Piriformis Syndrome is a Rare Cause of Insidious Unilateral Lower Limb Weakness and Buttock Pain: a Case Report
CASE REPORT
Piriformis Syndrome is a Rare Cause of Insidious Unilateral Lower Limb Weakness and Buttock Pain: a Case Report
AWT Chin, KS Tse, PY Chu
Department of Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong
Correspondence: Dr AWT Chin, Department of Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong. Email: anthonywtchin@gmail.com
Submitted: 22 Mar 2019; Accepted: 24 Apr 2019.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: The patient was treated in accordance with the tenets of the Declaration of Helsinki. The patient provided written informed
consent for all treatments and procedures.
INTRODUCTION
Piriformis syndrome is a neuromuscular disorder in
which the sciatic nerve is compressed at the level of
the piriformis muscle. Patients usually complain of
buttock pain radiating down the thigh.[1] Primary causes
are intrinsic abnormalities such as aberrant piriformis
muscle fibres; secondary causes involve direct injury
of the piriformis muscle resulting in hematoma or scar
tissue formation.[1] Piriformis syndrome constitutes 0.3%
to 6% of all cases of low back or buttock pain.[1] [2] There
are no uniform standardised diagnostic criteria because
symptoms can be non-specific and electrodiagnostic
tests are technically difficult to perform.[3] Magnetic
resonance imaging (MRI) helps to depict the anatomical
relationship of the sciatic nerve with the piriformis
muscle and can exclude secondary compression of the
sciatic nerve. We report a case of piriformis syndrome in
a young adult patient successfully diagnosed with the aid
of MRI and treated with surgery.
CASE REPORT
