Benign Soft Tissue and Osseous Tumours of the Hand: a Pictorial Essay
PICTORIAL ESSAY
Benign Soft Tissue and Osseous Tumours of the Hand:
a Pictorial Essay
WI Sit, SKS Tse, PY Chu, KKL Lo
Department of Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong
Correspondence: Dr WI Sit, Department of Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong.. Email: sitsitkathy@gmail.com
Submitted: 12 Oct 2018; Accepted: 27 Dec 2018.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This pictorial essay received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: This study was approved by the Kowloon Central/Kowloon East Cluster Research Ethics Committee (Ref KC/KE-20-0023/
ER-3). The patients provided written informed consent for all treatments and procedures.
INTRODUCTION
Both soft tissue and osseous lesions of the hand are
commonly encountered in everyday clinical practice.
The majority of these lesions are benign, and imaging is
often needed to determine the nature of the lesion. Some
lesions demonstrate characteristic features that enable
diagnosis without intervention. For soft tissue lesions,
plain radiographs have a limited role in diagnosis but
are useful to demonstrate calcification or mineralisation.
Ultrasonography and magnetic resonance imaging (MRI)
play an important role in characterisation of soft tissue
masses of the hand. Ultrasonography can differentiate
cystic from non-cystic masses and MRI can further
characterise the latter. Benign primary bone tumours of
the hand are often found incidentally during presentation
of unrelated injuries or pain due to pathological fracture.
Radiography is usually the first imaging of choice with
computed tomography or MRI reserved for complex
cases. It is important to be familiar with the variety of
lesions that can occur in the hand so that appropriate
clinical management can be instigated and unnecessary
interventions avoided. In this article, we review the
imaging findings of common benign hand lesions with
attention to their discriminating features.
BENIGN SOFT TISSUE TUMOURS
Ganglion Cyst
Ganglion cysts are the most commonly encountered
soft tissue mass in the hand and wrist region.[1] They tend
to occur in adults, with a female predominance. The
prevalence of ganglion cysts in the hand and wrist region
has been reported in up to 51% of the asymptomatic adult
population.[1] The most common location is in the dorsum
of the wrist, typically close to the scapholunate joint.
Other less common sites include the volar aspect of the
wrist and flexor tendon sheath of the fingers. Ganglion
cysts are thought to represent degeneration of connective
tissue caused by chronic irritation.[2] A tendon sheath cyst
consists of a special ganglion cyst subtype located along
the course of a tendon sheath. Tendon sheath cysts should
be distinguished from the rarer intratendinous cysts that
are believed to result from recurrent injury to the tendon
with subsequent cystic degeneration. Intratendinous
ganglia are clinically relevant because they weaken
the structure of tendons and may predispose them to
rupture.[3] Diagnosis is usually made by ultrasonography
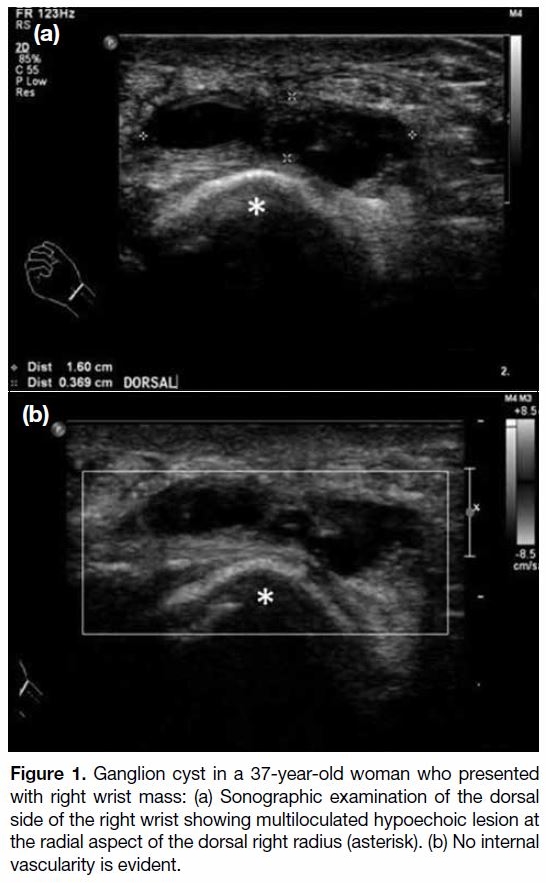
(Figure 1). On ultrasonography scans, ganglion cysts
appear as unilocular or multilocular anechoic to
hypoechoic lesions with posterior acoustic enhancement.
Figure 1. Ganglion cyst in a 37-year-old woman who presented
with right wrist mass: (a) Sonographic examination of the dorsal
side of the right wrist showing multiloculated hypoechoic lesion at
the radial aspect of the dorsal right radius (asterisk). (b) No internal
vascularity is evident.
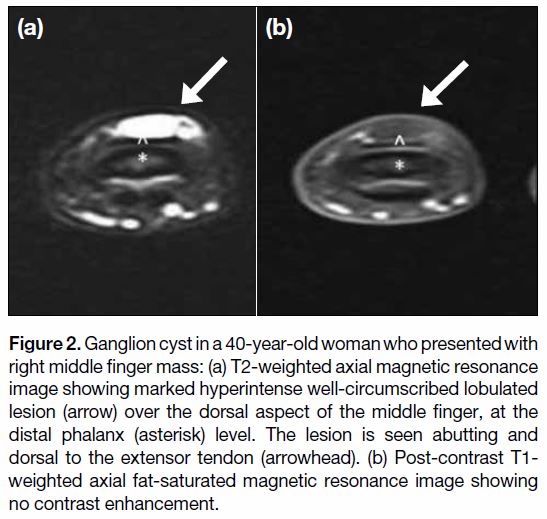
Occasionally, the neck of the lesion may demonstrate
extension towards the adjacent joint. On MRI scans
(Figure 2), ganglion cysts are seen as well circumscribed
unilocular or multilocular cystic lesions without
corresponding contrast enhancement. Sometimes, they
may demonstrate an isointense or hyperintense T1 signal
due to proteinaceous content or haemorrhage.
Figure 2. Ganglion cyst in a 40-year-old woman who presented with
right middle finger mass: (a) T2-weighted axial magnetic resonance
image showing marked hyperintense well-circumscribed lobulated
lesion (arrow) over the dorsal aspect of the middle finger, at the
distal phalanx (asterisk) level. The lesion is seen abutting and
dorsal to the extensor tendon (arrowhead). (b) Post-contrast T1-weighted axial fat-saturated magnetic resonance image showing
no contrast enhancement.
