Incidental Focal Colonic Uptake of 18F-fluorodeoxyglucose on Positron Emission Tomography/Computed Tomography: Its Incidence and Clinical Significance
ORIGINAL ARTICLE
Incidental Focal Colonic Uptake of 18F-fluorodeoxyglucose on
Positron Emission Tomography/Computed Tomography:
Its Incidence and Clinical Significance
YH Hui, BT Kung, TK Au Yong
Department of Nuclear Medicine, Queen Elizabeth Hospital, Hong Kong
Correspondence: Dr YH Hui, Department of Nuclear Medicine, Queen Elizabeth Hospital, Hong Kong. Email: yancol82@yahoo.com.hk
Submitted: 15 Oct 2018; Accepted: 18 Dec 2018.
Contributors: YHH and BTK designed the study. YHH acquired the data, analysed the data, and wrote the manuscript. All authors critically
revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: As editors of the journal, YH Hui and TK Au Yong were not involved in the peer-review process. Other authors have
declared no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethics Approval: This study was approved by the Kowloon Central Cluster/Kowloon East Cluster Research Ethics Committee (Ref KCC/KEC-
2018-0253). The need for patient consent was waived owing to the retrospective nature of the study.
Declaration: The results of the present study were presented in part at the 23rd Annual Scientific Meeting of the Hong Kong College of
Radiologists, Hong Kong on 14-15 November 2015 and the 12th Asia Oceania Congress of Nuclear Medicine and Biology, Yokohama, Japan
on 5-7 October 2017.
Abstract
Objective
To determine the incidence and clinical significance of incidental focal colonic 18F-fluorodeoxyglucose
(FDG) activity.
Methods
A retrospective review of data of 1851 patients who underwent FDG positron emission tomography/computed tomography (PET/CT) imaging in a clinical PET centre, Queen Elizabeth Hospital, from January 2013
to June 2013, was performed. Patients with incidental focal colonic FDG activity mentioned in the PET/CT report
with subsequent colonoscopy or surgery within 120 days were included. Patients with uptake corresponding to known
colorectal carcinoma were excluded. Using the electronic patient record system, basic demographic information,
medical history, and subsequent investigation, as well as endoscopic and histological findings, if any, were reviewed.
Results
We found 88 patients (4.8%) with 93 uptake foci. Forty-three of them had subsequent colonoscopy and
five of them had undergone surgery. In all, 38 patients with 41 foci had positive endoscopic or surgical findings.
Statistically significant differences in maximum standardised uptake values (SUVmax) between benign and malignant
groups, and between benign and premalignant groups, were found. The receiver operating characteristic curve of
SUVmax for benign versus premalignant lesions had an area under the curve of 0.852, with an optimal cut-off value
of 7.5 (sensitivity 78.8%; specificity 87.5%).
Conclusion
The incidence of incidental focal colonic FDG activity was 4.8%. The SUVmax for premalignant
and malignant lesions was significantly higher than for benign ones. Because of the high positive predictive value,
incidental focal colonic FDG uptake should always be reported and investigated without delay, especially with
SUVmax ≥7.5.
