Albumin-bilirubin versus Child-Pugh Grade as a Predictor of Survival after Individualised Hypofractionated Radiotherapy for Hepatocellular Carcinoma
ORIGINAL ARTICLE
Albumin-bilirubin versus Child-Pugh Grade as a Predictor of Survival after Individualised Hypofractionated Radiotherapy for
Hepatocellular Carcinoma
CHM Ho,1 CL Chiang,1,2,3 FAS Lee,1 JCH Chan,4 CSY Yeung,1 CKK Choi,1 FCS Wong,1 SY Tung1
1 Department of Clinical Oncology, Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Department of Clinical Oncology, The University of Hong Kong, Pokfulam, Hong Kong
3 Department of Clinical Oncology, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
4 Department of Clinical Oncology, Queen Elizabeth Hospital, Jordan, Hong Kong
Correspondence: Dr CHM Ho, Department of Clinical Oncology, Tuen Mun Hospital, Tuen Mun, Hong Kong. Email: gconnie@gmail.com
Submitted: 25 Mar 2018; Accepted: 30 Jul 2018.
Contributors: CHMH, CLC, FASL, and JCHC contributed to the design of the study, acquisition of the data, analysis and interpretation of the
data, and drafting of the manuscript. All authors contributed to critical revision of the manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and
integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: This study was approved by the New Territories West Cluster Clinical Research Ethics Committee (Ref NTWC/CREC/17037).
The requirement for patient consent was waived.
Abstract
Purpose
To evaluate the ability of Child-Pugh (CP) versus albumin-bilirubin (ALBI) grade to predict overall survival
(OS) in patients with hepatocellular carcinoma (HCC) undergoing individualised hypofractionated radiotherapy
(IHRT) using stereotactic body radiotherapy (SBRT).
Methods
We retrospectively reviewed data on our patients with HCC treated with IHRT using SBRT per our
institutional protocol from May 2006 to February 2015. We collected CP and ALBI grades prior to treatment and
analysed their prognostic value for OS.
Results
A total of 174 consecutive patients were included in this study. Among them, 63% were CP grade A5 and
37% were A6. The median ALBI score was -2.39 (range, -3.61 to -1.41) with 35% grade A1 and 65% grade A2.
OS was significantly associated with ALBI grade (p = 0.015), but not with CP grade (p = 0.47). On multivariable
regression analysis, the ALBI score, tumour size, number of lesions, total biologically effective dose, presence of
portal vein thrombosis, and the presence of metastasis were shown to be independent factors for OS.
Conclusion
ALBI grade is a better predictor of survival than the CP grade in patients with HCC receiving IHRT.
Key Words: Albumins; Carcinoma, hepatocellular
中文摘要
比較白蛋白—膽紅素與Child-Pugh分級作為個體化肝細胞癌大分割
放療後存活率的預測指標
何凱文、蔣子樑、李安誠、陳俊軒、楊善如、蔡國強、黃志成、董煜
目的
評估Child-Pugh和白蛋白—膽紅素(ALBI)分級預測使用立體定向放療(SBRT)接受個體化
肝細胞癌大分割放療(IHRT)的肝細胞癌患者的總體存活率的表現。
方法
回顧分析2006年5月至2015年2月期間,根據協議使用SBRT接受IHRT治療的肝細胞癌患者數
據,並於患者接受治療前收集Child-Pugh和ALBI分級和分析它們對總體存活率的預後價值。
結果
納入174例連續患者,其中Child-Pugh分級為A5佔63%,Child-Pugh分級為A6佔37%。ALBI的
中位數評分為-2.39(介乎-3.61至-1.41),其中A1級佔35%,A2級佔65%。總體存活率與ALBI分級
顯著相關(p = 0.015),但與Child-Pugh分級無顯著差異(p = 0.47)。多變量迴歸分析顯示ALBI評
分、腫瘤大小、病灶變數量、總生物學有效劑量、門靜脈血栓形成和轉移是預測總體存活率的獨立
因素。
結論
在接受IHRT的肝細胞癌患者中,ALBI分級比Child-Pugh分級更能預測存活率。
INTRODUCTION
Most patients with hepatocellular carcinoma (HCC)
have compromised liver function due to pre-existing
liver diseases. Treatment decisions depend very much on
hepatic function as estimated by Child-Pugh (CP) grade.[1]
However, its calculation involves subjective variables.