Epidermoid Inclusion Cyst
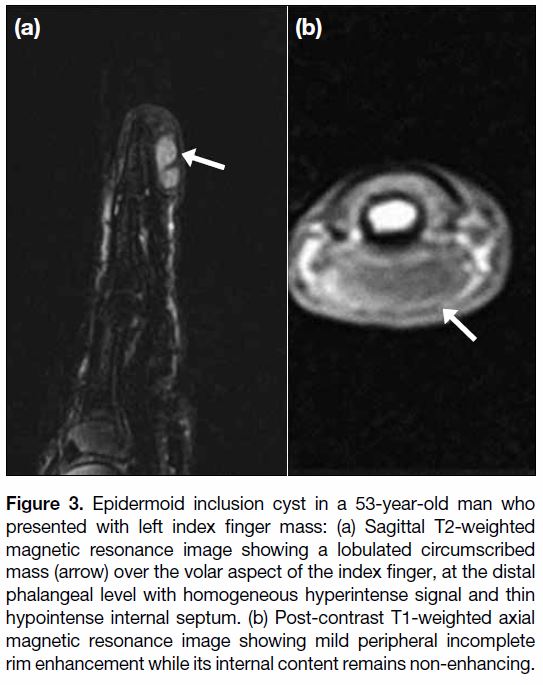
Epidermoid cyst formation (Figure 3) results from
proliferation of surface epidermal cells within the
confined space of the dermis. It is a common benign
cystic lesion that can occur anywhere in the body with
about 10% found in the upper limbs. It is commonly
seen secondary to trauma with implantation of epithelial
squames into the dermis. In the hands, it is usually
seen within subcutaneous tissue at the finger pulps. It
can also cause adjacent bony erosion that is evident on
radiograph or computed tomography. On MRI scan, it is seen as a well-circumscribed lesion with variable
signal intensity on T2-weighted sequence depending
on the chemical composition. Lesions with a high
lipid content will demonstrate hyperintense signal on
both T1- and T2-weighted images, whereas lesions
with keratin and microcalcifications will demonstrate low signal intensity on T2-weighted images. After
administration of gadolinium contrast, there is a lack
of enhancement in uncomplicated cases. Peripheral rim
enhancement is possible with underlying inflammatory
or infective changes.[4] In cases of ruptured epidermal
cyst, MRI scan may show thick and irregular peripheral
rim enhancement, surrounding soft tissue reactions,
and/or variable septa, therefore simulating an infectious
or neoplastic lesion. It might resemble some malignant
soft tissue tumours with central necrosis and these should
be included in the differential diagnosis list.[5]
Figure 3. Epidermoid inclusion cyst in a 53-year-old man who
presented with left index finger mass: (a) Sagittal T2-weighted
magnetic resonance image showing a lobulated circumscribed
mass (arrow) over the volar aspect of the index finger, at the distal
phalangeal level with homogeneous hyperintense signal and thin
hypointense internal septum. (b) Post-contrast T1-weighted axial
magnetic resonance image showing mild peripheral incomplete
rim enhancement while its internal content remains non-enhancing.
Giant Cell Tumours of the Tendon Sheath
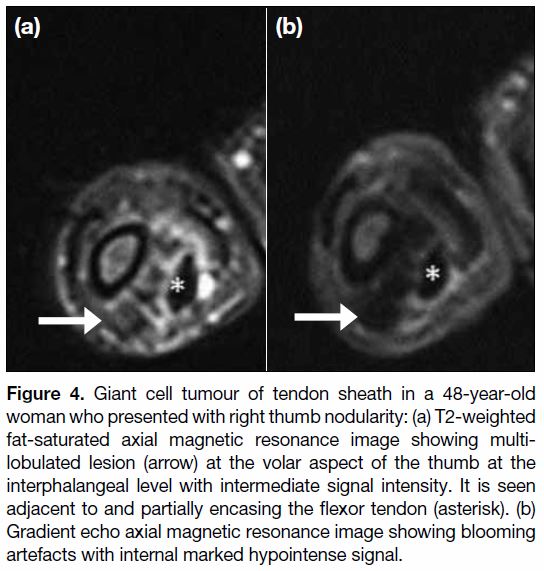
Tenosynovial giant cell tumours are a group of generally
benign soft tissue tumours with common histological
findings. Previously termed villonodular tenosynovitis,
the tumours are commonly found in the hand region.[6]
The tumours are lobulated, well circumscribed and
at least partially covered by a fibrous capsule. Their
microscopic appearance is variable, depending on the
proportion of mononuclear cells, multinucleated giant
cells, foamy macrophages, and siderophages and the
amount of stroma. Haemosiderin deposits are virtually
always identified.[7] Tenosynovial giant cell tumours can
be roughly divided into two distinct forms: localised
and diffuse. The localised form primarily occurs extra-articularly
in the tendon sheaths of the hand and foot, or
sometimes in bursa; whereas the diffuse form occurs in
larger joints with a more aggressive growth pattern and
associated with a higher recurrence rate. The aetiology of
giant cell tumour of the tendon sheath remains uncertain.
They usually present as a painless mass in the hands
or feet with non-specific clinical features and are seen
close to a joint or tendons on imaging. Pressure erosion
in adjacent bone can be seen on plain radiographs in
10% to 20% of cases.[8] MRI is currently the optimal
modality for preoperative assessment of tumour size,
extent and invasion of adjacent joint and tenosynovial
space.[9] On MRI scans (Figure 4), the tumour has a low
signal intensity on T1-weighted imaging and variable,
but usually low to intermediate, signal intensity on
T2-weighted imaging. There is moderate contrast
enhancement after intravenous gadolinium contrast
medium injection. Susceptibility artefact on gradient
echo sequence is typical due to haemosiderin deposition.
This is rarely seen in other masses and serves as a useful
feature to differentiate from other soft tissue lesions in
the hand.
Figure 4. Giant cell tumour of tendon sheath in a 48-year-old
woman who presented with right thumb nodularity: (a) T2-weighted
fat-saturated axial magnetic resonance image showing multi-lobulated
lesion (arrow) at the volar aspect of the thumb at the
interphalangeal level with intermediate signal intensity. It is seen
adjacent to and partially encasing the flexor tendon (asterisk). (b)
Gradient echo axial magnetic resonance image showing blooming
artefacts with internal marked hypointense signal.
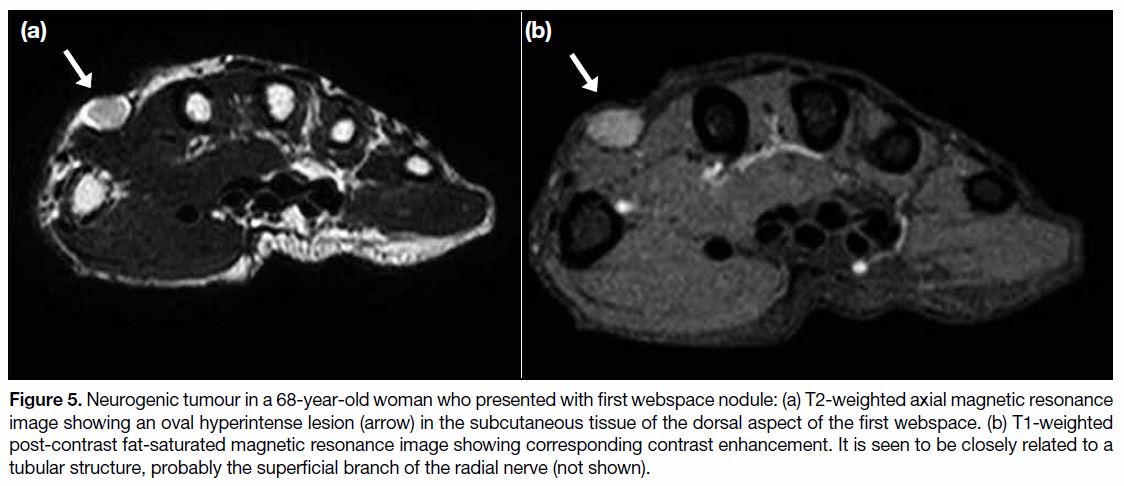
Peripheral Nerve Sheath Tumour
Benign peripheral nerve sheath tumours include schwannomas and neurofibromas. They are commonly
found in the forearm and hand region. Schwannomas
arise from the Schwann cells surrounding the nerve
whereas neurofibromas arise from the central nerve
fascicles. Schwannomas tend to occur in larger and
deeper nerves whereas neurofibromas tend to arise from
smaller cutaneous nerves.[10] Clinically, they are usually
seen in adults as a painless slow-growing mass. Most are
not associated with neurofibromatosis. Ultrasonography
shows a fusiform hypoechoic lesion with a “dural tail”
representing the entering and exiting nerve. This may be
difficult to visualise in smaller and superficial cases. On
MRI (Figure 5), they are generally of low-to-intermediate
signal intensity on T1-weighted sequence, high signal
intensity on T2-weighted sequence with homogeneous
contrast enhancement. For larger lesions, target sign with
central T2 hypointense signal may be observed, more
frequently in neurofibromas. Schwannomas can undergo
cystic or fatty degeneration. Features including large
size (>5 cm), infiltrative margins, marked heterogeneity
and rapid growth should raise concern about underlying
malignant change.[11]
Figure 5. Neurogenic tumour in a 68-year-old woman who presented with first webspace nodule: (a) T2-weighted axial magnetic resonance
image showing an oval hyperintense lesion (arrow) in the subcutaneous tissue of the dorsal aspect of the first webspace. (b) T1-weighted
post-contrast fat-saturated magnetic resonance image showing corresponding contrast enhancement. It is seen to be closely related to a
tubular structure, probably the superficial branch of the radial nerve (not shown).
