Setting Standards for Judging the Rapid Film Reporting Section in Postgraduate Radiology Assessment: a Feasibility Study
ORIGINAL ARTICLE
Setting Standards for Judging the Rapid Film Reporting Section in Postgraduate Radiology Assessment: a Feasibility Study
AF Abdul Rahim1, NS Roslan1, IL Shuaib2, MS Abdullah3, KA Sayuti3, H Abu Hassan4
1 Department of Medical Education, School of Medical Sciences, Universiti Sains Malaysia, Malaysia
2 Department of Radiology, Advanced Medical and Dental Institute, Universiti Sains Malaysia, Malaysia
3 Department of Radiology, School of Medical Sciences, Universiti Sains Malaysia, Malaysia
4 Department of Radiology, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Malaysia
Correspondence: Dr AF Abdul Rahim, Department of Medical Education, School of Medical Sciences, Universiti Sains Malaysia,
Malaysia. Email: fuad@usm.my
Submitted: 8 Mar 2020; Accepted: 4 Jun 2020.
Contributors: AFAR and NSR designed the study. ILS, MSA, KAS, and HAH acquired the data. AFAR, NSR analysed the data. AFAR, NSR,
ILS, and HAH drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access
to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: The study was granted an exemption from ethical approval from the Human Research Ethics Committee USM. The participants
were treated in accordance with the tenets of the Declaration of Helsinki. The participants provided written informed consent for all data
collection.
Abstract
Objective
We investigated the feasibility of applying a standard-setting procedure for the rapid film reporting
examination of the Malaysian National Conjoint Board of Radiology.
Methods
We selected the modified Angoff standard-setting process. Judges were nominated and trained, performance
categories were discussed, and judges’ ratings on films were collected after an iterative procedure. The process was
then evaluated for evidence of validity.
Results
A cut-off score of 92% resulted, compared with the 80% usually used. Judges were satisfied with the training
and understood the procedure and their roles. In all, 27.3% felt that time given for the task was not sufficient. A
total of 54.5% of judges thought the final passing cut-off score of 92% was too high, and 27.3% were not confident
regarding its appropriateness. The inter-rater reliability was 0.928. External comparison with a ‘gold standard’ of
supervisor ratings revealed a sensitivity of 0.25 and specificity of 1.00 compared with the traditional cut-off score
having a sensitivity of 0.92 and specificity of 0.33. In this kind of situation, high specificity is considered to be more
important than high sensitivity.
Conclusion
Standard setting for the rapid film reporting examination using the modified Angoff method was feasible
with robust procedural, internal, and external validity evidence. Areas for improvement were identified to address
the perceived high cut-off score obtained and improve the overall process.
Key Words: Education, medical; Preceptorship; Psychometrics; Radiology; Teacher training
中文摘要
於放射科培訓醫生的快速放射影像報告考核中使用標準設定:可行性研究
AF Abdul Rahim、NS Roslan、IL Shuaib、MS Abdullah、KA Sayuti、H Abu Hassan
目的
檢視馬來西亞國家放射學聯合委員會以設定快速放射影像報告考核標準的可行性。
方法
採用改良版Angoff標準設定法,獲提名考官須經過培訓、討論考核表現類別,並以迭代程序收集考官對放射影像片子的評級,然後對該程序進行有效性評估。
結果
跟一般使用的劃割分數80%相比,本研究的劃割分數為92%。考官對培訓感到滿意,並且
理解過程和他們的角色。當中,27.3%認為完成任務時間不足,54.5%認為最終合格分數過高(即
92%),27.3%對這個合格分數的適當性存疑。評分者間一致度信度為0.928。與主管級醫師評級的
「黃金標準」進行外部比較時,使用劃割分數92%的靈敏度為0.25,特異性為1.00;使用傳統劃割分
數(即80%)的靈敏度則為0.92,特異性為0.33。在這種情況下,高特異性比高靈敏度更為重要。
結論
基於過程上、內部和外部的可靠效度,快速放射影像報告考核中使用改良版Angoff標準設定
法是可行的。研究也就劃割分數過高提出改進之處,以改善整個程序。
INTRODUCTION
Assessment in medical education is an important
undertaking; one of its goals is protecting the public by
upholding high professional standards.[1] Over the past
two decades, medical schools and postgraduate training
bodies have put in rigorous efforts to provide valid
assessment in certifying physicians. This is guided by
the current view of validity as a hypothesis that must be
supported by evidence.[2]
The Malaysian National Conjoint Board of Radiology,
responsible for the training of radiologists in Malaysia,
has recently embarked on gradually improving the
assessment of its graduates. The establishment of
standard setting of the assessment procedure is a priority
area.
