Long-term Results of Palliative Stereotactic Radiotherapy of Barcelona Clinic Liver Cancer Stage C Hepatitis B–Related Hepatocellular Carcinoma
ORIGINAL ARTICLE CME
Long-term Results of Palliative Stereotactic Radiotherapy of
Barcelona Clinic Liver Cancer Stage C Hepatitis B–Related
Hepatocellular Carcinoma
CKK Choi, CHM Ho, MYP Wong, RWK Leung, FCS Wong, SY Tung, FAS Lee
Department of Clinical Oncology, Tuen Mun Hospital, Hong Kong
Correspondence: Dr CKK Choi, Department of Clinical Oncology, Tuen Mun Hospital, Hong Kong. Email: calvinkkchoi@hkbh.org.hk
Submitted: 17 Jul 2020; Accepted: 8 Mar 2021.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors declare no conflict of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: This study was approved by New Territories West Cluster Research Ethics Committee (Ref NTWC/REC/20040). Informed
consent was obtained from patients for stereotactic body radiotherapy.
Acknowledgements: The authors acknowledge Mr Jia-Jie Huang for his statistical analysis support.
Abstract
Objective
To assess the long-term effectiveness of palliative stereotactic body radiotherapy (SBRT) in patients with
large unresectable Barcelona Clinic Liver Cancer stage C hepatitis B–related hepatocellular carcinomas (HCCs).
Methods
Consecutive HCC cases treated with fractionated SBRT between January 2008 and December 2010 were
analysed. The long-term survival and response rate were evaluated. Univariate and multivariate analyses were
performed to identify the significant predictors of survival.
Results
In total, 32 cases were analysed, with median gross tumour volume was 509.5 cm3 (range, 2.2-3088 cm3).
Median treatment prescription was 32 Gy (range, 20-40 Gy) in five to 10 fractions over 1 to 2 weeks. Median followup
was 13.4 months; median survival was 13.3 months (95% confidence interval [CI]=11.4-15.2). Stable and partial
tumour response rates by RECIST criteria were 69% and 31%, respectively. Alpha-fetoprotein reduction at ≥3 months
after radiotherapy (p = 0.018) and gain in body weight after SBRT (p < 0.001) were significantly associated with
longer survival after multivariate analysis.
Conclusion
SBRT with dose individualisation can be delivered safely to large unresectable tumours in patients with
HBV-related HCC. The median survival after SBRT in this study was 13.3 months. Alpha-fetoprotein reduction at ≥3
months and weight gain after radiotherapy were positive prognostic factors for longer survival. More prospective
studies are warranted to confirm these results.
Key Words: Carcinoma, hepatocellular; Hepatitis B, Radiosurgery
中文摘要
巴塞隆拿肝癌分期系統第3期乙型肝炎相關肝細胞癌患者的紓緩性立體定位放射治療的長期結果
蔡國強、何凱文、黃然柏、梁永堅、黃志成、董煜、李安誠
目的
評估紓緩性立體定位放射治療(SBRT)對巨大無法切除的巴塞隆拿肝癌分期系統第3期乙型肝炎相關肝細胞癌(HCC)患者的長期療效。
方法
分析2008年1月至2010年12月期間接受SBRT分次治療的HCC患者。評估長期存活率和腫瘤緩解率,並以單變量和多變量分析檢視存活期的重要預測因子。
結果