A 34-year-old man presented with right buttock pain,
right lower limb clumsiness and weakness of gradual
increasing severity for 3 years. His medical history
was unremarkable except for allergic rhinitis and
appendectomy. The patient denied any trauma history. Physical examination revealed tenderness and shooting
pain along the right posterior thigh radiating to the right calf on pressing the right gluteal region. Seated
piriformis stretch test (a passive flexion, adduction with
internal rotation test performed as the examiner palpates
the deep gluteal region with the patient seated) and pace
test (abduction and external rotation against resistance)
reproduced the symptoms, but straight leg raise test did
not. The patient had impaired dorsiflexion of the big
toe with power of grade 4 out of 5. Motor and sensory
examinations were otherwise unremarkable.
The preliminary working diagnosis was piriformis
syndrome. Nerve conduction study failed to detect any
abnormality. MRI of the lumbosacral spine did not reveal
evidence of neurological compression. MRI of the pelvis
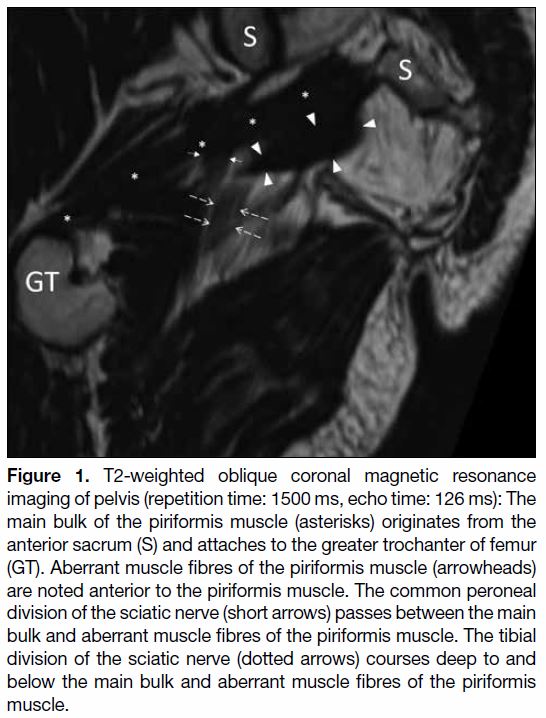
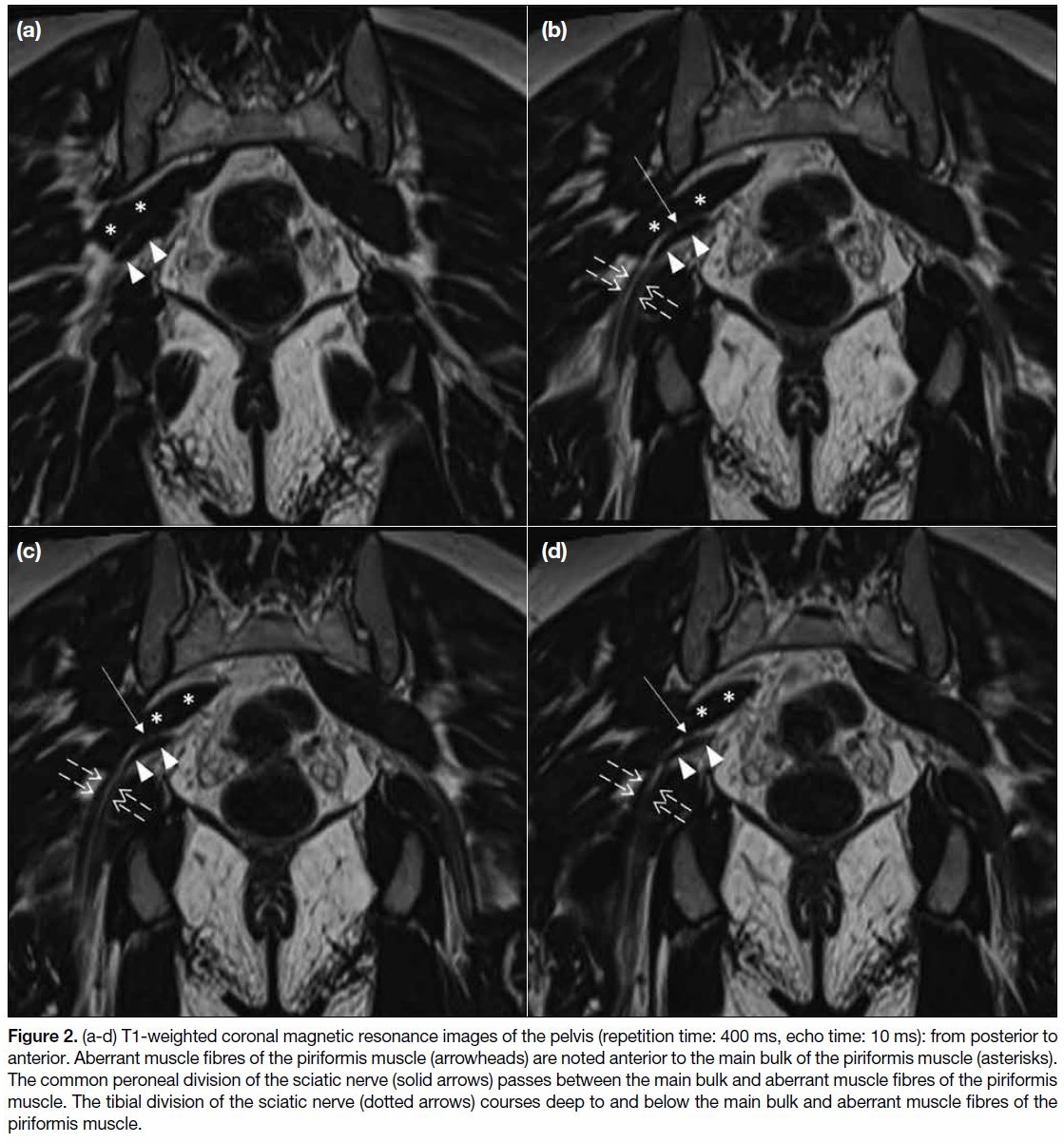
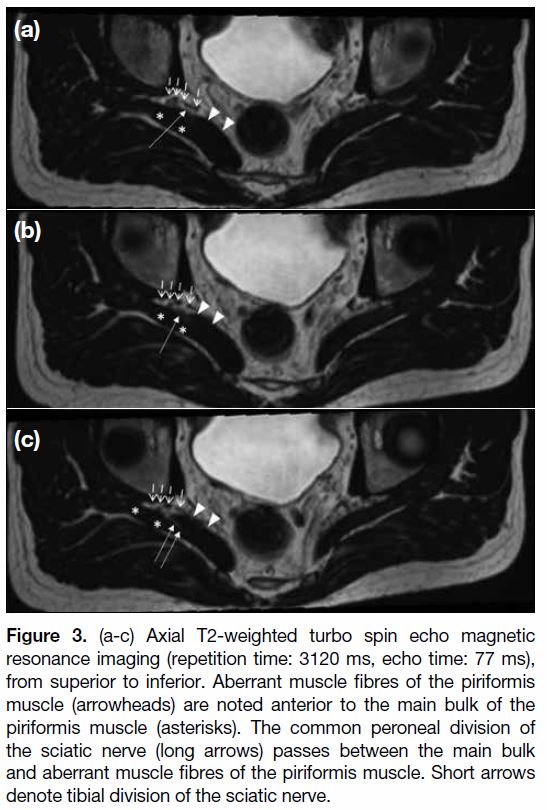
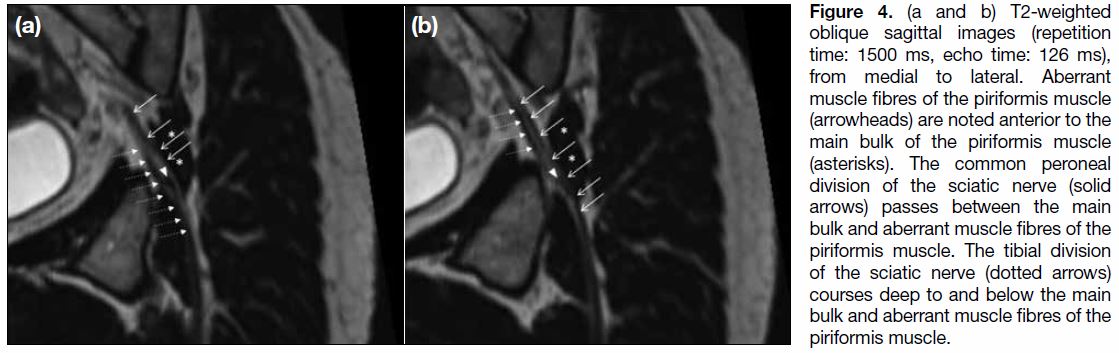
(Figures 1 2 3 4) revealed the presence of aberrant fibres
of the right piriformis muscle anterior to its main bulk.
The common peroneal branch of the right sciatic nerve
appeared to branch out proximally and travel between
the aberrant and main muscle bulk of the piriformis muscle (Beaton and Anson’s classification type B). The
left sciatic nerve course was below the piriformis muscle
with no aberrant muscle fibres detected (Beaton and
Anson’s classification type A).