The 4-year training programme is currently divided into
three phases. Phase I is the first year, phase II covers
the second and third years, and the fourth year is phase
III. Assessment is divided into continuous and end-of-phase professional examinations. Examinations in
Phase I include a multiple true-false (Type X) question
examination, an objective structured clinical examination,
an objective structured practical examination, and an oral
examination. In Phase II the professional examinations
include multiple-choice tests, film reporting, and an oral
examination. The final Phase III examinations include a
rapid film reporting examination, a dissertation, and an oral examination based on the dissertation project.
The rapid film reporting examination simulates the
typical day-to-day tasks of a radiologist, who has to
review numerous radiographs in a short time, particularly
in emergency medicine and general practice situations.[3]
The examination requires candidates to view several
radiographs within a specified amount of time and report
on the findings. In the Malaysian setting, candidates
need to report on 25 radiographs within 30 minutes.
For each film, they have to state whether it is normal or
abnormal; and if abnormal, then they have to describe the
abnormalities seen. The Royal College of Radiologists in
the United Kingdom has reported using rapid reporting
sessions as part of their examinations.[3]
The Board feels that, as part of the final-year high-stakes
exit examination, the rapid film reporting
examination also requires standard setting of its cut-off
score.
This article reports on a pilot study of standard setting
of the rapid film reporting examination of the Malaysian
National Conjoint Board of Radiology. To our
knowledge, there is no literature reporting on standard
setting of this particular method of assessment. We hope
this report will be useful for radiology postgraduate
training institutions employing similar assessment
modalities.
METHODS
A workshop to introduce members of the board to
standard-setting principles and practice was held in
April 2019. The workshop was organised with the help
of the Medical Education Department from one of the
participating universities.
A standard-setting meeting was organised before the
rapid film reporting examination in the exit examination
for Year 4 candidates in May 2019. It was chaired by one
of the authors, ILS.
An eight-step standard-setting planning process was
followed.[4]
Selection of a Standard-Setting Method
Modified Angoff is one of the standard-setting methods
that offers a systematic procedure in estimating
performance standard at the pass-fail level.[5] It has been
used in various high-stakes examinations as it offers the
best balance between technical adequacy and feasibility.[6]
The Modified Angoff method was selected for this
examination as it is an absolute standard-setting method — the candidates are judged against defined standards
rather than cohort performance. This is achieved by
asking qualified and trained judges to review test items
or prompts before the examination is administered.
Although the process can be time-consuming and labour-intensive,
it is relatively easier and more flexible than
other test-based methods. It is supported by a strong body
of evidence in the literature and has wide applicability to
many formats.[7]
In the modified Angoff method, judges review items
(questions) used in the assessment, discuss and agree on
the characteristics of a borderline candidate, and assess
the likely performance of borderline candidates for each
item. The mean of the judges’ estimates for all items is
taken as the cut-off score for that particular assessment.[4]
Selection of Judges
The selection of qualified judges is critical for an
absolute standard-setting method.[4] The following criteria
are recommended: content expertise, familiarity with the
target population, understanding of the task of judging
as well as the content materials, being fair and open-minded,
willingness to follow directions, lack of bias,
and willingness to devote their full attention to the task.