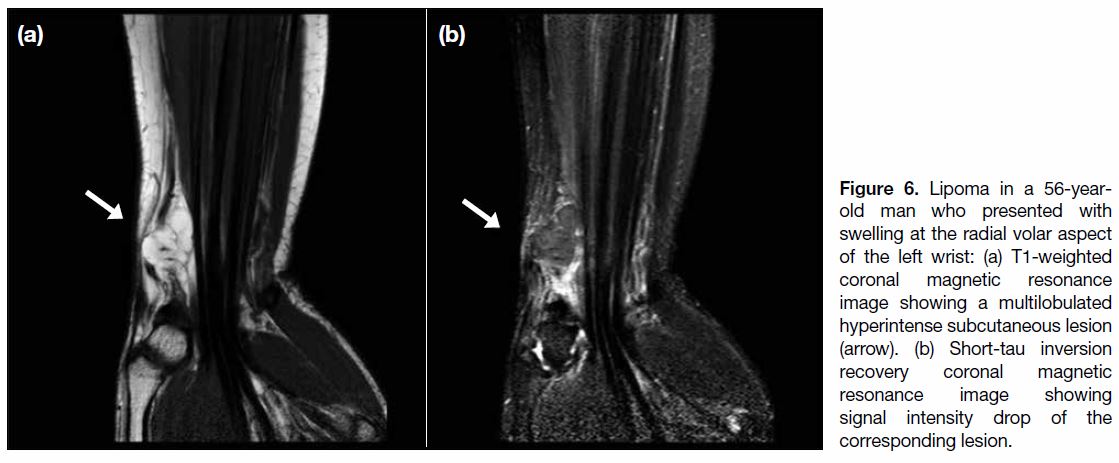
Lipoma
Lipomas are the most common soft tissue tumour in
adults. They are only occasionally seen in the hand and
wrist regions, and account for only 5% of all lipomas
occurring in the upper limb.[12] Clinically, they present
as a painless slow-growing mass, typically at the thenar or hypothenar eminence. Compression on adjacent
nerves or vessels may occur in cases where they are in a
confined space such as the carpal tunnel. Characteristic
sonographic features of a lipoma are an encapsulated
hyperechoic lesion with fine linear internal echogenic
echos.[13] However, the echogenicity may be variable.
On MRI (Figure 6), lipomas show homogeneous
hyperintense signal on T1-weighted sequence with
corresponding signal intensity drop on short-tau
inversion recovery or fat-saturated sequence. Thick
enhancing septation and nodular or a solid component
raises suspicion for atypical lipoma and liposarcoma.[14]
Figure 6. Lipoma in a 56-year-old
man who presented with
swelling at the radial volar aspect
of the left wrist: (a) T1-weighted
coronal magnetic resonance
image showing a multilobulated
hyperintense subcutaneous lesion
(arrow). (b) Short-tau inversion
recovery coronal magnetic
resonance image showing
signal intensity drop of the
corresponding lesion.
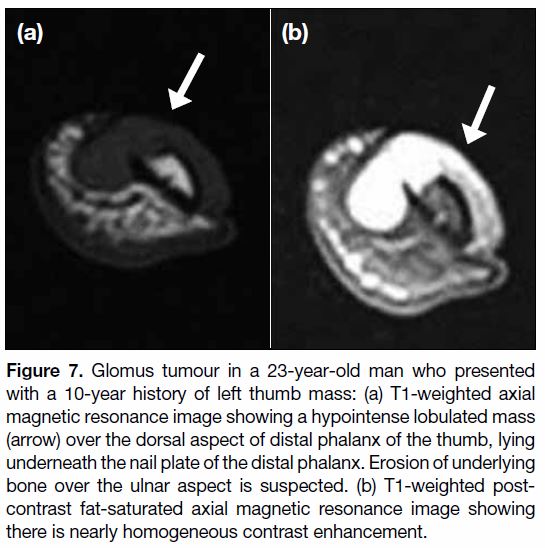
Glomus Tumours
Glomus tumours typically occur in young adults but may
occur at any age. There is no sex predilection except in
subungual lesions that are far more common in women.[7]
A glomus tumour is a benign proliferation of cells
from the glomus body that is involved in regulation of
vascular flow for temperature control. It is occasionally
seen in the hand region, accounting for about 1% of all
hand tumours.[7] Typically, they are seen as subungual
masses in the fingertips. They may present with pain,
temperature sensitivity and point tenderness.[15] Pressure
erosion may also be seen on radiographs. On ultrasound scans, they appear as a non-specific, solid, hypoechoic
mass beneath the nail, possibly with associated erosion
of the underlying phalangeal bone. The high-velocity
flow in intratumoural shunt vessels causes this lesion
to be hypervascular on colour Doppler imaging, and
is diagnostic.[16] On MRI (Figure 7), glomus tumours
demonstrate low signal intensity on T1-weighted
sequence with homogeneous hyperintense signal on
T2-weighted sequence and intense contrast enhancement.
magnetic resonance angiography is a useful non-invasive
adjunct to conventional MRI for establishing
the diagnosis of glomus tumour. Typical magnetic
resonance angiographic findings include areas of strong
enhancement in the arterial phase and tumour blush, with
increase in size in the delayed phase.[16] The characteristic
location at the subungual region with the above imaging
features allows its differentiation from other fingertip
lesions. MRI remains the imaging of choice in suspected
recurrent cases after surgery.[17]
Figure 7. Glomus tumour in a 23-year-old man who presented
with a 10-year history of left thumb mass: (a) T1-weighted axial
magnetic resonance image showing a hypointense lobulated mass
(arrow) over the dorsal aspect of distal phalanx of the thumb, lying
underneath the nail plate of the distal phalanx. Erosion of underlying
bone over the ulnar aspect is suspected. (b) T1-weighted post-contrast
fat-saturated axial magnetic resonance image showing
there is nearly homogeneous contrast enhancement.