Albumin-bilirubin (ALBI) grade is an objective test.[2]
ALBI grade has recently been shown to be better than
CP grade as a predictor of overall survival (OS) in
patients with HCC undergoing surgical resection,[3] [4]
transarterial chemoembolisation (TACE),[5] yttrium-90
radioembolisation,[5] sorafenib,[6] [7] or stereotactic ablative
radiation therapy (SBAR).[8]
In our centre, we offer patients with HCC individualised
hypofractionated radiotherapy (IHRT) with stereotactic
body radiotherapy. IHRT is administered to patients with
HCC who are not eligible for, or have failed, standard
locoregional therapy. In contrast to SBAR, which
delivers a high dose to a relatively small tumour in three
to five fractions, IHRT delivers doses to HCC that are
individualised to each patient according to the normal
tissue constraints, rather than relative to size, in five to
10 fractions. This permits more patients with HCC to
benefit from high-precision radiotherapy.
In a previous study, we investigated the predictive value
of platelet-albumin-bilirubin, ALBI, and CP scores for patients with advanced HCC receiving radiotherapy.[9]
However, to the best of our knowledge there are no
studies that have investigated the prognostic value of
ALBI grade in routine daily practice for patients with
HCC treated with IHRT. The purpose of the present
study was to compare the ability of CP versus ALBI
grade to predict OS in patients with HCC with CP grade
A5 or A6 treated with IHRT.
METHODS
Patients
Data from consecutive patients who were treated
between 2006 and 2015 with our institutional IHRT
protocol were retrospectively extracted from medical
records in Tuen Mun Hospital, Hong Kong. Those
patients who fulfilled the inclusion criteria for this
study were included for analysis. The diagnosis of HCC
was established either by biopsy or by the American
Association for the Study of Liver Diseases criteria. The
eligibility criteria for this study were: unsuitable for,
failed or refused standard local treatments (including
resection, liver transplantation, local ablation therapies);
a minimum of 700 mL of uninvolved liver; an Eastern
Cooperative Oncology Group performance score ≤2;
CP grade A5 or A6; and adequate liver function and
complete blood counts. Patients with small-volume
distant metastases were included. Patients were excluded
if they had infiltrative disease or more than five tumour nodules. There was no limit on tumour size.
Treatment and Follow-up
Different techniques of stereotactic body radiotherapy
have been used in our institution over the years.
Patients were immobilised with a customised device
(Vac-Lok™; MEDTEC, Orange City [IA], United
States). Computed tomography (CT) with multiphasic
intravenous contrast was used to define gross tumour
volume (GTV). Breath-hold CT or four-dimensional CT
(average phase or respiratory phase sorted) was used to
determine internal target volume and/or planning target
volume. Motion management was done with maximum
intensity projection, respiratory gating, active breathing
control, or abdominal compression. IHRT was delivered
using dynamic conformal arc, intensity-modulated
radiotherapy, or volumetric arc therapy. Image guidance
was done with an infrared body positioning system
(ExacTrac™; BrainLab AG, Feldkirchen, Germany) or
cone beam CT.
Our IHRT protocol divides patients into ‘favourable’
and ‘unfavourable’ groups depending on dose and
fractionation. Individuals who meet all the following
criteria are classified into the favourable group: tumour
size ≤10 cm, Eastern Cooperative Oncology Group
score 0-1, and liver volume minus GTV ≥700 mL. For
47 patients classified into the favourable group, 5-9 Gy
for six fractions was prescribed; for the other 127 patients
classified into the unfavourable group, 4 Gy for five to
10 fractions was prescribed. The dose was individualised
by normal tissue constraints, as described previously.[9]
The normal liver was allowed to receive a biological
effective dose with α/β = 3 of 30 Gy3 <40% and mean
dose <28 Gy3. Minor dose constraint violation was
allowed in patients who were not carriers of hepatitis B
or C and were without evidence of cirrhosis.