A total of 11 judges were chosen after considering the
above criteria.
Preparation of Descriptions of Performance
Categories
Judges need to have a clear understanding of the
performance categories, which are ‘narrative descriptions
of the minimally acceptable behaviours required in order
to be included in a given category’[4] to enable them to
distinguish between different levels of performance.
In licensing and certification situations, the focus is often
on discussion and description of a ‘borderline candidate’.[8]
Candidates who equal or exceed the performance of
these borderline candidates are then deemed ‘pass’ while
those who perform worse are deemed ‘fail’.
The group discussed the characteristics of a borderline
candidate in the setting of the Radiology Master of
Medicine course and agreed that: ‘A borderline candidate
of the exit examination should demonstrate basic
knowledge for safe clinical decision and management,
is able to work under minimal supervision, is equipped
with basic radiological skills and conducts himself/
herself professionally.’
Training of Judges
The definition of the borderline candidate appears
straightforward, but judges often find it difficult to
come up with an actual mark after reading a question
while thinking like a borderline student.[4] Judges need
familiarisation with the procedure and in generating
ratings. Training judges, therefore, is given priority and
can take more than one day.[9]
In our situation, apart from attending the introductory
workshop mentioned above, judges were also briefed by
the department chairperson at the beginning of the exercise.
The objectives, procedures for standard setting, and the
definition of a borderline candidate were discussed.
Collection of Ratings or Judgements
All 25 films used in the rapid film reporting examination,
together with the answers, were shown in the standard-setting
session. Each film was shown for 10 seconds
and judges were asked to individually decide, “Will a
borderline candidate be able to decide whether this film
is normal or abnormal? If abnormal, will they be able to
describe the abnormality in full?” Based on the answers
to these questions the judges calculated the scores
obtained by their hypothetical borderline candidates.
Judges then announced the scores verbally in turn and
their judgements were recorded immediately in a pre-prepared
Excel file by an assistant.
The rating of one film by judges and the collection
of their judgements was considered as one round of
standard setting.
Provision of Feedback and Facilitation of
Discussion
We included a discussion session after each round of
judgement. The completed spreadsheet was projected to
a screen where judges could see their standing relative
to the other judges. This ‘normative information’ helps
judges generate relevant and realistic cut-off scores.[8]
Ratings at the extreme ends were then discussed. A
second round of standard setting followed, where judges
were then allowed to revise their ratings. This step of
feedback and discussion followed by a second round of
ratings is known as an ‘iterative procedure’.[4]
Evaluation of the Standard-Setting
Procedure
There are three main sources of evidence to support
the validity of a standard-setting procedure: procedural
evidence, internal evidence, and external evidence.[4]
For procedural evidence, we reviewed the practicality
and implementation of the exercise and obtained
feedback from the judges involved. To this end, an
online questionnaire, taken from Yudkowsky et al[4] was
administered. It looked at judges’ perceptions of their
orientation, training, and implementation as well as their
confidence in the resulting cut-off scores.
Internal evidence was evaluated by calculating the inter-rater
reliability, the standard deviation of judge scores
(judgement SD), and the standard deviation of examinee
test scores (test SD). The judgement SD should be no
more than 25% of the test SD.[10]
Provision of Results, Consequences and
Validity Evidence to Decision-Makers
For the external evidence, we looked at the aspect of
reasonableness which is ‘…the degree to which cut-off
scores derived from the standard-setting process
classify examinees into groups in a manner consistent
with other information about the examinees’.[11] We
adapted the ‘diagnostic performance’ approach used
by Schoonheim-Klein et al[12] whereby two clinical
supervisors in each participating university were asked
to independently rate their candidates’ ability in rapid
reporting on a four-point scale: excellent, borderline
pass, borderline fail, and poor. The supervisors, who
observe their supervisees over a prolonged time period,
were guided by a rubric for each decision. To ensure
credible ratings, they were informed that their ratings were not a measure of supervision quality and would
not contribute to the candidates’ examination marks.
