Radiation Dose Reduction for Endoscopic Retrograde Cholangiopancreatography: An Initiative for Patient and Endoscopist Radiation Safety
ORIGINAL ARTICLE
Radiation Dose Reduction for Endoscopic Retrograde
Cholangiopancreatography: An Initiative for Patient and
Endoscopist Radiation Safety
KY Man, KH Lui, KY Cho
Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong
Correspondence: Dr KY Man, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong. Email: dsgundam@hotmail.com
Submitted: 16 Jan 2018; Accepted: 24 Aug 2018.
Contributors: KYM designed the study. KYM and KHL acquired the data. KYM analysed the data and drafted the manuscript. All authors
critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the
final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Hong Kong East Cluster Research Ethics Committee (Ref HKECREC-2017-061). The patients
were treated in accordance with the tenets of the Declaration of Helsinki. The patients provided written informed consent for all treatments and
procedures.
Abstract
Objectives
To evaluate the effectiveness of a practical dose reduction measure for endoscopic retrograde
cholangiopancreatography (ERCP) and to ensure the radiation dose is maintained in line with well-established
international reference levels.
Methods
Between January 2017 and July 2017, 50 ERCP examinations were retrospectively evaluated to estimate
the patient radiation doses received while undergoing ERCP examinations in a tertiary referral centre in Hong Kong
before and after implementation of radiation dose reduction measures by adjusting the acquisition parameters on the
fluoroscopy machine in the designated fluoroscopic suite. Statistical analysis was performed on dose area product.
We also assessed the fluoroscopy time, the number of spot images taken during the examination, the quality of the
diagnostic radiographic images, and the outcome of the ERCP (including technical success rate and complications).
Results
A significant reduction (53.4%) in dose area product was achieved at the end of the study. The fluoroscopy
time, the number of spot images taken, the quality of the diagnostic radiographic images, and the outcome of ERCP
before and after implementation of dose reduction measures did not show any significant differences.
Conclusion
A significant reduction in radiation dose to patients undergoing ERCP was achieved after implementation
of a simple practical dose reduction measure in our hospital, without lengthening fluoroscopy time, or compromising
image quality or outcome.
Key Words: Cholangiopancreatography, endoscopic retrograde; Fluoroscopy; Radiation exposure; Radiometry
中文摘要
降低內窺鏡逆行胰膽管造影術的放射劑量:關於患者和內窺鏡醫師放射
安全的一個倡議措施
文家潤、呂錦浩、曹君彥
目的
評估內窺鏡逆行胰膽管造影(ERCP)的實際劑量減少措施的有效性,並確保輻射劑量與公認的國際參考水平保持一致。
方法
於2017年1月至2017年7月期間,在香港三級轉診中心進行ERCP檢查時通過調整指定透視套房內透視機上的採集參數,對50次ERCP檢查進行回顧 性評估,以估計在實施減少輻射劑量措施前後患者接受的輻射劑量。對劑量面積乘積進行統計分析。我們同時評估透視時間、檢查期間拍攝的點圖像數量、診斷性放射圖像質量,以及ERCP結果(包括技術成功率和併發症)。
結果
在研究結束時實現了劑量面積乘積的顯著減少(53.4%)。實施劑量減少措施前後的ERCP在透視時間、拍攝的點片圖像數量,以及診斷性放射圖像質量均沒有顯示出任何顯著差異。
結論
在我們醫院實施簡單實用的劑量降低措施後,接受ERCP的患者的輻射劑量顯著降低,而不延長透視時間也不影響圖像質量或結果。
INTRODUCTION
Ionising radiation is sometimes used during endoscopic
procedures, most frequently during endoscopic
retrograde cholangiopancreatography (ERCP). With
increasing public awareness and concern surrounding
radiation risks, it is crucial that procedures be performed
according to the “as low as reasonably achievable”
(ALARA) principle.
Several previous studies have proposed dose reduction
measures during ERCP by adding protective lead
shields or drapes,[1] [2] [3] but this may involve additional
manipulation of patients or changes in equipment
positioning. For example, when the shield is used,
exposure of endoscopists to radiation was reduced to
17% for diagnostic procedures and to <7% for therapeutic
procedures.[1] However, the shield may interfere with the
manipulation of catheters and wires or affect fluoroscopic
or videoendoscopic visualisation during the procedure.