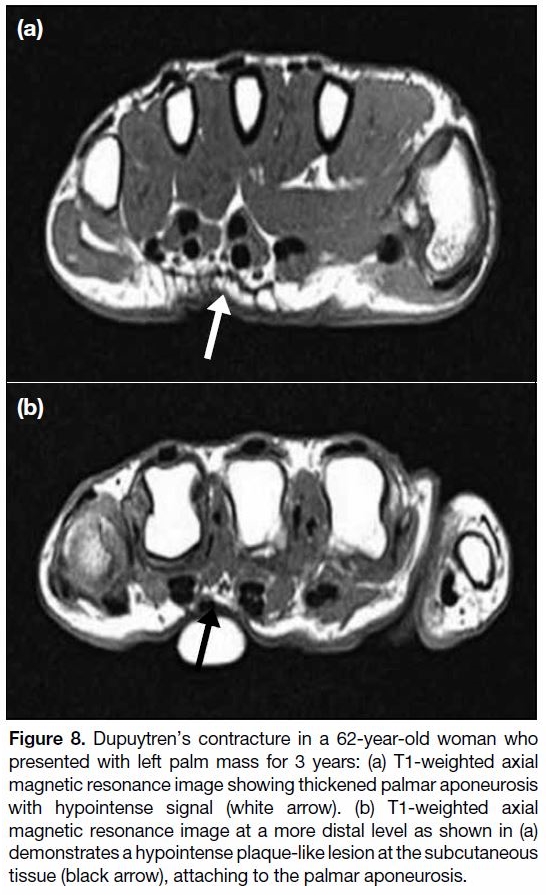
Dupuytren’s Contracture
Dupuytren’s contracture or palmar fibromatosis is a
fibrosing condition that typically presents as painless
subcutaneous nodularity over the palmar surface of the
hand.[18] The disease most commonly occurs in patients
aged >65 years with a male predominance. It is considered
the most common of the superficial fibromatoses and
is thought to affect 1% to 2% of the population. These
nodules can slowly progress to cords and bands and may
cause flexion contracture secondary to fibrous attachment to the underlying tendon sheath. On ultrasound scans, they
are seen as subcutaneous nodules superficial to the flexor
tendons. These lesions are typically found at the level
of the distal palmar crease, commonly with an epicentre
at the distal metacarpal, most commonly the fourth
digit.[19] On MRI (Figure 8), Dupuytren’s contracture is
seen as nodularity or cord-like superficial masses that
arise from the palmar aponeurosis. Typically, these
lesions are of low signal intensity on all pulse sequences
without contrast enhancement. Occasionally, they may
show intermediate signal intensity on both T1- and T2-
weighted images with contrast enhancement, possibly
due to a higher cellular component.
Figure 8. Dupuytren’s contracture in a 62-year-old woman who
presented with left palm mass for 3 years: (a) T1-weighted axial
magnetic resonance image showing thickened palmar aponeurosis
with hypointense signal (white arrow). (b) T1-weighted axial
magnetic resonance image at a more distal level as shown in (a)
demonstrates a hypointense plaque-like lesion at the subcutaneous
tissue (black arrow), attaching to the palmar aponeurosis.
Venous Malformation
Vascular malformations can be subcategorized according
to their flow dynamics into low and high flow types.[20]
Low flow types include venous, lymphatic, capillary-venous and capillary-lymphatic-venous malformations.
The presence of an arterial component indicates a high
flow lesion that includes arteriovenous malformations and arteriovenous fistulas. Venous malformation
(Figures 9 and 10) is the most common peripheral
vascular malformation, usually seen in the head and neck
region, trunk and extremities. Venous malformation
typically presents as a soft, compressible and non-pulsatile
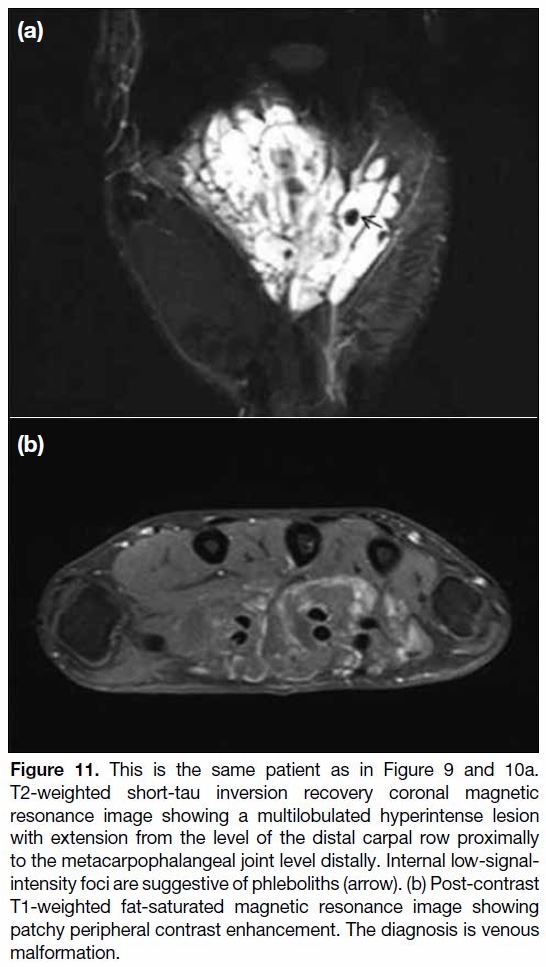
slow-growing mass. On MRI (Figure 11),
vascular malformations are seen as infiltrative lobulated
lesions without significant mass effect, with hyperintense
T2 signal and gradual enhancement on post-contrast
images. Phleboliths may be present. No flow void is
demonstrated. Delayed contrast-enhanced sequences are
also helpful in demonstrating any connection between
the malformations and deeper venous vessels. This is
an important detail to confirm prior to intervention since
these lesions have been linked to a greater risk of deep
venous thrombosis.[21]
Figure 9. An 18-year-old woman presented with right palm mass
for 1 year: Frontal radiograph of the right hand showing a tiny
opacity (arrow) over the radial aspect of the third metacarpal-phalangeal
joint. It could represent a phlebolith. Otherwise there is
no focal bone lesion.
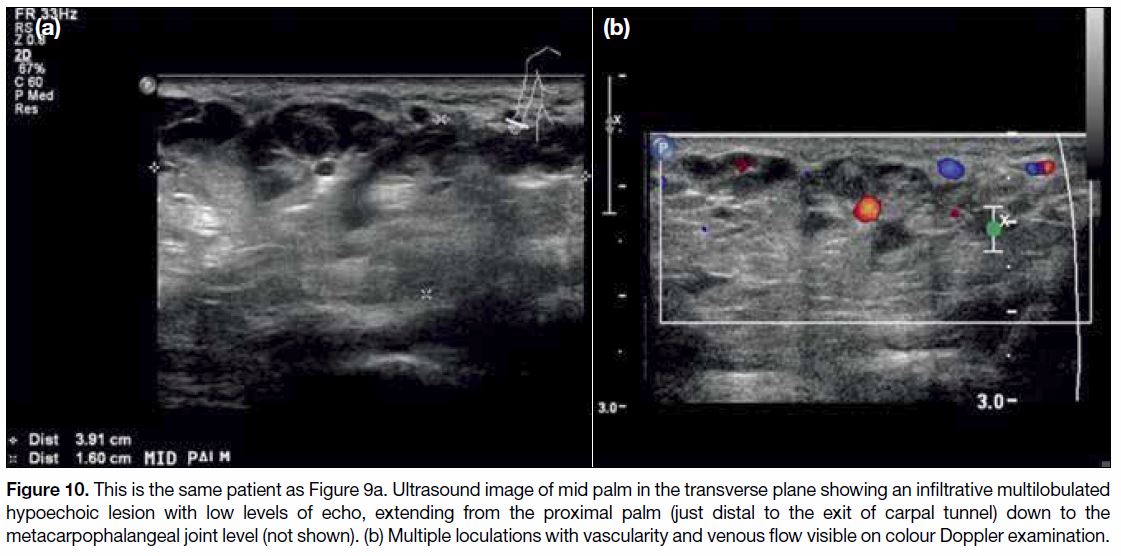
Figure 10. This is the same patient as Figure 9a. Ultrasound image of mid palm in the transverse plane showing an infiltrative multilobulated
hypoechoic lesion with low levels of echo, extending from the proximal palm (just distal to the exit of carpal tunnel) down to the
metacarpophalangeal joint level (not shown). (b) Multiple loculations with vascularity and venous flow visible on colour Doppler examination.