分析SBRT分次治療的HCC患者共32例,中位腫瘤體積509.5 cm3(介乎2.2-3088 cm3)。處方劑量中位數為32 Gy 20-40 Gy /5-10 frs/1-2週。中位隨訪期為13.4個月,中位存活期為13.3個月(95%置信區間:11.4至15.2個月)。根據固體腫瘤反應評估標準(RECIST),腫瘤大小無變化和部分緩解分別為69%和31%。多變量分析顯示患者放療3個月或之後的甲胎蛋白減少(p = 0.018)和SBRT後體重增加(p < 0.001)與較長存活期顯著相關。
結論
對於與乙型肝炎病毒相關的不可切除HCC患者,劑量個體化SBRT是安全的療法。這項研究顯示患者在SBRT後中位存活期為13.3個月。放療後3個月或以上的甲肝蛋白下降,以及放療後體重增加是延長存活期的正向預後因素。需要進行更多前瞻性研究證實以上結果。
INTRODUCTION
Hepatocellular carcinoma (HCC) is the fifth most
common cancer in Hong Kong and sixth most common
cancer worldwide. Eighty-nine percent of HCC cases are
hepatitis B virus (HBV)–related. There were more than
1834 new cases in 2017. It was the third most common
cause of cancer deaths in males in 2017.[1]
In the past, radiotherapy (RT) was seldom used in the
management of HCC because of the high risk of liver
toxicity. Recent studies have shown that stereotactic body
radiotherapy (SBRT) in HCC has high control rates with
low liver toxicities.[2] The Barcelona Clinic Liver Cancer
staging system (BCLC) does not include radiotherapy
as a treatment option. According to the BCLC treatment
algorithm, stage C locally advanced HCC is treated with
sorafenib.[3] With the advances in radiotherapy planning
and delivery,[4] SBRT has been shown to be a safe and
effective treatment for unresectable HCC.[5] [6] [7] The National
Comprehensive Cancer Network Guidelines for HCC
recommends RT as a locoregional therapy option.[8]
To the best of our knowledge, there is limited literature
evaluating the role of SBRT in BCLC stage C HBV-related
HCC. In our previous paper,[7] we reported
radiotherapy details, short-term response, safety, and toxicity of palliative SBRT in 36 patients with HBV-related
HCC. In the present study, we investigated the
long-term efficacy of palliative SBRT for HBV-related
HCC, as well as prognostic factors.
METHODS
Patients
The data of consecutive patients with HBV-related
BCLC stage C HCC, Child’s grade A to B8 without
distant metastases treated with SBRT from 2008 to 2010
were retrieved retrospectively from hospital records in
2015. Eligibility criteria are described in our previous
paper studying the impact of SBRT on liver function,
with stages other than BCLC stage C excluded.[7]
Radiotherapy Treatment
Patients were prescribed 4 Gy per fraction to the planning
target volume for five to 10 fractions.[7]
Statistical Analysis
The data were analysed using SPSS (Windows version
23.0; IBM Corp., Armonk [NY], United States). Kaplan–Meier testing was used for univariate overall survival
(OS) analysis with p < 0.05 considered significant.
Cox regression was used for those variables that were
significant in the univariate OS analysis.
RESULTS
Cases
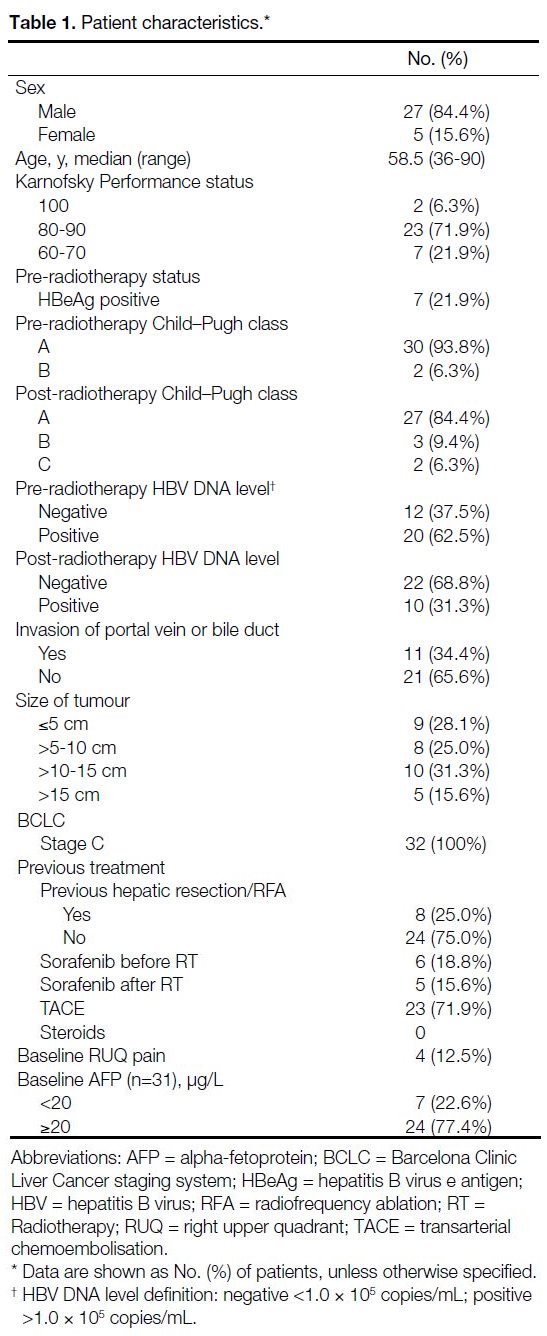
Between January 2008 and December 2010,
32 consecutive patients with BCLC stage C unresectable
HCC underwent SBRT at our institution (Table 1). These patients had large unresectable tumours, with
median gross tumour volume (GTV) 509.5 cm3
(range, 2.2-3088 cm3). The tumour size was >10 cm in
15 (46.9%) patients and >15 cm in five (15.6%) patients.