Figure 1. T2-weighted oblique coronal magnetic resonance
imaging of pelvis (repetition time: 1500 ms, echo time: 126 ms): The
main bulk of the piriformis muscle (asterisks) originates from the
anterior sacrum (S) and attaches to the greater trochanter of femur
(GT). Aberrant muscle fibres of the piriformis muscle (arrowheads)
are noted anterior to the piriformis muscle. The common peroneal
division of the sciatic nerve (short arrows) passes between the main
bulk and aberrant muscle fibres of the piriformis muscle. The tibial
division of the sciatic nerve (dotted arrows) courses deep to and
below the main bulk and aberrant muscle fibres of the piriformis
muscle.
Figure 2. (a-d) T1-weighted coronal magnetic resonance images of the pelvis (repetition time: 400 ms, echo time: 10 ms): from posterior to
anterior. Aberrant muscle fibres of the piriformis muscle (arrowheads) are noted anterior to the main bulk of the piriformis muscle (asterisks).
The common peroneal division of the sciatic nerve (solid arrows) passes between the main bulk and aberrant muscle fibres of the piriformis
muscle. The tibial division of the sciatic nerve (dotted arrows) courses deep to and below the main bulk and aberrant muscle fibres of the
piriformis muscle.
Figure 3. (a-c) Axial T2-weighted turbo spin echo magnetic
resonance imaging (repetition time: 3120 ms, echo time: 77 ms),
from superior to inferior. Aberrant muscle fibres of the piriformis
muscle (arrowheads) are noted anterior to the main bulk of the
piriformis muscle (asterisks). The common peroneal division of
the sciatic nerve (long arrows) passes between the main bulk
and aberrant muscle fibres of the piriformis muscle. Short arrows
denote tibial division of the sciatic nerve.