Figure 11. This is the same patient as in Figure 9 and 10a.
T2-weighted short-tau inversion recovery coronal magnetic
resonance image showing a multilobulated hyperintense lesion
with extension from the level of the distal carpal row proximally
to the metacarpophalangeal joint level distally. Internal low-signal-intensity
foci are suggestive of phleboliths (arrow). (b) Post-contrast
T1-weighted fat-saturated magnetic resonance image showing
patchy peripheral contrast enhancement. The diagnosis is venous
malformation.
Aneurysm/Pseudoaneurysm
Aneurysms and pseudoaneurysms in the hand are
occasionally seen in clinical practice.[22] Pseudoaneurysms
usually occur secondary to trauma but may be iatrogenic
following arterial puncture. True aneurysms are
uncommon and may be associated with underlying
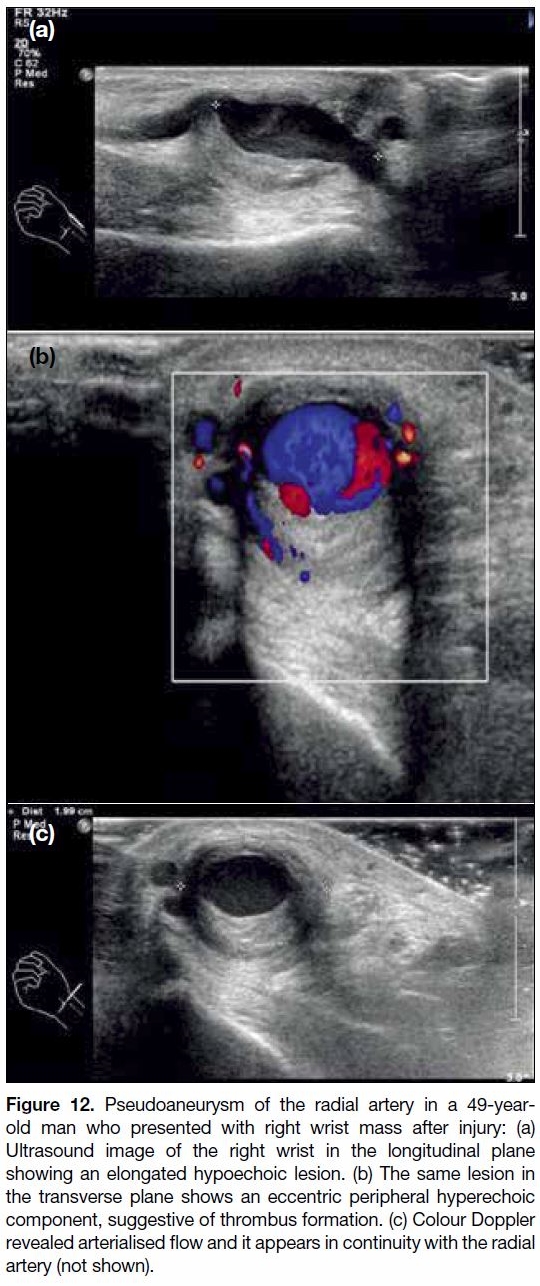
vasculitis. On ultrasound scans (Figure 12), aneurysms
and pseudoaneurysms demonstrate turbulent flow
with a characteristic yin-yang sign on colour Doppler
images. A to-and-fro pattern may be seen with pulsed
Doppler images. Signal intensity on MRI is variable,
depending on the presence of thrombus or turbulent flow.
Figure 12. Pseudoaneurysm of the radial artery in a 49-year-old
man who presented with right wrist mass after injury: (a)
Ultrasound image of the right wrist in the longitudinal plane
showing an elongated hypoechoic lesion. (b) The same lesion in
the transverse plane shows an eccentric peripheral hyperechoic
component, suggestive of thrombus formation. (c) Colour Doppler
revealed arterialised flow and it appears in continuity with the radial
artery (not shown).
Generally, aneurysms and pseudoaneurysms are slightly
hyperintense on T1- and T2-weighted sequence with
signal void. Susceptibility artefact may be demonstrated
in the presence of thrombosis. Sometimes, continuity
with the parent artery is seen. These characteristic
imaging features allow diagnosis and avoid unnecessary
and dangerous biopsy.
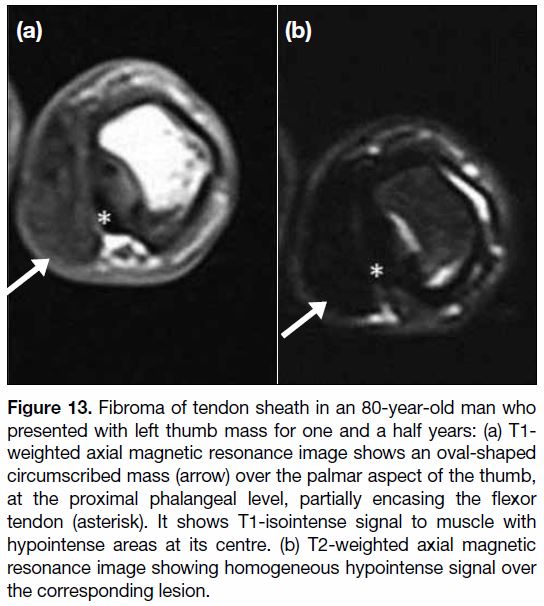
Fibroma of the Tendon Sheath
Fibroma of the tendon sheath is a rare condition and
most (around 82%) are found in the hand and wrist
region.[9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20] [21] [22] [23] It is usually seen in adults (20-50 years old)
with a male predominance. It is composed of well-circumscribed
nodules on histology that are typically
paucicellular, containing spindled fibroblasts embedded
in a collagenous stroma.[7] Clinically, fibromas manifest as painless slow-growing masses, typically well-circumscribed
and small (<3 cm) with close proximity
to a tendon or tendon sheath on imaging. On MRI
(Figure 13), fibromas typically have a signal intensity
equal to or lower than that of skeletal muscle on both
T1- and T2-weighted sequences with a variable contrast enhancement pattern.[24] However, the T2 signal can be
variable if areas of increased cellularity or myxoid change
are present.[25] No susceptibility artefact is demonstrated
on gradient echo sequence. The lack of blooming
artefact in fibroma is helpful in differentiation from giant
cell tumour of tendon sheath that may also present as a
low signal lesion on both T1- and T2-weighted sequence
on MRI. They also tend to have a lower signal on
T2-weighted images and show less enhancement with
intravenous contrast material compared with giant cell
tumour of tendon sheath.[26]
Figure 13. Fibroma of tendon sheath in an 80-year-old man who
presented with left thumb mass for one and a half years: (a) T1-weighted axial magnetic resonance image shows an oval-shaped
circumscribed mass (arrow) over the palmar aspect of the thumb,
at the proximal phalangeal level, partially encasing the flexor
tendon (asterisk). It shows T1-isointense signal to muscle with
hypointense areas at its centre. (b) T2-weighted axial magnetic
resonance image showing homogeneous hypointense signal over
the corresponding lesion.