The median age was 58.5 years (range, 36-90 years).
The majority (25 [78.1%]) of patients had a Karnofsky
Performance status ≥80. In 2015, 30 patients were dead.
Of the surviving two patients, one patient was alive for
5.9 years since treatment and censored on 12 October
2015 when data were collected. The other patient was
lost to follow-up and censored on 26 March 2010,
1.5 years after treatment.
Table 1. Patient characteristics.
Treatment
All 32 patients received 4 Gy per fraction with a median
total prescription dose of 32 Gy (range, 20-40 Gy). Prior
treatments included surgical resection or radiofrequency
ablation in eight (25%) patients, and transarterial
chemoembolisation (TACE) in 23 (71.9%) patients.
Sorafenib was administered to six (18.8%) patients before
SBRT and five (15.6%) patients after SBRT. No patient
received steroid therapy. Details of the radiotherapy can
be found in our previous study.[7]
Symptom Control
Pain
The most common presenting symptoms were right
upper quadrant pain and distension. After 3 to 4 weeks
of radiotherapy, up to 90% of patients had significant
pain relief.
Body Weight
Weight loss was defined as a decrease in body weight
of ≥10% within the 3 months before treatment. In total,
12 (37.5%) of the 32 cases had increased body weight
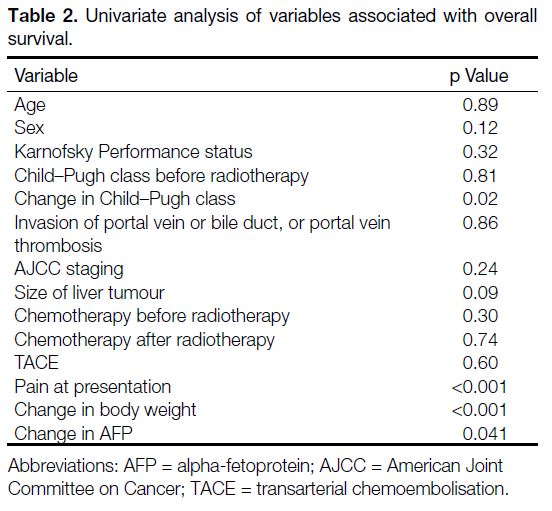
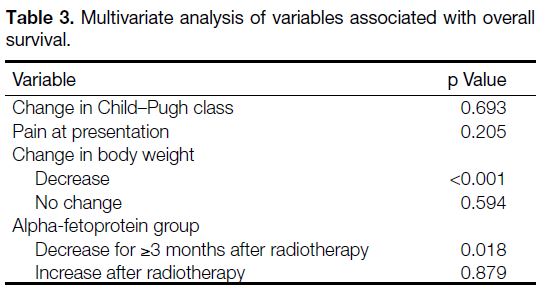
1 month after radiotherapy; univariate and multivariate
analysis showed that this was significantly associated
with longer survival (p < 0.001 and p < 0.001) [Tables 2 and 3]. In all, 11 (34.4%) patients had unchanged body
weight after radiotherapy and nine (28.1%) patients
experienced weight loss. Univariate and multivariate
analysis showed that patients with weight loss were
observed to have shorter survival (p < 0.001 and
p < 0.001) [Tables 2 and 3].
Table 2. Univariate analysis of variables associated with overall survival.
Table 3. Multivariate analysis of variables associated with overall survival.