Figure 4. (a and b) T2-weighted
oblique sagittal images (repetition
time: 1500 ms, echo time: 126 ms),
from medial to lateral. Aberrant
muscle fibres of the piriformis muscle
(arrowheads) are noted anterior to the
main bulk of the piriformis muscle
(asterisks). The common peroneal
division of the sciatic nerve (solid
arrows) passes between the main
bulk and aberrant muscle fibres of the
piriformis muscle. The tibial division
of the sciatic nerve (dotted arrows)
courses deep to and below the main
bulk and aberrant muscle fibres of the
piriformis muscle.
The patient underwent surgery under general anaesthesia
and MRI findings were confirmed. The common
peroneal branch of the sciatic nerve was identified to
penetrate between the main bulk and the aberrant muscle fibres of the piriformis with an indentation noted at the
penetration site. The tendon insertion of the main bulk
of the piriformis muscle was released from the greater
trochanter. The aberrant piriformis muscle was released
and excised.
The patient recovered dorsiflexion of his right big toe
with full motor power. Neurological examination and
sensation of the right lower limb was normal without any
complications. The patient had subjective improvement
of symptoms.
DISCUSSION
The piriformis muscle originates at the anterolateral
S2-S4 level of the sacrum, travels through the greater
sciatic foramen and attaches to the greater trochanter.[1] [3]
It acts as an external rotator of the hip as well as assisting
hip flexion and hip abduction. Beaton and Anson first
described variations in the sciatic nerve relationship
with the piriformis muscle.[4] The undivided sciatic nerve
passes completely below the piriformis muscle in most
people (Beaton and Anson classification type A). A
recent study of 102 limbs showed that 89% of subjects
had conventional anatomy, while in 8.8% of subjects,
the common peroneal branch of the sciatic nerve passed
through the piriformis muscle, as in our patient (Beaton
and Anson classification type B).[5] In the remaining 2.9%,
the common peroneal branch passed over the piriformis
muscle (Beaton and Anson classification type C).[5] All
but one subject showed variant anatomy in one lower
limb but normal in the other.[5] Multiple manoeuvres have
been described that elicit sciatic pain due to piriformis
stretching and contraction through hip movements.[6] [7]
Anatomical variations are thought to be related to
development of piriformis syndrome, especially that of
Beaton and Anson classification type B.[5] Knowledge of
the anatomical course of the sciatic nerve is important to guide choice of physiotherapy exercises, image-guided
analgesic injections and surgical approach.[5]
With the advancement of MRI, acquisitions of images
of the pelvis in the axial and coronal planes as well as
multiplanar reconstruction using isometric sequences
enables a clear anatomical depiction of the sciatic nerve
and pyriformis and facilitates subsequent management.
Use of MRI in diagnosing piriformis syndrome has
been previously confined to case reports with anatomy
confirmed during surgery.[1] [8] [9] [10] Our institution performs
T1-weighted and T2-weighted spin echo sequences in
axial and coronal planes with and without fat suppressed
techniques, as well as T2-weighted isometric images
acquired in the coronal plane. We find the images
without fat suppression techniques allow better depiction
of sciatic nerve and piriformis anatomy, while use of
fat suppression techniques achieves better depiction
of muscle oedema. Features to look for include sciatic
nerve configuration, any thickening and signal change
of the piriformis muscle and exclusion of other causes
of sciatic nerve compression such as haematoma or soft
tissue mass.[1] [3] Sciatic nerve signal changes may not
be present as in our case. This is due to the functional
nature of the syndrome, as the sciatic nerve may not be
compressed when the patient lies supine on the MRI
examination table.[9] In addition, limitation of physical
activity by the patient as well as chronicity of disease
may explain the lack of sciatic nerve signal changes.[9]
No single imaging feature is diagnostic of the condition.