Candidates rated as ‘poor’ and ‘borderline fail’ were
grouped as ‘incompetent’, and those rated as ‘borderline
pass’ and ‘excellent’ were grouped as ‘competent’. This
clinical rating (considered as the ‘true qualification’)
was then compared with the pass-fail classification
obtained from the standard-setting method under study
to get the rate of ‘false positives’ and ‘false negatives’.
We also calculated the sensitivity and specificity for the
traditional and standard-setting–derived passing mark.
Sensitivity is defined as the ability of the standard-setting–
derived passing mark to correctly identify the
competent candidates or the true-positive rate. On the
other hand, specificity is defined as the ability of the
mark to correctly eliminate the incompetent candidates,
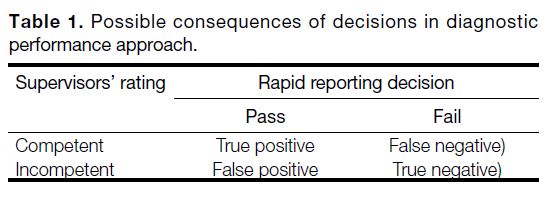
or true-negative rate. Table 1 summarises these concepts
and the formulas used to arrive at the decisions.
Table 1. Possible consequences of decisions in diagnostic
performance approach.
Provision of Results, Consequences and
Validity Evidence to Decision-Makers
Ultimately, policymakers set the standards, not the
judges.[8] As this is a pilot study, the validity data were
presented to the board to help decide on the adoption of
the standard-setting procedure.
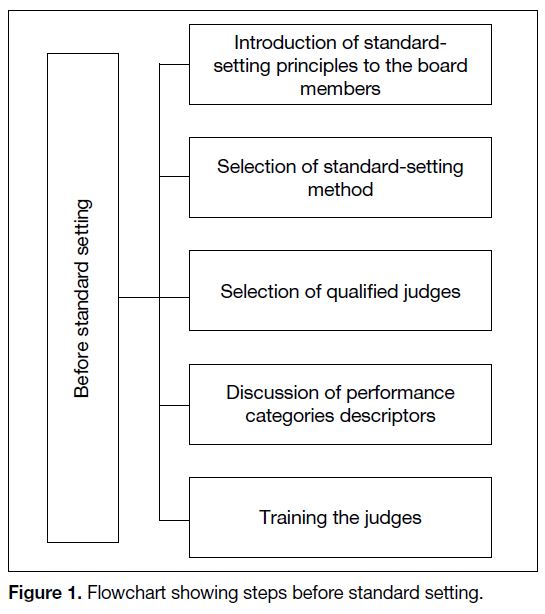
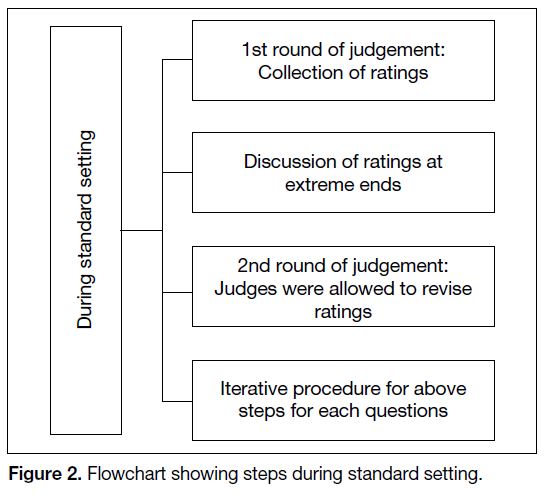
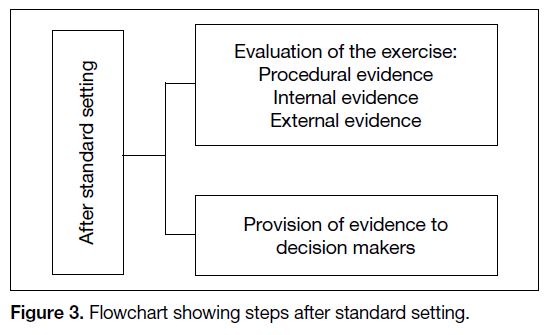
A summary of these procedures is given as steps before
(Figure 1), during (Figure 2) and after (Figure 3) the
standard-setting procedure.