Changes in Alpha-Fetoprotein after
Radiotherapy
Only 31 patients were evaluated for change of alpha-fetoprotein
(AFP) levels after radiotherapy because of
missing data for one patient. In total, 24 of 31 patients
(77.4%) had elevated AFP level (>20 μg/L) at the time of treatment planning. Seven (22.6%) patients had
reduction of AFP level that persisted for ≥3 months after
radiotherapy. Seven (22.6%) patients had increased AFP
level after radiotherapy, and 17 patients had decreased or
static AFP level within 3 months after radiotherapy. In
the seven patients with reduction of AFP level, median
survival was 640 days (range, 398-2190 days). Univariate
and multivariate analysis showed that reduced AFP
level was significantly associated with longer survival
(p = 0.041 and p = 0.018) [Tables 2 and 3]. In the seven
patients with increased AFP levels after radiotherapy,
median survival was 210 days (range, 101-1277 days).
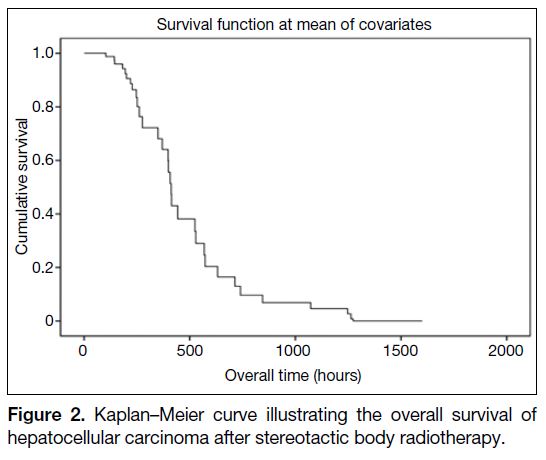
Response and Survival
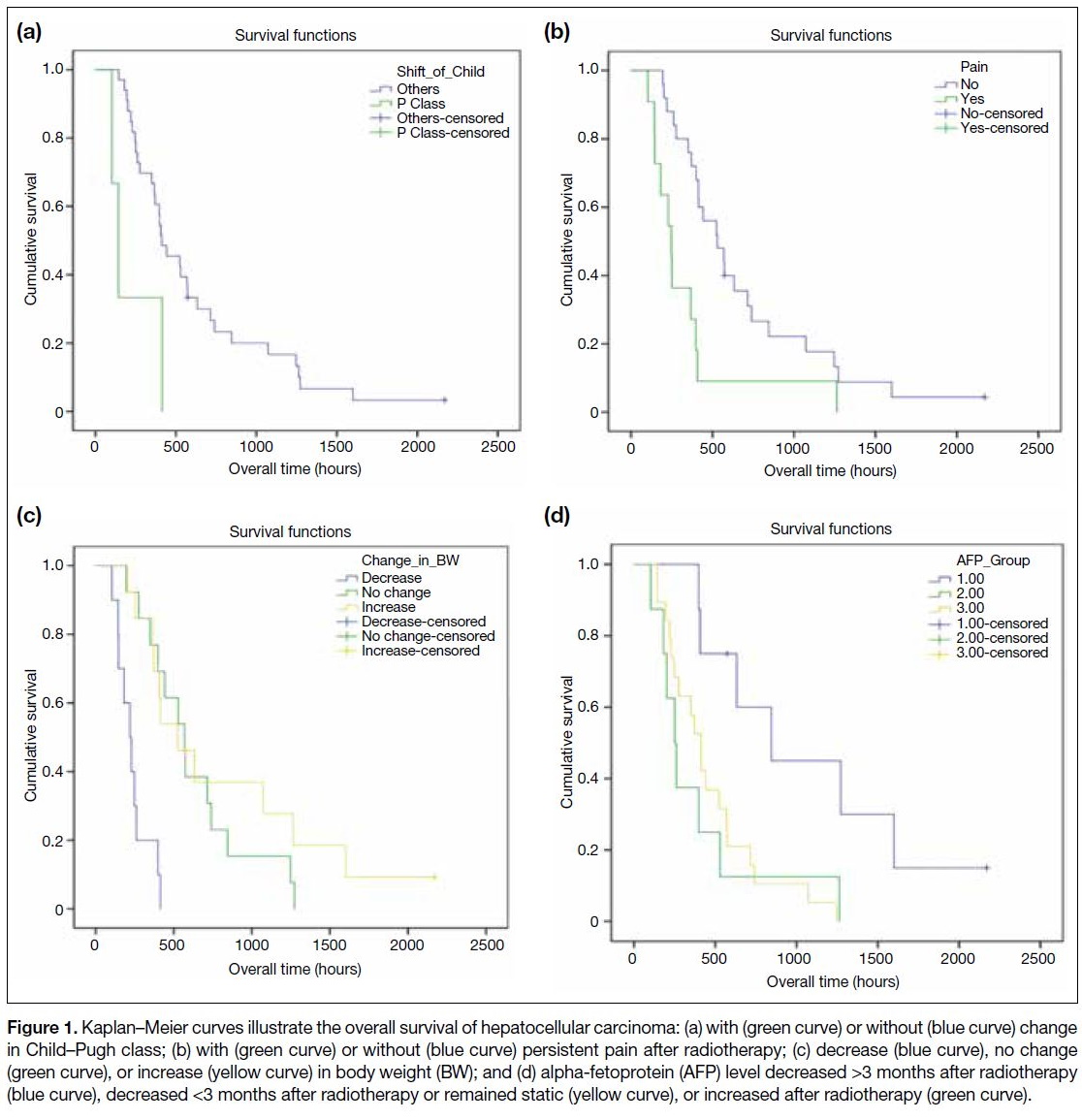
The median survival of all 32 patients was 13.3 months
(95% confidence interval [CI]=11.4 -15.2) The 1-year
and 3-year survival was 62.5% (95% CI=53.9%-71.1%)
and 14.1% (95% CI=7.74%-20.5%), respectively. Figure 1 shows the Kaplan–Meier curves illustrating factors affecting the OS. Figure 2 shows Kaplan–Meier
curves illustrating OS of patients with HCC after SBRT.
Figure 1. Kaplan–Meier curves illustrate the overall survival of hepatocellular carcinoma: (a) with (green curve) or without (blue curve) change
in Child–Pugh class; (b) with (green curve) or without (blue curve) persistent pain after radiotherapy; (c) decrease (blue curve), no change
(green curve), or increase (yellow curve) in body weight (BW); and (d) alpha-fetoprotein (AFP) level decreased >3 months after radiotherapy