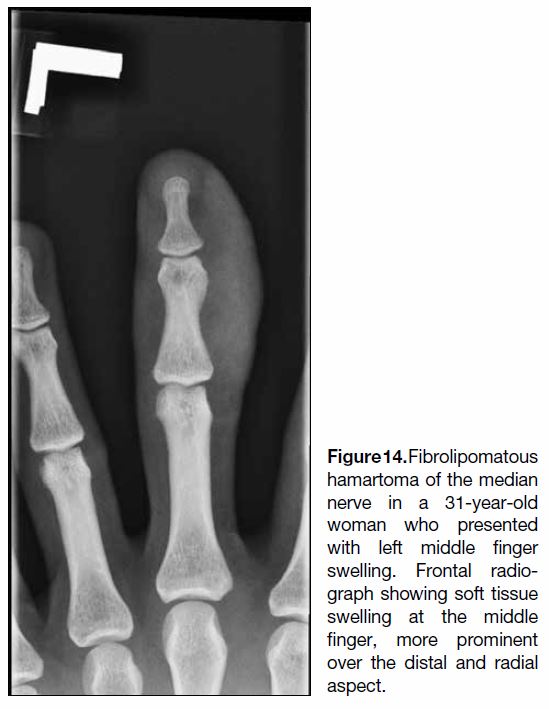
Fibrolipomatous Hamartoma
Also known as neural fibrolipoma or perineural or
intraneural lipoma, a fibrolipomatous hamartoma is
comprised of hypertrophic mature fat and fibroblasts
along the perineurium, surrounding the nerve
bundles within the nerve sheath. It is a rare benign
neoplasm leading to enlargement of the affected nerve,
with predilection at the median nerve. Clinically,
fibrolipomatous hamartomas present as slow-growing
masses at the volar aspect of the hand and wrist region.
They may be associated with macrodactyly (Figure 14),
a condition known as macrodystrophia lipomatosa.
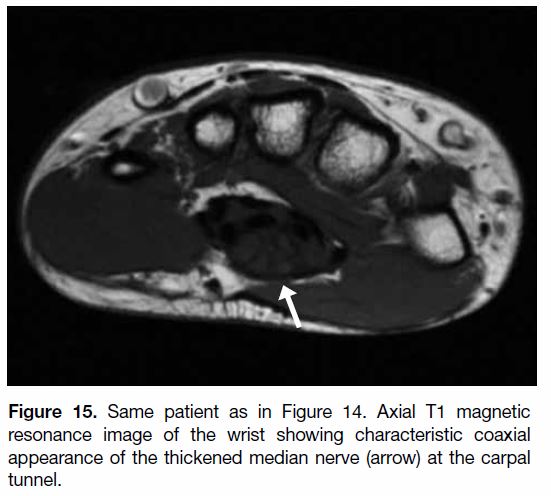
Diagnosis can be made by ultrasonography or MRI,
with longitudinally orientated fusiform structures
representing enlarged nerve fascicles, giving a spaghetti-like
appearance on coronal planes and coaxial cable appearance on axial images (Figure 15).[27] There will
be areas of high and low T1 signal intensity within the
lesion representing the fatty and fibrous components,
respectively.
Figure 14. Fibrolipomatous
hamartoma of the median
nerve in a 31-year-old
woman who presented
with left middle finger
swelling. Frontal radio-graph showing soft tissue
swelling at the middle
finger, more prominent
over the distal and radial
aspect.
Figure 15. Same patient as in Figure 14. Axial T1 magnetic
resonance image of the wrist showing characteristic coaxial
appearance of the thickened median nerve (arrow) at the carpal
tunnel.
BENIGN BONE TUMOURS
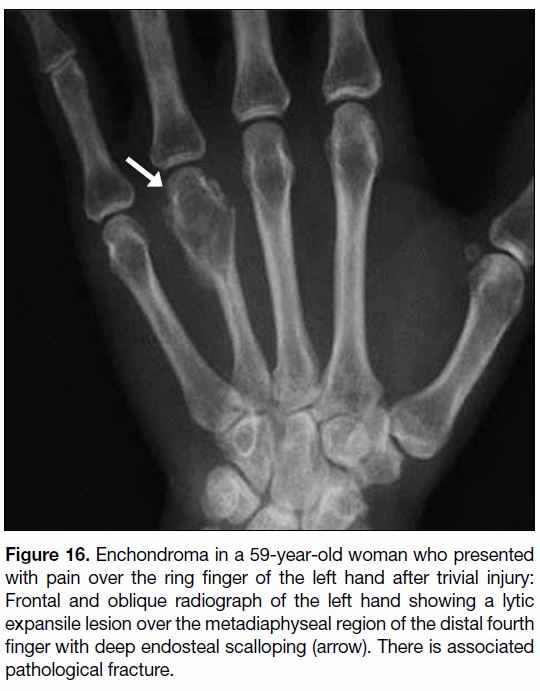
Enchondroma
Enchondroma (Figure 16) is the most common benign
bone tumour of the hand, often asymptomatic and
found incidentally on radiographs for an unrelated
indication. Associated pain should raise concern for an
underlying pathological fracture. Enchondroma in the
hand is classically lobular in contour and associated with
endosteal scalloping, commonly deep and associated
with cortical thinning and a variable degree of bone
expansion.[27] A ring and arc pattern of matrix may be
present. Malignant transformation is rare but should be
considered in cases of interval growth, local periosteal
reaction or severe new pain.[28] In the long bones, the
destruction of more than two thirds of the thickness of
the cortex in a chondroid lesion would raise concern
for underlying low-grade chondrosarcoma.[29] [30] Multiple
enchondromatosis, also known as Ollier’s disease,
typically demonstrates multiple enchondromas in the
hand with deformity. The metacarpal bones are more
frequently involved than the phalanges. Malignant
transformation has been reported in 20% to 45.8% of
pre-existing enchondromatosis cases and in 52% to 57.1%
of patients with Maffucci’s syndrome in a recent study.[31]
Figure 16. Enchondroma in a 59-year-old woman who presented
with pain over the ring finger of the left hand after trivial injury:
Frontal and oblique radiograph of the left hand showing a lytic
expansile lesion over the metadiaphyseal region of the distal fourth
finger with deep endosteal scalloping (arrow). There is associated
pathological fracture.
