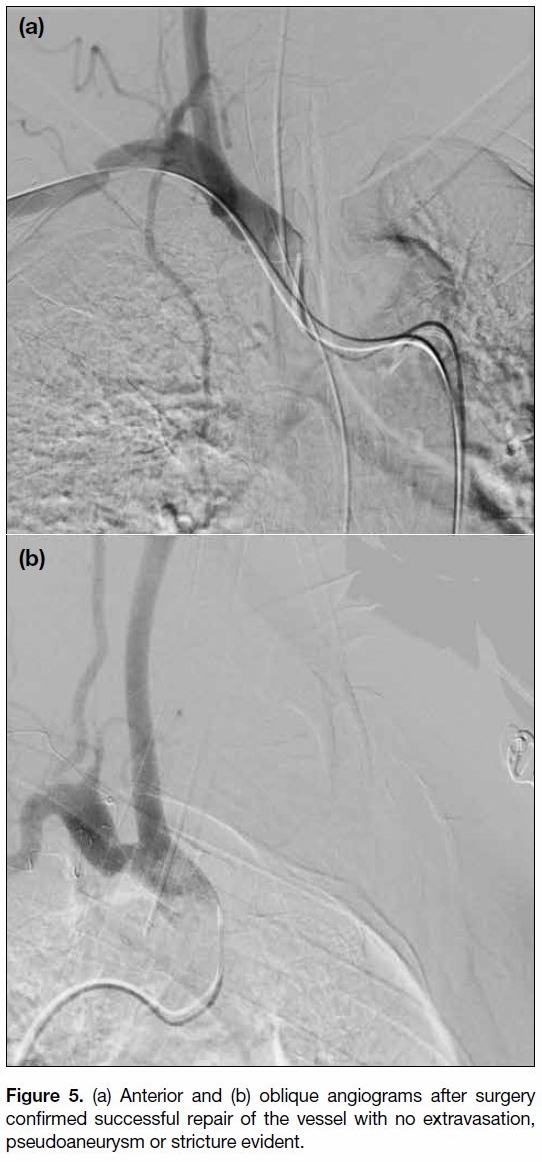
Figure 5. (a) Anterior and (b) oblique angiograms after surgery
confirmed successful repair of the vessel with no extravasation,
pseudoaneurysm or stricture evident.
DISCUSSION
CVC insertion is an essential procedure in the
management of a critically ill patient. Accidental arterial
puncture is a known complication with potentially
fatal outcomes including active haemorrhage or
cerebrovascular thromboembolic events. The incidences
of arterial puncture are about 1% and 2.7% for CVC
insertion through the jugular and subclavian veins,
respectively.[2] [3] CVC insertion under ultrasound guidance
can reduce but not completely eliminate the risk.[4] [5] [6] [7]
Where puncture occurs, treatment options include open
surgical repair, placement of a stent-graft across the puncture site, or repair of the arterial puncture with a
percutaneous closure device. Additional application
of intra-arterial balloon for temporary tamponade is
optional. Open surgical repair may pose greater risk
in a critically ill patient with poor premorbid state.
Placement of a stent-graft is a promising treatment with
good success rate as high as 94% to 100%.[8] Use of a
percutaneous closure device is another convenient and
readily available option.
These treatment options were evaluated for treatment
planning in our case. Considering the relatively deep
and central puncture site at a retroclavicular site at
the brachiocephalic artery, direct compression was
not possible. A deep and extensive incision might be
needed to expose the puncture site for surgical repair,
with the risk of partial clavicular resection or need for
conversion to thoracotomy for adequate exposure. Such
major surgery may have posed high surgical risk and
was deemed unsuitable for a fragile patient with multiple
injuries. We therefore adopt a percutaneous approach for
catheter removal with vascular repair performed using
a suture-mediated closure device. The procedure was
arranged in a hybrid operating theatre equipped with
digital subtraction angiography, where conversion to
open surgery was feasible if necessary.
One advantage of a suture-mediated closure device is that
it involves only suture lines with minimal intraluminal
material, so reducing any risk of dislodgement or distal
vascular thromboembolic event. Secondly, in case of
initial suture failure to anchor or achieve only partial
haemostasis, additional sutures can be deployed along the
guidewire that remains in place throughout the procedure.
Use of a percutaneous closure device has been approved
in the closure of femoral arterial puncture, and has been
proven to be a safe and reliable method with additional
benefits of earlier haemostasis and patient mobilisation.[9]
As the femoral artery locates more superficially than the
brachiocephalic artery, we slightly dissected and dilated
the CVC insertion tract to advance the relatively soft and
flexible insertion tip of the closure device, which was
designed for a more superficial structure, into the deep
puncture site. Use of a percutaneous closure device for
subclavian arterial puncture repair is yet to be approved
and still considered off-label use. However, some
successful cases of subclavian artery puncture repair
of various diameters solely with percutaneous closure
devices or in conjunction with a balloon catheter have
been reported.[10] [11] [12] [13]
In view of the centrally located puncture, any failed
haemostasis could lead to rapid, massive and fatal
haemomediastinum, compromising the cardiovascular
system. Therefore we retained a “safety wire” across
the puncture site, running from the site of femoral
assess to the proximal right brachial artery, throughout
the procedure until haemostasis was confirmed on final
angiogram. In case of failed haemostasis by the closure
device, a balloon catheter could be rapidly deployed
along the “safety wire” for immediate haemostasis and a covered stent could also be deployed.