(blue curve), decreased <3 months after radiotherapy or remained static (yellow curve), or increased after radiotherapy (green curve).
Figure 2. Kaplan–Meier curve illustrating the overall survival of
hepatocellular carcinoma after stereotactic body radiotherapy.
DISCUSSION
In Hong Kong, HBV-related HCC is clinically different
to hepatitis C–related HCC in Western populations.
It is relatively larger in size and some of the tumours
are encapsulated. In terms of efficacy, we previously
demonstrated the response to and efficacy of moderate
doses of hypofractionated SBRT for patients with
unresectable HCC.[7] Most patients had significant
pain relief after radiotherapy. In the present study, we
investigated the long-term efficacy of palliative SBRT
for HBV-related HCC.
With a median follow-up of 13.4 months, no patients
developed progressive disease within 3 months after
radiotherapy. The tumour response rate by mRECIST
criteria was 69%. The median survival was 13.3 months.
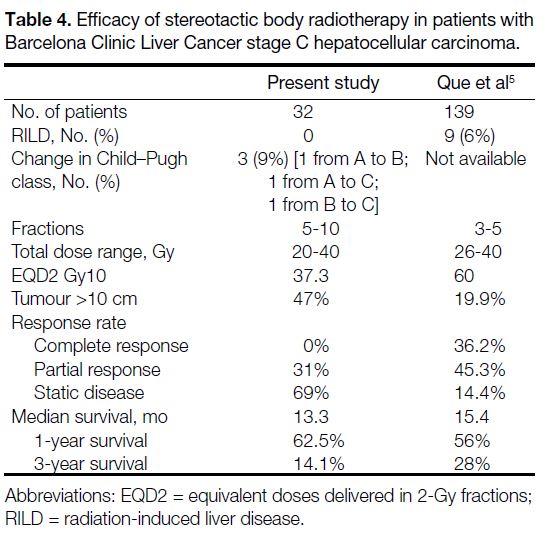
Que et al[5] published the treatment results of SBRT in
patients with BCLC stage C HCC. Their series found
the overall RECIST response rate was 81.5% (complete
response, 36.2%; partial response, 45.3%), with a stable
disease rate of 14.4%. Their median dose was 40 Gy in
three to five fractions (range, 39-40 Gy). In the current
study, the tumour size was much larger and the equivalent
doses delivered in 2-Gy fractions (EQD2) Gy10 were
lower than those in Que et al’s study (37.3 Gy10 vs 60
Gy10)[5] [Table 4]. Thus, the higher response rate in Que
et al’s study may have been due to the smaller size of
tumours as well as the higher radiation dose.[5]
Table 4. Efficacy of stereotactic body radiotherapy in patients with Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma.