Key Words: Colonic neoplasms; Electronic health records; Fluorodeoxyglucose F18; Incidental findings; Positron-emission
tomography
中文摘要
PET/CT意外探測到直結腸局灶性FDG攝取:發病率和臨床意義
許殷豪、龔本霆、歐陽定勤
目的
研究18氟—脫氧葡萄糖正電子電腦掃描(18F-FDG PET/CT)檢查時意外探測到直結腸局灶性FDG攝取的發病率和臨床意義。
方法
回顧分析2013年1月至2013年6月於伊利沙伯醫院臨床PET中心接受18F-FDG PET/CT檢查的患者
共1851例。納入PET/CT檢查時意外探測到直結腸局灶性FDG攝取後120天內進行結腸鏡檢查或手術
的患者並排除已知結直腸癌的患者。研究透過醫院的電子病歷系統對基本人口統計信息、病史和後
續調查進行回顧分析。部份患者有內鏡和組織學檢查結果。
結果
1851例中確定88例(4.8%)共93個攝取灶,其中43人隨後接受結腸鏡檢查,5人接受手術。38
例共41個攝取灶經內鏡或手術檢查診斷為陽性。良性和惡性病變組,以及良性和惡性前期病變組之
間的最大標準攝取值(SUVmax)有統計學差異。SUVmax對良性和惡性前期病變的ROC曲線下面積
為0.852,最佳臨界值為7.5(敏感性和特異性分別為78.8%和87.5%)。
結論
這項研究顯示意外探測到直結腸局灶性FDG攝取的發病率為4.8%。惡性和惡性前期病變的SUVmax明顯高於良性病變。由於陽性預測值高,當意外探測到直結腸局灶性FDG攝取,尤其當SUVmax為7.5或以上時應盡快作進一步檢查。
INTRODUCTION
Whole-body 18F-fluorodeoxyglucose (FDG) positron
emission tomography/computed tomography (PET/CT)
has been increasingly used for oncologic purposes,
including diagnosis, staging, restaging, and treatment
monitoring.[1] Incidental bowel FDG uptake is commonly
noted.[2] [3] These uptakes can represent physiologic,
inflammatory or neoplastic changes.[4] Although a
diffuse pattern of FDG uptake in bowel is considered
physiologic, information on the nature and clinical
significance of focal patterns of FDG activity in bowel
is limited.[5] [6] To date, the incidence of focal colonic FDG
activity found on clinical FDG PET/CT in Hong Kong
has not been reported. The purpose of this study was to
determine the incidence of incidental focal colonic FDG
activity and its clinical significance as well as the clinical
utility of uptake intensity for discriminating benign from
malignant or premalignant pathology.
METHODS
The electronic medical record data of all 1851 consecutive
patients who had undergone whole-body FDG PET/CT
in Queen Elizabeth Hospital, Hong Kong, during the
period January 2013 to June 2013 were retrospectively
reviewed. Those patients with incidental focal FDG
uptake in the colon mentioned in the PET/CT scan report were included. Incidental focal colonic FDG uptake was
defined as focal accumulation of activity greater than the
surrounding background in the colon that could not be
explained based on the patient’s known medical history at
the time of scanning. Thus, those foci of increased uptake
referring to known colorectal cancers were excluded
from the study. The location and intensity in terms of
maximum standardised uptake values (SUVmax) of
these foci were retrieved from the medical report. The
medical records of these patients were then reviewed
by a single researcher for demographic information,
medical history, and subsequent investigations of the
incidental colonic uptake, if any.
Positron Emission Tomography/Computed
Tomography Protocol
Imaging was performed with a PET/CT scan system
with a spatial resolution of 6.6 mm in the centre of the
field of view (Discovery LS, GE Healthcare, Milwaukee
[WI], United States). All patients fasted for at least
6 hours before the PET/CT study. 370 MBq of FDG
was injected intravenously. Imaging was initiated
60±5 minutes after intravenous FDG injection.
Intravenous iodinated contrast medium was used if it
was requested by the ordering physicians. Images were
acquired from the skull vertex to mid-thigh. Image acquisition was performed for 3 minutes per bed position.
Low-dose CT was performed for attenuation correction
and lesion localisation. The examinations were then
reported by one of four independent nuclear medicine
physicians, each of whom has at least 8 years of PET/CT
interpretation experience.
Endoscopic or Surgical Correlation
Findings of subsequent colonoscopy were retrieved from
the electronic medical record database for all patients
with incidental focal colonic FDG uptake. Colonoscopy
was considered diagnostic if it was performed within
120 days of the PET/CT study. For those patients with
colonoscopy performed >120 days after the PET/CT
study, the focal colonic FDG activity was not further
evaluated and excluded from the study. Findings on
endoscopy were correlated with the incidental focal
colonic FDG activity on the PET/CT report. Whenever
a biopsy or polypectomy of the positively correlated
endoscopic abnormalities was performed, the subsequent
pathological reports were evaluated. If the endoscopic
findings were negative, the incidental focal colonic FDG
activity was considered as normal/physiologic. The final
diagnoses were classified into one of four categories:
malignant, premalignant (such as tubular adenoma,
villous adenoma, and tubulovillous adenoma), benign
(hyperplastic polyps or inflammatory lesions), and
normal.