Figure 1. Flowchart showing steps before standard setting.
Figure 2. Flowchart showing steps during standard setting.
Figure 3. Flowchart showing steps after standard setting.
RESULTS
Procedural Evidence
A cut-off score of 0.95 (95%) was obtained for the
first round, and 0.92 (92%) for the second round. The
traditional passing mark of the rapid film reporting was
80%.
Eleven judges provided feedback via the online
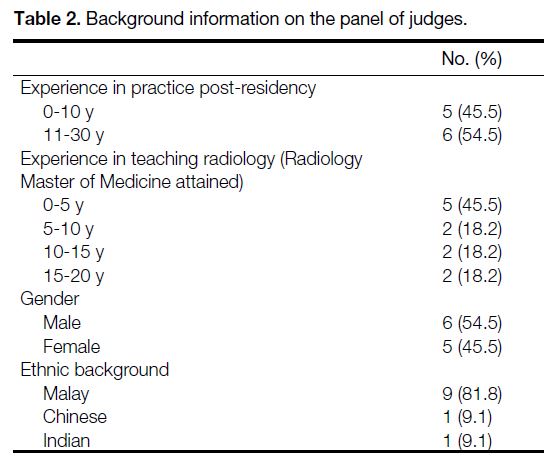
questionnaire. The panel was comprised of an almost
equal number of junior (<10 years of post-residency
practice and <5 years of involvement in teaching the
Radiology Master of Medicine course) and senior members. The same can be said of gender distribution.
The majority of panel members were ethnic Malay
(Table 2).
Table 2. Background information on the panel of judges.
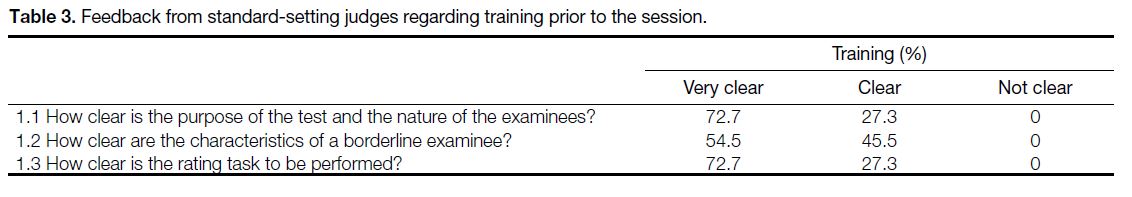
As regards feedback from judges about the training
and orientation that was provided before the session,
judges were generally clear about the purpose of the
test, the nature of the examinees, the characteristics of a
borderline candidate, and the rating task to be performed
(Table 3).
Table 3. Feedback from standard-setting judges regarding training prior to the session.
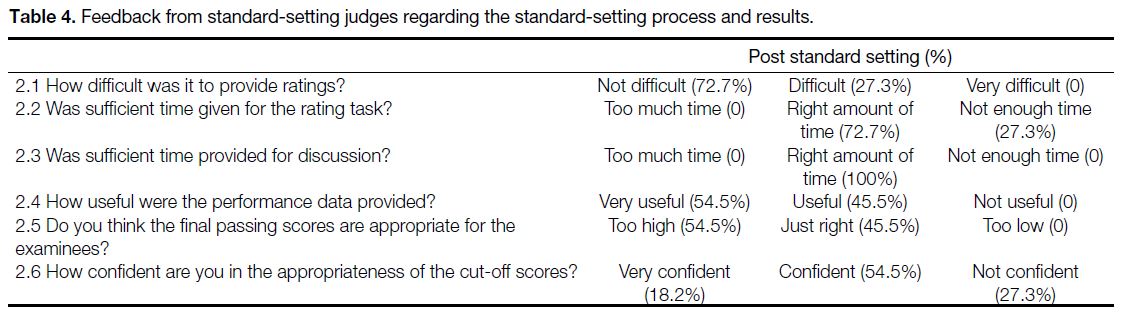
In terms of feedback from judges regarding the process
of standard setting, the majority were positive (Table 4).