The 1-year OS was 62.5%, and 3-year OS was 14.1%.
The 1-year and 3-year OS rates in Que et al’s series
were 56% and 28%, respectively.[5] The survival rates are
comparable. Que et al’s response rate was much higher
than that in our study.[5] Again, it may be due to the tumour
size, which was much smaller than that in our study
cases, or higher radiation dose. In univariate analysis, the
present study showed that change in Child–Pugh class,
pain at presentation, change in body weight, and change
in AFP were significantly related to OS. TACE before
RT was not significant but there was a trend to improve
OS. In multivariate analysis, only change in body weight
and decrease in AFP were significantly associated with
OS.
This is the first study to show that patients with large
unresectable HCCs can benefit from a small palliative dose. We found a significant survival benefit. It is
worthwhile to administer palliative radiotherapy to
large HBV-related liver tumours. An individualised
dose prescription is safe up to a ceiling dose of 40 Gy
in 10 fractions in accordance with dose constraints to
uninvolved liver (V30 <40% and mean dose <28 Gy)
and uninvolved liver volume >700 cm3 in a relatively
large liver tumour (median GTV 509.5 cm3; range 2.2-3088 cm3).
CONCLUSION
Palliative SBRT with individualised dose up to 40 Gy in
10 fractions can be delivered safely to large unresectable
HBV-related HCCs. The median survival rate of patients
with BCLC stage C HCC in this study was 13.3 months.
AFP reduction at ≥3 months and body weight gain after
radiotherapy were positive prognostic factors. More
prospective studies are warranted to confirm these
results.
REFERENCES
1. Hospital Authority, Hong Kong SAR Government. Hong Kong Cancer Registry. 2019. Available from: https://www3.ha.org.hk/
cancereg/. Accessed 1 Feb 2021.
2. Baumann BC, Wei J, Plastaras JP, Lukens JN, Damjanov N,
Hoteit M, et al. Stereotactic body radiation therapy (SBRT) for
hepatocellular carcinoma high rate of local control with low
toxicity. Am J Clin Oncol. 2018;41:1118-24. Crossref
3. Richani M, Kolly P, Knoepfli M, Herrmann E, Zweifel M, von
Tengg-Kobligk H, et al. Treatment allocation in hepatocellular
carcinoma: Assessment of BCLC algorithm. Ann Hepatol.
2016;15:82-90. Crossref
4. Meyer J, Singal AG. Stereotactic ablative radiotherapy for hepatocellular carcinoma: history, current status and opportunities.
Liver Transpl 2018;24:420-7. Crossref
5. Que J, Lin CH, Lin LC, Ho CH. Challenges of BCLC stage C hepatocellular carcinoma: Results of a single-institutional
experience on stereotactic body radiation therapy. Medicine
(Baltimore). 2020;99:e21561. Crossref
6. Chopra S, George K, Engineer R, Rajamanickam K, Nojin S,
Joshi K, et al. Stereotactic body radio therapy for inoperable large
hepatocellular cancers: results from a clinical audit. Br J Radiol.
2019;92:20181053. Crossref
7. Choi CK, Lee FA, Lam TC, Wong FC, Wong VY, Lui C, et al.
Impact of fractionated stereotactic body radiotherapy on liver
function in patients with hepatitis B virus-related hepatocellular
carcinoma: clinical and dosimetric analysis. Hong Kong J Radiol.
2013;16:94-9. Crossref
8. Wahl DR, Stenmark MH, Tao Y, Pollom EL, Caoili EM,
Lawrence TS, et al. Outcomes after stereotactic body radiotherapy
or radiofrequency ablation for HCC. J Clin Oncol. 2016;34:452-9. Crossref