Statistical Analysis
Statistical analysis was performed using SPSS (Windows
version 22.0; IBM Corp, Armonk [NY], United States).
Descriptive statistics were used to delineate the incidence
of incidental focal colonic FDG activity. The nonparametric
Mann-Whitney U test was used to assess for
differences of the SUVmax between groups (malignant
vs benign; malignant + premalignant vs benign; and
malignant vs premalignant). Statistical significance was
assumed for p<0.05. Receiver operating characteristic
curve (ROC) analysis was performed to determine an
optimal cut-off value for SUVmax for differentiating
benign from premalignant lesions.
RESULTS
Among the 1851 patients, 93 incidental foci of colonic
FDG uptake were reported in 88 patients, giving an
incidence of 4.8%. The majority of these patients were
men (62 male vs 26 female) with mean age 69 years.
Most foci of incidental uptake were located in the
sigmoid colon (30 foci, 32%). In total, 22, 19, and 17
foci of increased uptake involved the rectum, ascending colon, and descending colon, respectively. The fewest
incidental uptake foci involved the transverse colon,
accounting for 5%. Figure 1 shows the flowchart for
patient selection.
Figure 1. Flowchart for patient selection
Of 45 patients undergoing subsequent endoscopies and
five patients undergoing surgery ≤120 days after the
PET/CT study, the histological specimens of one of the
patients were considered necrotic by the pathologists and
the nature of the lesion could not be determined. Another
patient, with two foci of FDG uptake on the PET/CT
study, underwent endoscopy at another location,
and detailed pathological reports were not available.
Thus, these two patients were excluded from further
histopathologic analysis.
After these exclusions, 48 patients remained: 33 of
them (35 foci of increased uptake) had true-positive
colonoscopies; five patients (six foci of uptake)
underwent surgery directly; and the remaining 10 patients
had normal colonoscopy. Of the 38 patients with
positive findings, nine patients (10 foci of uptake) had
adenocarcinoma, 21 patients (23 foci of uptake) had premalignant lesions, and the remaining eight patients
(8 foci of uptake) had benign pathology on histological
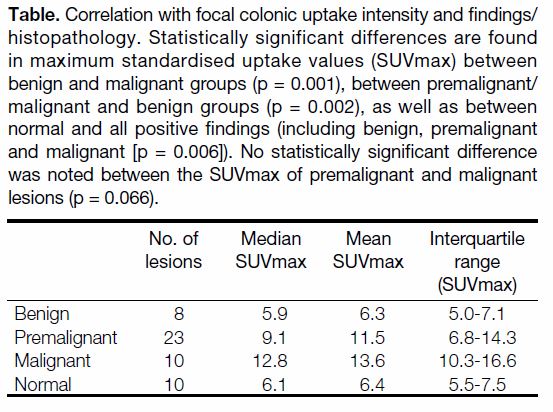
findings. The mean, median and interquartile range of
these uptakes are given in the Table. Figure 2 shows one
of the patients with positive colonoscopy findings. A
statistically significant difference of SUVmax was found
between the benign and malignant groups (p = 0.001) as
well as between the benign and premalignant/malignant groups (p = 0.002). There was no statistically significant
difference in SUVmax between the premalignant
and malignant groups when analysed with the Mann-
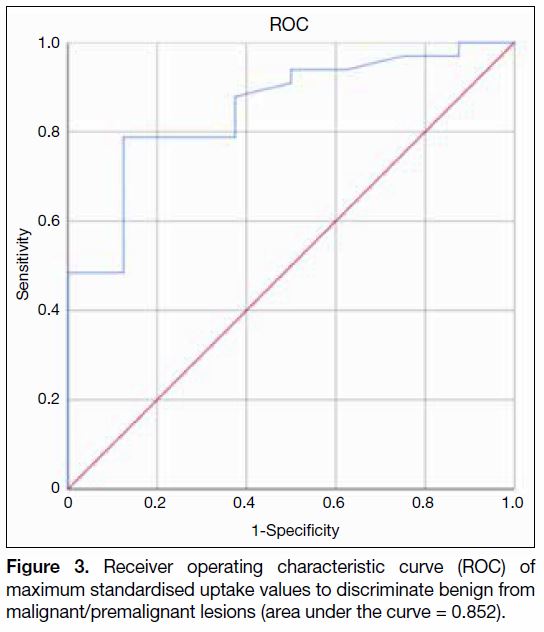
Whitney U test (p = 0.066). According to ROC analysis,
the optimal diagnostic cut-off value to discriminate
between benign and premalignant/malignant lesions was
an SUVmax of 7.5 (sensitivity 78.8%; specificity 87.5%;
area under curve 0.852). Figure 3 shows the ROC.