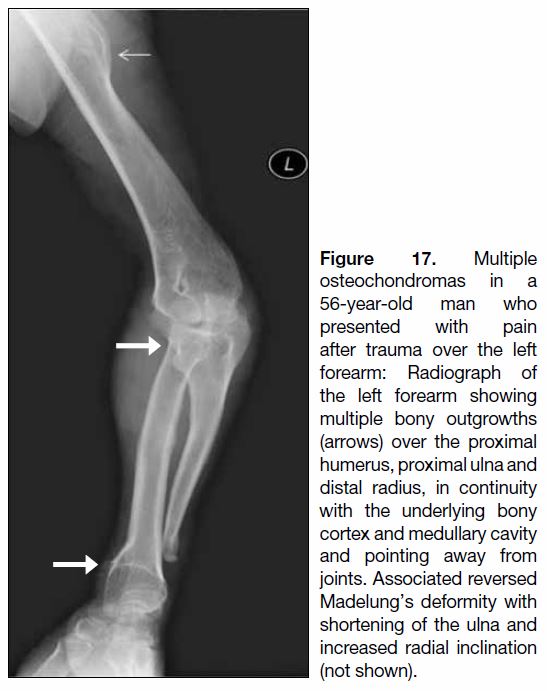
Osteochondroma
Osteochondroma is the most common bone tumour.
Around one in ten occur in the small bones of the hands
and feet.[28] It comprises cortical and medullary bone
with overlying hyaline cap, often asymptomatic and
an incidental finding on radiographs. Localised pain
may be present due to irritation of adjacent structures.
Radiographically (Figure 17), osteochondromas
are seen as a bony exostosis continuous with the
underlying parent bone cortex and medullary cavity
and pointing away from a joint. There are two forms of
osteochondromas radiographically, namely sessile and
pedunculated. Osseous continuity in the sessile type of
osteochondroma may be difficult to see on radiographs.
Multiple osteochondromas in the hand and wrist region
raises concern for underlying hereditary multiple
exostosis.
Figure 17. Multiple
osteochondromas in a
56-year-old man who
presented with pain
after trauma over the left
forearm: Radiograph of
the left forearm showing
multiple bony outgrowths
(arrows) over the proximal
humerus, proximal ulna and
distal radius, in continuity
with the underlying bony
cortex and medullary cavity
and pointing away from
joints. Associated reversed
Madelung’s deformity with
shortening of the ulna and
increased radial inclination
(not shown).
Nora’s Lesion
Nora’s lesions, also known as bizarre parosteal
osteochondromatous proliferations, are benign surface
lesions of the small tubular bones of the hand. Nora’s
lesions typically involve the metaphysis or diaphysis
of the phalanges and metacarpals. They are thought to be due to reactive heterotopic mineralisation arising
from the periosteal aspect of an intact cortex, without
involvement of the medullary canal.[28] Nora’s lesions
occurring under the nail bed are called subungual
exostosis. Radiographically (Figure 18), Nora’s lesions
are seen as broad-based ossified juxtacortical lesions,
without definite cortical or medullary continuation.[32]
Periosteal reaction is usually absent. Radiographs
alone are sufficient for diagnosis as they have a typical
radiographic appearance.[28] Computed tomography
(Figure 19) or MRI (Figure 20) scans are reserved for
cases with inconclusive radiographic findings as they better demonstrate the relationship with underlying
bone. Surgical excision is the treatment of choice but the
recurrence rate is high at 50% to 55%.[33]
Figure 18. Nora’s lesion in a 41-year-old
woman who presented with left
little finger mass: Frontal and lateral
radiographs of the left fifth finger show
an ossified lesion over the dorsal
aspect of the fifth proximal phalanx
as indicated by the metallic marker,
closely related to the underlying cortex.
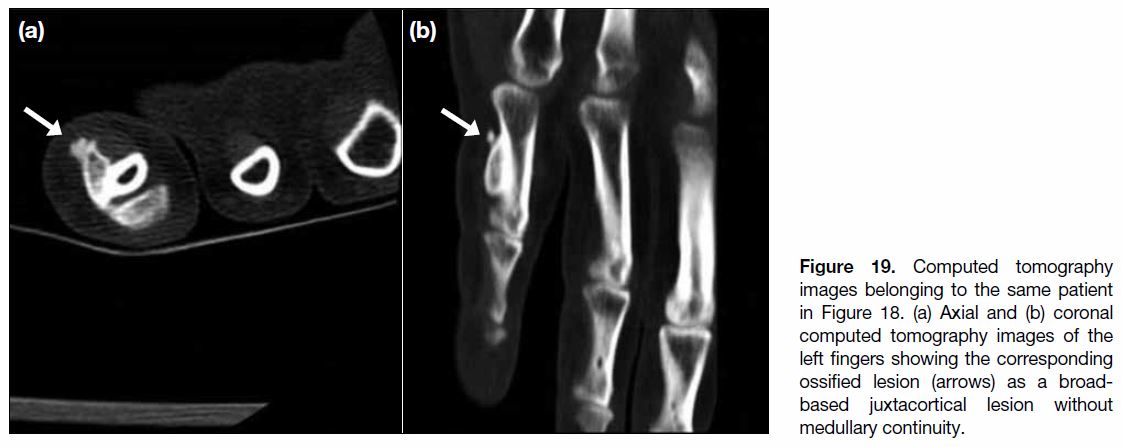
Figure 19. Computed tomography
images belonging to the same patient
in Figure 18. (a) Axial and (b) coronal
computed tomography images of the
left fingers showing the corresponding
ossified lesion (arrows) as a broad-based
juxtacortical lesion without
medullary continuity.
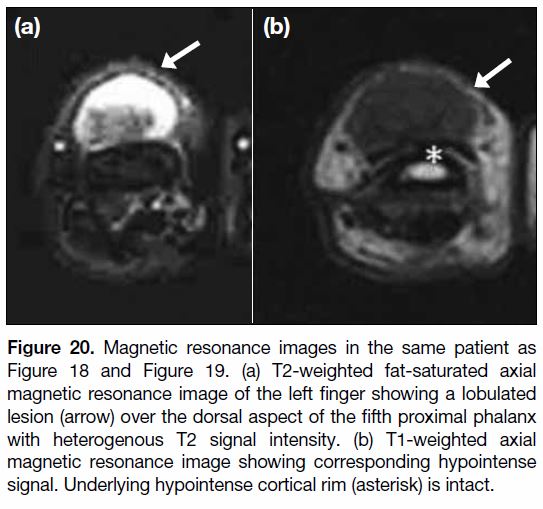
Figure 20. Magnetic resonance images in the same patient as
Figure 18 and Figure 19. (a) T2-weighted fat-saturated axial
magnetic resonance image of the left finger showing a lobulated
lesion (arrow) over the dorsal aspect of the fifth proximal phalanx
with heterogenous T2 signal intensity. (b) T1-weighted axial
magnetic resonance image showing corresponding hypointense
signal. Underlying hypointense cortical rim (asterisk) is intact.
CONCLUSION
A variety of lesions may present in the hand and
wrist region. Imaging plays an important role in their
characterisation and diagnosis. Plain radiographs remain
the first imaging of choice for patients with any complaints
in the hand and wrist region, but has a limited role in soft
tissue lesions. To investigate a soft tissue mass or swelling,
ultrasonography can be initially employed to confirm the presence of a mass lesion and differentiate cystic from
non-cystic masses. Ultrasonography can also provide
useful information about anatomical location, thereby
narrowing the differential diagnoses. In general, MRI is
the preferred modality to further characterise non-cystic
masses. For osseous lesions, computed tomography and
MRI are reserved for complex cases and/or when there
is any doubt. Knowledge of their characteristic imaging
features along with relevant clinical findings will enable
the radiologist to make a correct diagnosis and avoid the
need for invasive procedures. Some lesions have very
similar imaging characteristics and biopsy is required
to establish the diagnosis. Imaging guided percutaneous
biopsy is commonly performed for pathological analysis.