Baseline liver function data were obtained within 1 week
prior to IHRT. The ALBI score was calculated using
the formula: ALBI score = (log 10 bilirubin [μmol/L] ×
0.66) + (-0.085 × albumin [g/L]). The ALBI scores are
stratified into: ALBI grade A1 (≤-2.60); ALBI grade
A2 (>-2.60 to ≤-1.39); and ALBI grade A3 (>-1.39).
We assessed the patients weekly during IHRT, every
6 weeks after treatment, every 3 months for the first 2 years,
and every 4 months thereafter. Physical examinations
and blood tests were done at every follow-up.
Triphasic liver CT was performed every 3 months in the
first and second year, and then every 6 months.
Statistical Analyses
OS was calculated by the Kaplan-Meier curve. Log
rank test was used to compare outcomes among survival
curves for potential prognostic factors. Significant
factors in the univariate analyses (p < 0.1) were included
in the multivariable regression analyses using the Cox
proportional hazards regression model. Factors with
p < 0.05 were considered to be significant in the Cox
model.
RESULTS
Baseline Demographics and Clinic
Characteristics
A total of 174 patients undergoing IHRT for HCC were
included in this study. Patients with ALBI grade A3 were
excluded as there were only three of them. The majority
(86%) of the patients were male, and a majority (79%) of
them were hepatitis B carriers. Most (74%) patients had
Barcelona clinic liver cancer stage C disease. The median
size of the tumour was 9.8 cm (range, 2.3-25.7 cm)
and median GTV was approximately 440 mL (range,
9.2-4009 mL).
All patients in this study had CP grade A liver reserve;
63% had CP grade A5 and 37% had CP grade A6. The
median ALBI score was -2.39 (range, -3.61 to -1.41).
According to the ALBI grading system, 34.5% were
classified as grade A1, 65.5% were grade A2.
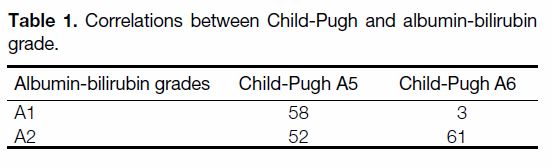
Correlation between Child-Pugh and
Albumin-bilirubin Grades
Table 1 shows the correlations between CP and ALBI
grades. Of patients with ALBI grade A1, 95% had CP
grade A5. Of patients with ALBI grade A2, 46% had CP
grade A5 and 54% had CP grade A6. Among patients
with CP grade A5, 53% were stratified into ALBI grade
A1 and 47% into ALBI grade A2. For patients with CP
grade A6, 95% had ALBI grade A2.
Table 1. Correlations between Child-Pugh and albumin-bilirubin grade.
Prognostic Factors of Overall Survival
With a median follow-up of 23.5 months (range,
2.8-136.3 months), the median OS of the entire
cohort was 24.1 months (95% confidence interval
[CI]=19.7-28.4 months). The 1-year and 2-year OS were 74.6% (95% CI=71.3-77.9%) and 50.2%
(95% CI=46.4%-54.0%), respectively.