Table. Correlation with focal colonic uptake intensity and findings/histopathology. Statistically significant differences are found
in maximum standardised uptake values (SUVmax) between
benign and malignant groups (p = 0.001), between premalignant/malignant and benign groups (p = 0.002), as well as between
normal and all positive findings (including benign, premalignant
and malignant [p = 0.006]). No statistically significant difference
was noted between the SUVmax of premalignant and malignant
lesions (p = 0.066).
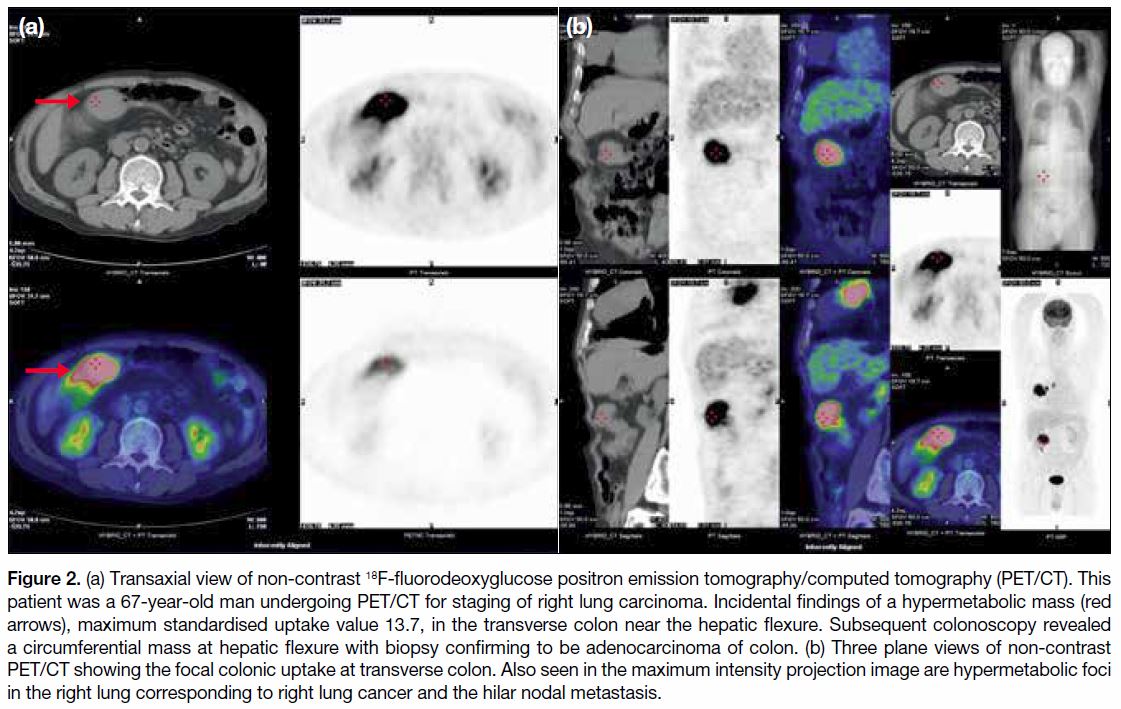
Figure 2. (a) Transaxial view of non-contrast 18F-fluorodeoxyglucose positron emission tomography/computed tomography (PET/CT). This
patient was a 67-year-old man undergoing PET/CT for staging of right lung carcinoma. Incidental findings of a hypermetabolic mass (red
arrows), maximum standardised uptake value 13.7, in the transverse colon near the hepatic flexure. Subsequent colonoscopy revealed
a circumferential mass at hepatic flexure with biopsy confirming to be adenocarcinoma of colon. (b) Three plane views of non-contrast
PET/CT showing the focal colonic uptake at transverse colon. Also seen in the maximum intensity projection image are hypermetabolic foci
in the right lung corresponding to right lung cancer and the hilar nodal metastasis.