Interesting points to note included the time given for
the rating task, where a minority (27.3%) felt that it
was insufficient. Slightly over half (54.5%) of judges
thought that the final passing score of 92% was too high.
A minority (27.3%) were not confident regarding the
appropriateness of the cut-off score.
Table 4. Feedback from standard-setting judges regarding the standard-setting process and results.
Internal Evidence
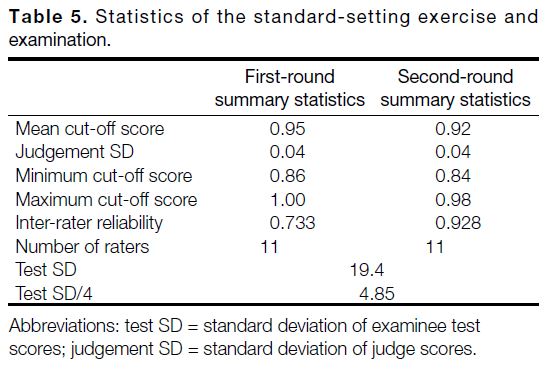
As stated above, cut-off scores of 0.95 and 0.92 were
obtained in the first and second rounds, respectively
(Table 5). The judgement SD was 0.04 on both rounds
while the test SD was 19.4. Inter-rater reliability
was 0.733 and 0.928 for the first and second rounds,
respectively.
Table 5. Statistics of the standard-setting exercise and examination.
External Evidence
As the ‘diagnostic performance approach’ assumes the
supervisors’ rating to be the gold standard, we calculated
the inter-rater reliability of the two supervisors. Cohen’s
kappa revealed a good agreement between the two
supervisors at κ = 0.780, p < 0.001.
The supervisors’ rating classified 24 candidates as
‘competent’ and three candidates as ‘incompetent’. As
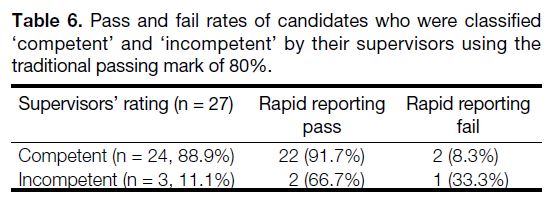
illustrated in Table 6, the traditional passing score of
80% resulted in a passing rate of 91.7% and a failure rate
of 8.3% among competent candidates. It is interesting
to note the occurrence of false-positives, where two
incompetent candidates passed the assessment. Only one
out of three incompetent candidates failed the assessment
using the traditional passing score. The sensitivity and
specificity for this passing score were found to be at 0.92
and 0.33, respectively.
Table 6. Pass and fail rates of candidates who were classified
‘competent’ and ‘incompetent’ by their supervisors using the traditional passing mark of 80%.
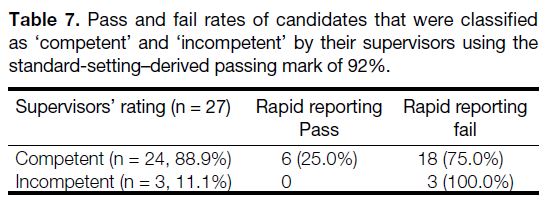
On the other hand, as per Table 7, using the standard-setting–
derived passing score of 92% resulted in a
25% passing rate among competent candidates. No incompetent candidates passed the assessment but there
was a high false-negative occurrence where 75% of
competent candidates failed the assessment. All three
incompetent candidates failed the assessment. This gives
this passing score a sensitivity of 0.25 and specificity of
1.00.