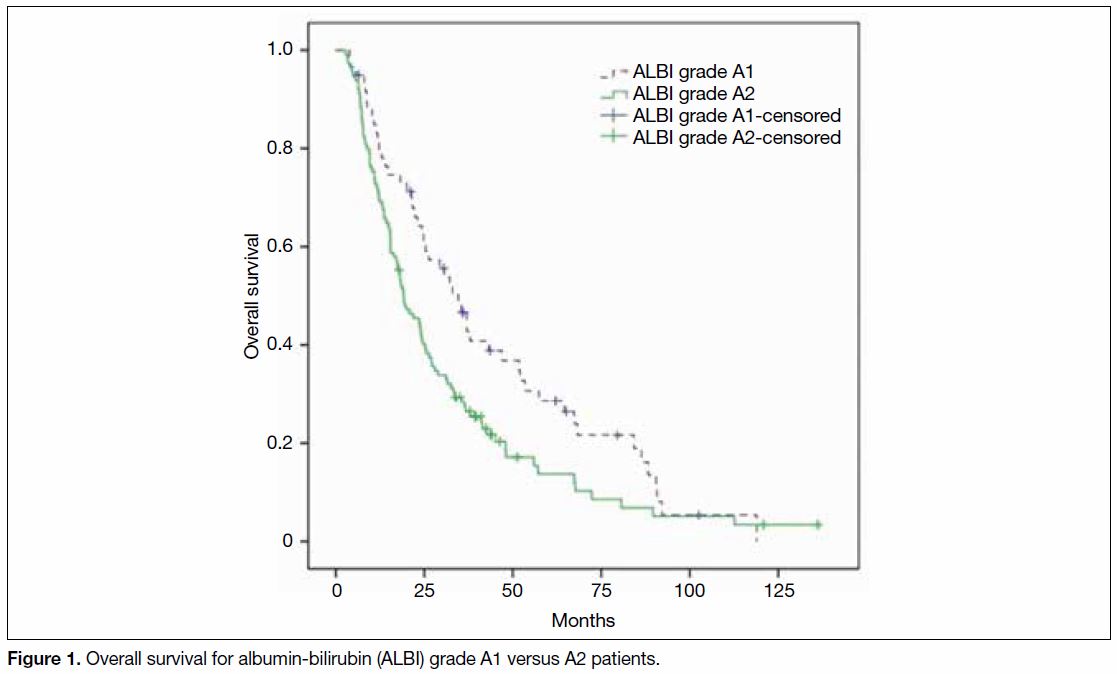
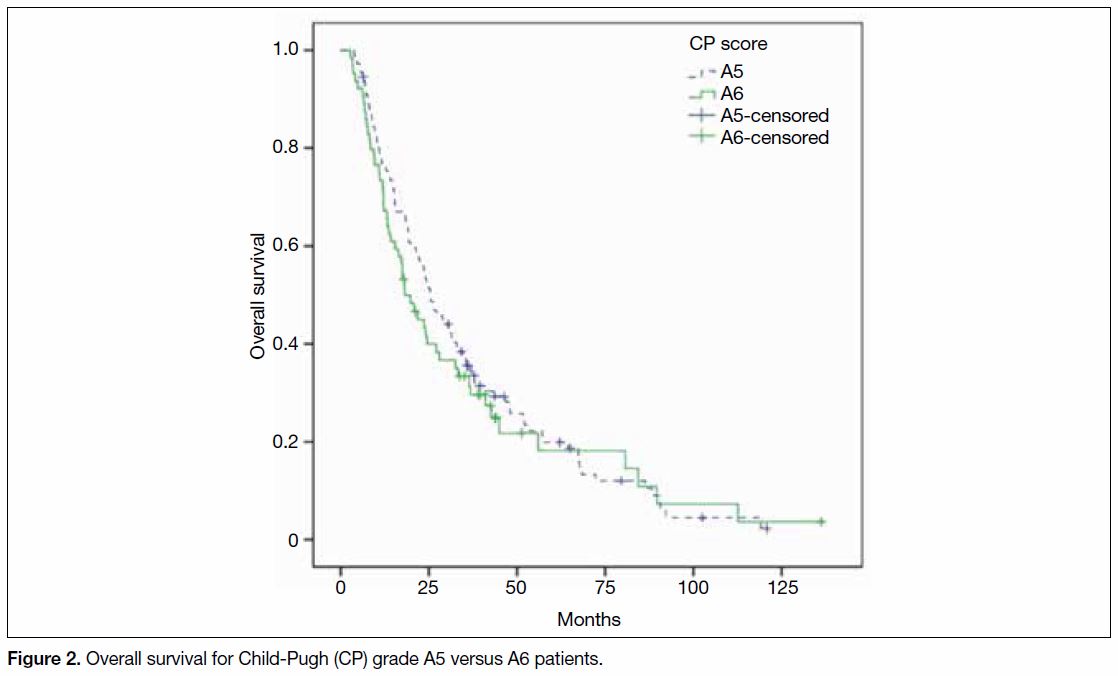
Figures 1 and 2 show the OS of our patients in terms of ALBI and CP grades, respectively.