The option of stent-graft repair may be considered if the
punctured artery needs to be preserved. However, in our
case, the puncture site was so close to the origin of the
right subclavian and common carotid arteries in order to
preserve blood flow to both major arteries, two stents had
to be placed in a kissing fashion with each stent landed
in each of the major arteries. Secondly, since the right
vertebral artery arose at the proximal right subclavian
artery, the arterial supply to the former would likely
be compromised if the stent-graft were in place. These
technical factors increased procedure complexity and in
turn increased the risk of neurovascular complications.
In addition, the need for antiplatelet therapy following
stent-graft placement was a clinical dilemma. Without
antiplatelet therapy, the stent-graft could be easily
thrombosed, resulting in cerebral infarct or upper limb
ischaemia; yet antiplatelet therapy could increase the
intracranial bleeding risk in our patient with recent
head trauma. Under these circumstances, stent-graft
repair was considered less favourable than use of a
closure device repair. However, the option of stent-graft
repair remained in case of closure device failure.
As deployment of a stent graft at the right subclavian
artery might impair right vertebral artery perfusion, a
complete cerebral angiogram was performed before the
vascular repair to assess the patency of bilateral carotid
and vertebral arteries, as well as to look for potential
collateral supplies.
We successfully repaired the 7-Fr subclavian arterial
puncture with application of one suture across the site
using a suture-mediated percutaneous closure device.
Temporary control of blood flow with tamponade effect
by a balloon catheter is a useful adjunct during repair
with a closure device.
CONCLUSION
We report successful repair of an inadvertent subclavian artery puncture by a 7-Fr CVC using a percutaneous
closure device. With increased experience and success
rates of using percutaneous closure devices, this
technique may become a promising treatment for
subclavian arterial puncture. We await further clinical
data.
REFERENCES
1. Kornbau C, Lee KC, Hughes GD, Firstenberg M. Central line
complications. Int J Crit Illn Inj Sci. 2015;5:170-8. Crossref
2. Iovino F, Pittiruti M, Buononato M, Lo Schiavo F. Central venous catheterization: Complications of different placements [in French].
Ann Chir. 2001;126:1001-6. Crossref
3. Szkup PL. A minimally invasive technique for closing an iatrogenic
subclavian artery cannulation using the Angio-Seal closure device:
Two case reports. J Med Case Rep. 2012;6:82. Crossref
4. Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound
guidance for placement of central venous catheters: A meta-analysis
of the literature. Crit Care Med. 1996;24:2053-8. Crossref
5. Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley
C, et al. Ultrasonic locating devices for central venous cannulation:
meta-analysis. BMJ. 2003;327:361. Crossref
6. Parsons AJ, Alfa J. Carotid dissection. A complication of internal
jugular vein cannulation with the use of ultrasound. Anesth Analg.
2009;109:135-6. Crossref
7. Thompson C, Barrows T. Carotid arterial cannulation. Removing
the risk with ultrasound? Can J Anaesth. 2009;56:471-2. Crossref
8. Schoder M, Cejna M, Hölzenbein T, Bischof G, Lomoschitz F,
Funovics M, et al. Elective and emergent endovascular treatment
of subclavian artery aneurysms and injuries. J Endovasc Ther. 2003;10:58-65. Crossref
9. Patel MR, Jneid H, Derdeyn CP, Klein LW, Levine GN,
Lookstein RA, et al. Arteriotomy closure devices for cardiovascular
procedures: a scientific statement from the American Heart
Association. Circulation. 2010;122:1882-93. Crossref
10. Wallace MJ, Ahrar K. Percutaneous closure of subclavian artery
injury after inadvertent catheterization. J Vasc Interv Radiol.
2001;12:1227-30. Crossref
11. Shetty SV, Kwolek CJ, Garasic JM. Percutaneous closure after
inadvertent subclavian artery cannulation. Catheter Cardiovasc
Interv. 2007;69:1050-2. Crossref
12. Chivate RS, Kulkarni SS, Shetty NS, Polnaya AM, Gala KB,
Patel PG. Percutaneous repair of iatrogenic subclavian artery
injury by suture-mediated closure device. Indian J Radiol Imaging.
2016;26:262-6. Crossref
13. Park TK, Yang JH, Choi SH. Endovascular repair using suture-mediated
closure devices and balloon tamponade following
inadvertent subclavian artery catheterization with large-caliber
hemodialysis catheter. Korean Circ J. 2016;46:584-7. Crossref