Table 7. Pass and fail rates of candidates that were classified
as ‘competent’ and ‘incompetent’ by their supervisors using the standard-setting–derived passing mark of 92%.
DISCUSSION
The main aim of this pilot study was to assess the
validity of the standard-setting procedure for the rapid
film reporting examination. The current concept of validity is the accumulation of evidence to support or
refute a particular interpretation or use of examination
data.[13] In the context of standard setting, we looked at
the procedural, internal, and external evidence to support
the validity of our rapid film reporting standard-setting
exercise[8] and generally found the results encouraging.
Procedurally, the process was feasible and practical.
No major hurdles were encountered in the planning
as well as preparation of the standard-setting exercise,
including the physical setting. The positive responses
from judges regarding implementation of points raised
in the questionnaire provided additional evidence of the
credibility of the standard-setting process.[8]
We take note that thorough and meticulous documentation
of the procedure is critical.[9] This includes the summary
of judges’ background information, which includes
speciality and teaching experience, as shown in Table 2.
The background and experiential composition of
the judges’ panel should be determined before their
nomination.[9]
It is interesting to note that slightly more than half of the
judges (54.5%) believed that the cut-off score obtained
was too high. Despite that, only 27.3% of judges were
not confident of the cut-off score obtained. We need to
differentiate between the perception of judges that the
cut-off score is high from actual unrealistically high
cut-off scores. The clarity of the judges regarding their
role and the nature of the candidates, as well as their
confidence in the cut-off score, are more in favour of the
former. The latter is noted to happen in many standardsetting
situations, particularly using the Angoff method
when judges are not given performance data.[4]
Still, the issue of producing a cut-off score that is too high
needs to be addressed, as it may hinder the acceptance of
standard setting in the future. One approach is to increase
the quality and efficiency of all the eight steps of standard
setting described in the methodology, especially the types
of feedback given to the judges during step 6 (Provision
of Feedback and Facilitation of Discussion). In our case,
the judges’ relative standing to each other, known as
normative information, were revealed following the first
round. The literature also describes providing judges
with information about actual candidate performance
on each item (reality information) and the consequences
of the generated cut-off scores (impact information).[8]
To have these kinds of information available, however,
requires the standard-setting procedure to be done after the actual examination. Another approach is to adjust the
cut-off score using the standard error of measurement of
the test. If false-negative decisions (failing competent
candidates) are of concern, then the cut-off score can be
lowered by one standard error of measurement.[4]
The internal evidence of validity includes the high inter-rater
reliability of the judgements, which was 0.733 for
the first round and 0.928 for the second round. Reliability
≥0.9 is needed for very-high-stakes examinations.[14] It is
worth noting that the reliability increased from 0.7 to 0.9
in the second round, supporting the value of the iterative
procedure in standard setting.
The judgement SD was small (0.04), less than the
recommended limit, which is 25% of the standard
deviation of the examinee test scores[10]; in this case,
4.85. Several factors may have contributed to this. One
is that all films to be used for the examination were
standardised in the session, instead of just sampling some
films. Another possible factor is the adequate number of
judges, 11 in this case. The recommended number is 10
to 12 judges.[4]
The sensitivity and specificity testing has shown the
value of standard setting in establishing consequential
validity evidence, discussed as part of ‘reasonableness’
in standard-setting literature.[9] In this exercise, using
the traditional passing mark of 80% resulted in three
incompetent candidates passing the assessment. For
high-stakes assessment such as the exit examination,
high specificity is considered to be more important
than high sensitivity. This is because re-examination
can correct the false-negative occurrences but not the
false-positive candidates who may practise unsafely
below the desired standards.[12] However, as judges have
been shown to naturally produce higher passing scores
in Angoff exercises, future practice could improve with
more training sessions, a more detailed discussion of the
borderline standards, and using performance data during
the judging process as a control measure.[12] [15] [16]
CONCLUSION
In summary, we are encouraged by the findings of
this standard-setting feasibility study of the rapid film
reporting examination. It appears feasible and seems to
have good procedural, internal, and external validity.