In particular, ultrasonography and computed tomography
are often used for guidance. Overall, imaging plays an
important role in the diagnostic workup of hand lesions.
It also serves as a guide for subsequent management or
surgical planning for clinicians.
REFERENCES
1. Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop
Surg. 1999;7:231-8. Crossref
2. Soren A. Pathogenesis and treatment of ganglion. Clin Orthop Relat
Res. 1966;48:173-9. Crossref
3. Vanhoenacker FM, Eyselbergs M, Van Hul E, Van Dyck P,
De Schepper AM. Pseudotumoural soft tissue lesions of the hand
and wrist: a pictorial review. Insights Imaging. 2011;2:319-33. Crossref
4. Ergun T, Lakadamyali H, Derincek A, Tarhan NC, Ozturk A.
Magnetic resonance imaging in the visualization of benign tumors
and tumor-like lesions of hand and wrist. Curr Probl Diagn Radiol.
2010;39:1-16. Crossref
5. Hong SH, Chung HW, Choi JY, Koh YH, Choi JA, Kang HS. MRI
findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol. 2006;186:961-6. Crossref
6. Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming
DJ, Walker EA. Pigmented villonodular synovitis: radiologic-pathologic
correlation. Radiographics. 2008;28:1493-518. Crossref
7. Fletcher CD, Bridge JA, Hogendoorn PC, Mertens F, editors.
World Health Organization Classification of Tumours. Pathology
and Genetics of Tumours of Soft Tissue and Bone. IARC Press:
Lyon; 2013.
8. Peh WC, Shek TW, Ip WY. Growing wrist mass. Ann Rheum Dis.
2001;60:550-3. Crossref
9. Wang C, Song RR, Kuang PD, Wang LH, Zhang MM. Giant cell
tumor of the tendon sheath: Magnetic resonance imaging findings
in 38 patients. Oncol Lett. 2017;13:4459-62. Crossref
10. Van Geertruyden J, Lorea P, Goldschmidt D, de Fontaine S,
Schuind F, Kinnen L, et al. Glomus tumours of the hand. A
retrospective study of 51 cases. J Hand Surg Br. 1996;21:257-60. Crossref
11. Baek HJ, Lee SJ, Cho KH, Choo HJ, Lee SM, Lee YH, et.al.
Subungual tumors: clinicopathological correlation with US and
MR imaging findings. Radiographics. 2010;30:1621-36. Crossref
12. Theumann NH, Goettmann S, Le Viet D, Resnick D, Chung CB,
Bittoun J, et al. Recurrent glomus tumors of fingertips: MR imaging
evaluation. Radiology.2002;223:143-51. Crossref
13. Chung EB, Enzinger FM. Fibroma of tendon sheath. Cancer.
1979;44:1945-54. Crossref
14. Dinauer PA, Brixey CJ, Moncur JT, Fanburg-Smith JC,
Murphey MD. Pathologic and MR imaging features of benign
fibrous soft-tissue tumors in adults. Radiographics. 2007;27:173-87. Crossref
15. Fox MG, Kransdorf MJ, Bancroft LW, Peterson JJ, Flemming DJ.
MR imaging of fibroma of the tendon sheath. AJR Am J
Roentgenol. 2003;180:1449-53. Crossref
16. Vassallo P. Diagnostic imaging of mass lesions in the hand. The
Synapse. 2015;14;29-31.
17. Murphey MD, Ruble CM, Tyszko SM, Zbojniewicz AM,
Potter BK, Miettinen M. From the archives of the AFIP:
musculoskeletal fibromatoses: radiologic-pathologic correlation.
Radiographics. 2009;29:2143-73. Crossref
18. Morris G, Jacobson JA, Kalume Brigido M, Gaetke-Udager K,
Yablon CM, Dong Q. Ultrasound features of palmar fibromatosis
or Dupuytren contracture. J Ultrasound Med. 2019;38:387-92. Crossref
19. Kransdorf MJ. Benign soft-tissue tumors in a large referral
population: distribution of specific diagnoses by age, sex, and
location. AJR Am J Roentgenol. 1995;164:395-402. Crossref
20. Paunipagar BK, Griffith JF, Rasalkar DD, Chow LT, Kumta SM,
Ahuja A. Ultrasound features of deep-seated lipomas. Insights
Imaging. 2010;1:149-53. Crossref
21. Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated
liposarcomas (atypical lipomas): results of MRI
evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol.
2004;182:733-9. Crossref
22. Marom EM, Helms CA. Fibrolipomatous hamartoma: pathognomonic
on MR imaging. Skeletal Radiol. 1999;28:260-4. Crossref
23. The J. Ultrasound of soft tissue masses of the hand. J Ultrason.
2012;12:381-401. Crossref
24. Abreu E, Aubert S, Wavreille G, Gheno R, Canella C, Cotton A.
Peripheral tumor and tumor-like neurogenic lesions. Eur J Radiol.
2013;82:38-50. Crossref
25. Flors L, Leiva-Salinas C, Maged IM, Norton PT, Matsumoto AH,
Angle JF, et.al. MR imaging of soft-tissue vascular malformations:
diagnosis, classification, and therapy follow-up. Radiographics.
2011;31:1321-40. Crossref
26. Madani H, Farrant J, Chhaya N, Anwar I, Marmery H, Platts A, et al.
Peripheral limb vascular malformations: an update of appropriate
imaging and treatment options of a challenging condition. Br J Radiol. 2015;88:20140406. Crossref
27. Millender LH, Nalebuff EA, Kasdon E. Aneurysms and thromboses
of the ulnar artery in the hand. Arch Surg. 1972;105:686-90. Crossref
28. Douis H, Saifuddin A. The imaging of cartilaginous bone tumours.
I. Benign lesions. Skeletal Radiol. 2012;41:1195-212. Crossref
29. Melamud K, Drapé JL, Hayashi D, Roemer FW, Zentner J,
Guermazi A. Diagnostic imaging of benign and malignant osseous
tumors of the fingers. Radiographics. 2014;34:1954-67. Crossref
30. Larbi A, Viala P, Omoumi P, Lecouvet F, Malghem J, Cyteval C,
et al. Cartilaginous tumours and calcified lesions of the hand: a
pictorial review. Diagn Interv Imaging. 2013;94:395-409. Crossref
31. Herget GW, Strohm P, Rottenburger C, Kontny U, Krauß T,
Bohm J, et al. Insights into enchondroma, enchondromatosis and
the risk of secondary chondrosarcoma. Review of the literature
with an emphasis on the clinical behaviour, radiology, malignant
transformation and the follow up. Neoplasma. 2014;61:365-78. Crossref
32. Dhondt E, Oudenhoven L, Khan S, Kroon HM, Hogendoorn PC,
Nieborg A, et al. Nora’s lesion, a distinct radiological entity.
Skeletal Radiol. 2006;35:497-502. Crossref
33. Joseph J, Ritchie D, MacDuff E, Mahendra A. Bizarre parosteal
osteochondromatous proliferation: a locally aggressive benign
tumor. Clin Orthop Relat Res. 2011;469:2019-27. Crossref
| Attachment | Size |
|---|---|
| v23n4_Benign.pdf | 516.8 KB |