Figure 3. Receiver operating characteristic curve (ROC) of
maximum standardised uptake values to discriminate benign from
malignant/premalignant lesions (area under the curve = 0.852).
DISCUSSION
Because of the increased application of PET/CT for
oncological management, incidental FDG activity in the
gastrointestinal tract is encountered more frequently. In
the present study, incidental focal colonic FDG uptake
was found in 4.8% of our patients. The incidence of
incidental focal colonic FDG activity varies among
studies, ranging from 1.1% to 28%.[7] [8] [9] This wide range of
incidence may be related to the variation in the definition
of focal FDG uptake.
Unfortunately, nearly half of the uptake foci (44%) did
not have subsequent correlative surgery or endoscopy
in our study. One of the reasons for not undergoing
subsequent correlative investigation for these patients was related to the advanced stage or metastatic nature
of their diseases (34%). As a result, we have no idea of
the nature of the lesions these foci represent. Among the
48 patients (with 51 foci of increased uptake) having
subsequent correlative investigations, 38 of them (with
41 uptake foci) had a positive endoscopy or surgery,
giving positive predictive value (PPV) of 80.4%. Our
findings are similar to previous studies concerning focal
colonic FDG uptake. Gutman et al reported that 15 of
20 patients with focal colonic FDG uptake had positive
endoscopic findings.[10] van Hoeij et al,[11] Treglia et al,[7]
Garrido Durán et al[12] and Putora et al[13] reported a PPV of
62% to 86%. In view of the high likelihood of identifying a
polypoid lesion, our study supports previous suggestions
of performing endoscopy for further investigations of
incidental focal colonic activity.[14]
In our study, the SUVmax for malignant and premalignant
lesions were significantly higher than those for benign
lesions, but not significantly different between malignant
and premalignant lesions. In the retrospective study done
by Luboldt et al,[15] high-grade adenomas and malignancies
demonstrated significantly higher SUVmax. Similar
findings were also reported in a retrospective study done
by van Hoeij et al.[11] However, some other previous studies
had been unable to demonstrate these differences among
the different groups assessed.[16] In our study according to ROC analysis, an optimal cut-off value to discriminate
premalignant/malignant from benign lesions is SUVmax
≥7.5. With colorectal cancer known to be arising
from adenomatous polyps, it is a common practice to
remove these polyps to prevent future development of
malignancy.[17] Thus we believe including precancerous
lesions to be of utmost importance in cancer prevention.
Our study has some limitations. First of all, up to 40% of
the patients with incidental focal colonic FDG activity did
not undergo further endoscopic correlation. As a result,
we were unable to know the nature of these uptakes.
Secondly, our data are limited to a single, tertiary referral
centre. Lastly, our study was a retrospective review of
PET/CT reports that have been reported by several
nuclear medicine physicians; hence inter-observer
variations in reporting were expected.
CONCLUSION
The incidence of incidental foci of colonic FDG uptake
identified in our institution was 4.8%. These incidental
foci had a high PPV for polypoid growths. Thus, all
incidental focal hotspots in the colon should be further
investigated. Malignant and premalignant lesions have
significantly higher SUVmax than benign lesions. The
SUVmax may be helpful in distinguishing premalignant/malignant from benign lesions, with an optimal cut-off
of ≥7.5. Thus, SUVmax may have a role in assisting
prioritisation of incidental foci of increased uptake for
endoscopic investigation.
REFERENCES
1. Chen K, Chen X. Positron emission tomography imaging of
cancer biology: current status and future prospects. Semin Oncol.
2011;38:70-86. Crossref
2. Beatty JS, Williams HT, Aldridge BA, Hughes MP, Vasudeva VS,
Gucwa AL, et al. Incidental PET/CT findings in the cancer patient:
how should they be managed? Surgery. 2009;146:274-81. Crossref
3. Liu Y, Ghesani NV, Zuckier LS. Physiology and pathophysiology
of incidental findings detected on FDG-PET scintigraphy. Semin
Nucl Med. 2010;40:294-315. Crossref
4. Cook GJ, Fogelman I, Maisey MN. Normal physiological and
benign pathological variants of 18-fluoro-2-deoxyglucose positron
emission tomography scanning: potential for error in interpretation.