Pretreatment ALBI grade stratified patients into
distinct survival cohorts with a median OS of
34.7 months (95% CI=25.6-43.7 months) for grade A1 versus 19.2 months (95% CI=13.9-24.3 months)
for grade A2 (p = 0.015). For CP classified patients,
the median OS for CP grade A5 was 25.4 months
(95% CI=20.4-30.4 months) and for CP grade A6 was
18.2 months (95% CI=14.0-24.2 months). The difference
was not significantly different (p = 0.467).
Figure 1. Overall survival for albumin-bilirubin (ALBI) grade A1 versus A2 patients.
Figure 2. Overall survival for Child-Pugh (CP) grade A5 versus A6 patients.
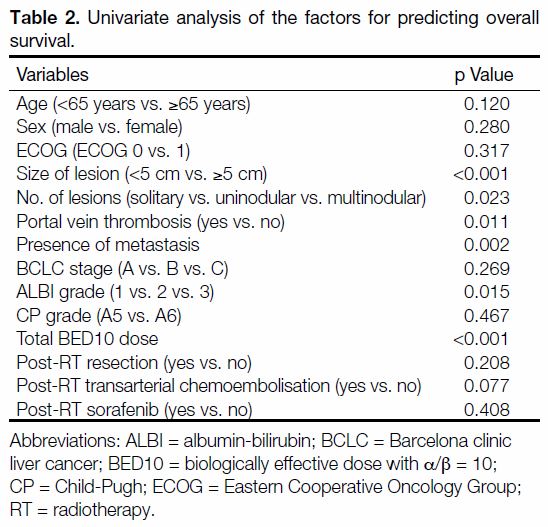
In the univariate analysis for the OS, the ALBI grade,
tumour size, number of lesions, presence of portal
vein thrombosis, presence of metastases, and the total
biological effective dose with α/β = 10 were significantly
associated with OS (Table 2). CP score was not a
significant factor.
Table 2. Univariate analysis of the factors for predicting overall survival.
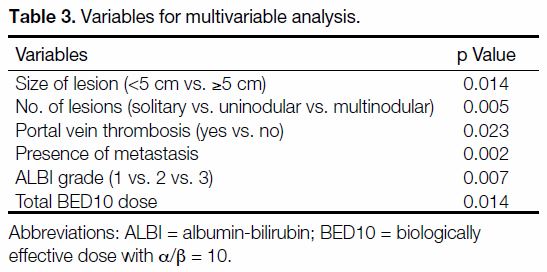
In the multivariable analysis for OS, pretreatment ALBI
score (p = 0.007) remained a significant independent
factor in predicting OS. Other significant factors
included: size of lesion (p = 0.014), number of lesions
(p = 0.005), presence of portal vein thrombosis
(p = 0.023), presence of metastasis (p = 0.002), and total
dose of radiotherapy (BED with α/β = 10, p = 0.014;
Table 3).
Table 3. Variables for multivariable analysis.
DISCUSSION
In this study, we investigated the CP versus ALBI grade
in patients with HCC treated with IHRT. Our data
showed that patients with CP grade A5 were stratified
almost equally by ALBI into grades A1 and A2. For
patients with CP grade A6, the majority were classified
as ALBI grade A2. In contrast, nearly all patients with
ALBI grade A1 had CP grade A5. Patients with ALBI
grade A2 were roughly distributed equally between CP
grades A5 and A6.
In the OS analysis, this study demonstrated that the
median OS of patients with ALBI grade A1 (35 months)
almost doubled that of patients with ALBI grade A2
(19 months). Conversely, the median OS difference
between CP grade A5 (25 months) and CP grade A6
(18 months) was not significant. In multivariable
regression analysis, ALBI was shown to be an
independent predictor of OS, whereas CP was not.
This indicates that ALBI grade is a significantly better
predictor of OS than CP.