Areas of potential improvement include more judge
training and providing more feedback data to judges. We
look forward to its official implementation in the near
future.
REFERENCES
1. Epstein RM. Assessment in medical education. N Engl J Med. 2007;356:387-96. Crossref
2. Beckman TJ, Cook DA, Mandrekar JN. What is the validity
evidence for assessments of clinical teaching? J Gen Intern Med.
2005;20:1159-64. Crossref
3. Booth TC, Martins RD, McKnight L, Courtney K, Malliwal R.
The Fellowship of the Royal College of Radiologists (FRCR)
examination: a review of the evidence. Clin Radiol. 2018;73:992-8. Crossref
4. Yudkowsky R, Downing SM, Tekian A. Standard Setting. In:
Yudkowsky R, Park YS, Downing SM, editors. Assessment in
Health Professions Education. 2nd ed. New York: Routledge; 2020:
p 86-105. Crossref
5. Shulruf B, Wilkinson T, Weller J, Jones P, Poole P. Insights into
the Angoff method: results from a simulation study. BMC Med
Educ. 2016;16:134. Crossref
6. Cizek GJ, Bunch MB. The Angoff method and Angoff variations.
In: Cizek GJ, Bunch MB, editors. Standard Setting. California:
Sage Publications; 2011: p 81-95.
7. Plake BS, Cizek GJ. Variations on a theme. ¬The modified Angoff,
extended Angoff and Yes/No standard setting methods. In: Cizek
GJ, editor. Setting Performance Standards: Foundations, Methods,
and Innovations. 2nd ed. New York: Routledge; 2012: p 181-99.
8. Cizek GJ, Earnest DS. Setting performance standards on tests. In:
Lane S, Raymond MR, Haladyna TM, editors. Handbook of Test
Development. 2nd ed. New York: Routledge; 2016; p 212-37.
9. Hambleton RK, Pitoniak MJ, Coppella JM. Essential steps in
setting performance standards on educational tests and strategies
for assessing the reliability of results. In: Cizek GJ, editor. Setting
Performance Standards: Foundations, Methods, and Innovations.
2nd ed. New York: Routledge; 2012: p 47-76.
10. Meskauskas JA. Setting standards for credentialing examinations:
an update. Eval Health Prof. 1986;9:187-203. Crossref
11. Cizek GJ. The forms and functions of evaluations in the standard
setting process. In: Cizek GJ, editor. Setting Performance
Standards: Foundations, Methods, and Innovations. 2nd ed. New
York: Routledge; 2012; p 165-78. Crossref
12. Schoonheim-Klein M, Muijtjens A, Habets L, Manogue M, van
der Vleuten C, van der Velden U. Who will pass the dental OSCE?
Comparison of the Angoff and the borderline regression standard
setting methods. Eur J Dent Educ. 2009;13:162-71. Crossref
13. Downing SM. Validity: on the meaningful interpretation of
assessment data. Med Educ. 2003;37:830-7. Crossref
14. Axelson RD, Kreiter CD. Rater and occasion impacts on the
reliability of pre-admission assessments. Med Educ. 2009;43:1198-202. Crossref
15. Kane MT, Crooks TJ, Cohen AS. Designing and evaluating
standard-setting procedures for licensure and certification tests.
Adv Heal Sci Educ Theory Pract. 1999;4:195-207. Crossref
16. Kramer A, Muijtjens A, Jansen K, Düsman H, Tan L, van der Vleuten C. Comparison of a rational and an empirical standard
setting procedure for an OSCE. Objective structured clinical
examinations. Med Educ. 2003;37:132-9. Crossref
| Attachment | Size |
|---|---|
| v24n1_Setting.pdf | 486.74 KB |