Piriformis asymmetry may not be diagnostic of
piriformis syndrome, as shown in a study of 100 patients
with no symptoms of piriformis syndrome but in whom
16% had piriformis asymmetry of 4 mm or more.[11]
Clinical correlation is crucial to making the correct
diagnosis. There is more recent evidence that use of MRI
neurography allows even better delineation of anatomy
and signal changes of the sciatic nerve.[12] [13] [14]
It has been argued that there is no gold standard to reliably
diagnose piriformis syndrome. Previous studies based on
treatment response assessed the usefulness of clinical and
imaging features to diagnose the condition. However,
Filler[14] suggested that the marked improvement in
symptoms followed by an MRI diagnosis and imageguided
injections strongly supports the importance of
piriformis in causing a patient’s symptoms.[1]
Treatment of piriformis syndrome is usually non-surgical
and includes oral analgesics and image-guided analgesic injections. Surgery is reserved for cases not amenable to
conservative management.[1]
CONCLUSION
We have described a young adult patient with piriformis
syndrome that was successfully diagnosed with the
assistance of MRI and who subsequently underwent
surgery with improved clinical symptoms. This
highlights the importance of multiplanar imaging to
assist in the diagnosis of this clinical entity.
REFERENCES
1. Miller TA, White KP, Ross DC. The diagnosis and management
of Piriformis Syndrome: myths and facts. Can J Neurol Sci.
2012;39:577-83. Crossref
2. Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated
2018 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2019 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/. Accessed 2 Jan 2019.
3. Petchprapa CN, Rosenberg ZS, Sconfienza LM, Cavalcanti CF,
Vieira RL, Zember JS. MR imaging of entrapment neuropathies
of the lower extremity. Part 1. The pelvis and hip. Radiographics.
2010;30:983-1000. Crossref
4. Beaton LE, Anson BJ. The relation of the sciatic nerve and of its
subdivision to the piriformis muscle. Anat Rec. 1937;70:1-5. Crossref
5. Lewis S, Jurak J, Lee C, Lewis R, Gest T. Anatomical variations of
the sciatic nerve, in relation to the piriformis muscle. Translational
Res Anat. 2016;5:15-9. Crossref
6. Michel F, Decavel P, Toussirot E, Tatu L, Aleton E, Monnier G,
et al. Piriformis muscle syndrome: diagnostic criteria and treatment
of a monocentric series of 250 patients. Ann Phys. Rehabil Med.
2013;56:371-83. Crossref
7. Michel F, Decavel P, Toussirot E, Tatu L, Aleton E, Monnier G,
et al. The piriformis muscle syndrome: an exploration of anatomical
context, pathophysiological hypotheses and diagnostic criteria. Ann
Phys Rehabil Med. 2013;56:300-11. Crossref
8. Jankiewicz JJ, Hennrikus WL, Houkom JA. The appearance of the
piriformis muscle syndrome in computed tomography and magnetic
resonance imaging. A case report and review of the literature. Clin
Orthop Relat Res. 1991;(262):205-9. Crossref
9. Lee EY, Margherita AJ, Gierada DS, Narra VR. MRI of piriformis
syndrome. AJR Am J Roentgenol. 2004;183:63-4. Crossref
10. Rossi P, Cardinali P, Serrao M, Parisi L, Bianco F, De Bac S.
Magnetic resonance imaging findings in piriformis syndrome: a
case report. Arch Phys Med Rehabil. 2001;82:519-21. Crossref
11. Russell JM, Kransdorf MJ, Bancroft LW, Peterson JJ, Berquist TH,
Bridges MD. Magnetic resonance imaging of the sacral plexus and
piriformis muscles. Skeletal Radiol. 2008;37:709-13. Crossref
12. Filler AG, Haynes J, Jordan SE, Prager J, Villablanca JP,
Farahani K, et al. Sciatica of nondisc origin and piriformis
syndrome: diagnosis by magnetic resonance neurography and
interventional magnetic resonance imaging with outcome study of
resulting treatment. J Neurosurg Spine. 2005;2:99-115. Crossref
13. Filler AG, Kliot M, Howe FA, Hayes CE, Saunders DE,
Goodkin R, et al. Application of magnetic resonance neurography
in the evaluation of patients with peripheral nerve pathology. J
Neurosurg. 1996;85:299-309. Crossref
14. Filler AG. Piriformis and related entrapment syndromes: diagnosis
& management. Neurosurg Clin N Am. 2008;19:609-22, vii. Crossref
| Attachment | Size |
|---|---|
| v23n4_Piriformis.pdf | 286.7 KB |