Our findings that ALBI is superior to CP in predicting
survival are consistent with the current evidence of
ALBI grade as a predictor of survival for other HCC
treatments, including surgical resection,[3] [4] TACE,
yttrium-90 radioembolisation,5 sorafenib,[6] [7] and SBAR.[8]
In the study by Wang et al[4] that evaluated the prognostic performance of ALBI versus CP after liver resection
and the study by Lo et al[8] on SBAR, both demonstrated
no significant differences in OS between CP grades A5
and A6. Their findings were consistent with our data,
although the patient and tumour characteristics, as well
as treatments, were different. The result of this study
may help to stratify patients with CP grade A5 into two
distinct prognostic groups using ALBI. A prospective
study will likely give a more definitive result for ALBI
to be used in daily practice.
The present study had some limitations. The retrospective
design of this study is prone to selection bias. Also, the
different doses may have an effect on OS. We have
strived to make this study a valuable one by including
all consecutive eligible patients, which resulted in a
relatively large sample size, a long follow-up period, and
a long recruitment period of nearly a decade. Toxicities
were not included in the analysis owing to the fact that
grade ≥3 toxicities (prospectively collected) were very
rare, and no radiation-induced liver disease occurred.
In conclusion, our findings suggest that ALBI grade is
a better predictor of OS than the CP grade in patients
with HCC who receive IHRT. A prospective study is
recommended in order to validate the use of ALBI grade
in daily practice.
REFERENCES
1. Child CG, Turcotte JG. Surgery and portal hypertension. Major
Probl Clin Surg. 1964;1:1-85.
2. Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M,
Reeves HL, et al. Assessment of liver function in patients with
hepatocellular carcinoma: a new evidence-based approach — the
ALBI grade. J Clin Oncol. 2015;33:550-8. Crossref
3. Toyoda H, Lai PB, O’Beirne J, Chong CC, Berhane S, Reeves H,
et al. Long-term impact of liver function on curative therapy for
hepatocellular carcinoma: application of the ALBI grade. Br J
Cancer. 2016;114:744-50. Crossref
4. Wang YY, Zhong JH, Su ZY, Huang JF, Lu SD, Xiang BD, et al.
Albumin-bilirubin versus Child-Pugh score as a predictor of
outcome after liver resection for hepatocellular carcinoma. Br J
Surg. 2016;103:725-34. Crossref
5. Hickey R, Mouli S, Kulik L, Desai K, Thornburg B, Ganger D,
et al. Independent analysis of albumin-bilirubin grade in a
765-patient cohort treated with transarterial locoregional therapy
for hepatocellular carcinoma. J Vasc Interv Radiol. 2016;27:795-
802. Crossref
6. Ogasawara S, Chiba T, Ooka Y, Suzuki E, Kanogawa N, Saito T,
et al. Liver function assessment according to the albumin-bilirubin
(ALBI) grade in sorafenib-treated patients with advanced
hepatocellular carcinoma. Invest New Drugs. 2015;33:1257-62. Crossref
7. Edeline J, Blanc JF, Johnson P, Campillo-Gimenez B, Ross P,
Ma YT, et al. A multicentre comparison between Child Pugh and
albumin-bilirubin scores in patients treated with sorafenib for
hepatocellular carcinoma. Liver Int. 2016;36:1821-8. Crossref
8. Lo CH, Liu MY, Lee MS, Yang JF, Jen YM, Lin CS, et al.
Comparison between Child-Turcotte-Pugh and albumin-bilirubin
scores in assessing the prognosis of hepatocellular carcinoma after
stereotactic ablative radiation therapy. Int J Radiat Oncol Biol Phys.
2017;99:145-52. Crossref
9. Ho CH, Chiang CL, Lee FA, Choi HC, Chan JC, Yeung CS, et al.
Comparison of platelet-albumin-bilirubin (PALBI), albuminbilirubin
(ALBI), and Child-Pugh (CP) score for predicting of
survival in advanced HCC patients receiving radiotherapy (RT).
Oncotarget. 2018;9:28818-29. Crossref