Semin Nucl Med. 1996;26:308-14. Crossref
5. Şimşek FS, İspiroğlu M, Taşdemir B, Köroğlu R, Ünal K,
Özercan IH, et al. What approach should we take for the incidental
finding of increased 18F-FDG uptake foci in the colon on PET/
CT? Nucl Med Commun. 2015;36:1195-201. Crossref
6. Salazar Andía G, Prieto Soriano A, Ortega Candil A,
Cabrera Martín MN, González Roiz C, Ortiz Zapata JJ, et al.
Clinical relevance of incidental finding of focal uptakes in the
colon during 18F-FDG PET/CT studies in oncology patients
without known colorectal carcinoma and evaluation of the impact
on management. Rev Esp Med Nucl E Imagen Mol. 2012;31:15-21. Crossref
7. Treglia G, Calcagni ML, Rufini V, Leccisotti L, Meduri GM, Spitilli MG, et al. Clinical significance of incidental focal colorectal
(18)F-fluorodeoxyglucose uptake: our experience and a review of
the literature. Colorectal Dis. 2012;14:174-80. Crossref
8. Peng J, He Y, Xu J, Sheng J, Cai S, Zhang Z. Detection of incidental
colorectal tumours with 18F-labelled 2-fluoro-2-deoxyglucose
positron emission tomography/computed tomography scans: results
of a prospective study. Colorectal Dis. 2011;13:e374-8. Crossref
9. Kunawudhi A, Wong AK, Alkasab TK, Mahmood U. Accuracy
of FDG PET/CT for detection of incidental premalignant and
malignant colonic lesions—correlation with colonoscopic and
histopathologic findings. Asian Pac J Cancer Prev. 2016;17:4143-7.
10. Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F,
et al. Incidental colonic focal lesions detected by FDG PET/CT.
AJR Am J Roentgenol. 2005;185:495-500. Crossref
11. van Hoeij FB, Keijsers RG, Loffeld BC, Dun G, Stadhouders PH,
Weusten BL. Incidental colonic focal FDG uptake on PET/CT:
can the maximum standardized uptake value (SUVmax) guide
us in the timing of colonoscopy? Eur J Nucl Med Mol Imaging.
2015;42:66-71. Crossref
12. Garrido Durán C, Payeras Capó MA, García Caparrós C,
Giménez García M, Daumal Domenech J. Clinical-endoscopic relevance of incidental colorectal lesions detected by PET-CT.
Rev Esp Enferm Dig. 2018;110:434-9. Crossref
13. Putora PM, Müller J, Borovicka J, Plasswilm L, Schmidt F.
Relevance of incidental colorectal FDG-PET/CT-enhanced lesions.
Onkologie. 2013;36:200-4. Crossref
14. Farquaharson AL, Chopra A, Ford A, Matthews S, Amin
SN, De Noronha R. Incidental focal colonic lesions found on
(18)Fluorodeoxyglucose positron emission tomography/computed
tomography scan: further support for a national guideline on
definitive management. Colorectal Dis. 2012;14:e56-63. Crossref
15. Luboldt W, Volker T, Wiedemann B, Zöphel K, Wehrmann
U, Koch A, et al. Detection of relevant colonic neoplasms with
PET/CT: promising accuracy with minimal CT dose and a
standardized PET cut-off. Eur Radiol. 2010;20:2274-85. Crossref
16. Kei PL, Vikram R, Yeung HW, Stroehlein JR, Macapinlac HA.
Incidental finding of focal FDG uptake in the bowel during
PET/CT: CT features and correlation with histopathologic results.
AJR Am J Roentgenol. 2010;194:W401-6. Crossref
17. O’ Brien MJ. Colorectal polyp. In: Cohen AM, Winawer SJ, editors.
Cancer of the Colon, Rectum and Anus. New York, NY: McGraw-Hill; 1995. p 127-35.
| Attachment | Size |
|---|---|
| v23n4_Incidental.pdf | 521.69 KB |