We aimed to evaluate the effectiveness of a dose
reduction technique involving the adjustment of
acquisition parameters on the fluoroscopy machine. We
also aimed to determine if this adjustment affected the
length of fluoroscopy due to decreased image quality.
METHODS
To formulate a dose reduction goal, a national dose
survey was used as a reference.[4] The means of dose area products (DAPs) for diagnostic and therapeutic ERCPs
are 4 and 10 Gycm2, respectively. The mean fluoroscopy
times for diagnostic and therapeutic ERCP are 2.6 and
4.4 minutes, respectively.
Study Design
A retrospective review of radiation doses received by
patients undergoing ERCP examinations from January
2017 to July 2017 in a local tertiary referral centre was
performed, before (standard dose) and after (low dose)
implementation of radiation dose reduction measures.
Two phases of the study have been conducted. The first
phase consisted of an audit of radiation dose for ERCP
from January to May 2017 (standard dose). These data
were used as a baseline reference representing normal
practices before implementation of dose reduction
measures. Endoscopists were not aware that the study
was being undertaken. After implementation of radiation
dose reduction measures, an audit of the low-dose
cohort from May 2017 to July 2017 was performed.
Radiological and clinical records of ERCP performed in
these periods were retrospectively reviewed.
The major outcomes were radiation dose, ERCP outcome,
and image quality. Data including patient demographics,
DAP (Gycm2), fluoroscopy time (min), number of spot
images taken during examinations, procedure indication,
difficulty, complications, technical success, and image
quality were collected.
The radiation doses were recorded from the fluoroscopic
machine display. The clinical variables related to the
ERCP were retrieved through dedicated electronic
patient records in our institution. Two independent
radiologists assessed the image quality.
Study Population
Adult patients (aged >18 years) who underwent ERCP
were included. The patients were referred from various
departments within the hospital. All ERCPs were
clinically indicated.
To estimate the sample size, we performed an a priori
sample size estimation with the G-Power 3.1.0 (power:
0.8; α: 0.05) by using data from a previous study that
examined radiation dose reduction during ERCP,[3] with a
calculated effect size of 1 (Cohen’s d). It was estimated
that at least 18 subjects in each group would be sufficient.
From January 2017 to May 2017 and May 2017 to July
2017, records of 25 consecutive patients who underwent
ERCP for the standard and 25 consecutive patients for
the low-dose ERCP examination groups were reviewed.
Fluoroscopic Examinations and Acquisition
Parameters
All examinations were performed in our fluoroscopic
suite (Artis zee multi-purpose system; Siemens,
München, Germany).
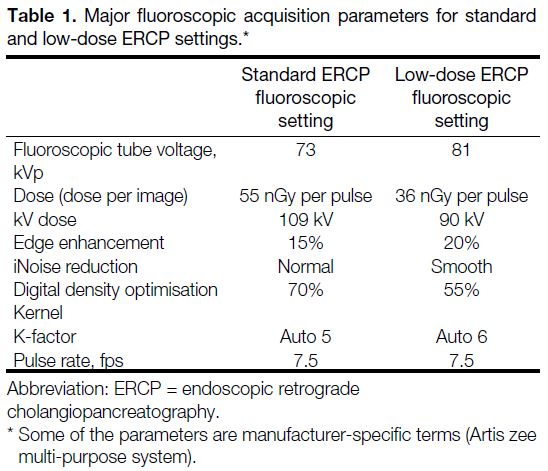
Table 1 shows the detailed acquisition parameters before
and after dose reduction for ERCP. Parameters were
adjusted based on two aspects: dose reduction and image
quality. It is generally thought that the image quality may be compromised in a low-dose setting; we aimed to
compensate for this effect.
Table 1. Major fluoroscopic acquisition parameters for standard and low-dose ERCP settings.
The changes were discussed with the manufacturer and
application specialists. In order to achieve ALARA, it
seemed unnecessary to use the relatively high-dose
settings currently in use to achieve an adequate image
quality for biliary tree evaluation. The proposed changes
to the protocol to reduce the dose were discussed and
agreed by an expert panel in the Working Group on
Radiation Safety in our institution. The local Institutional
Review Board approved this study.
The endoscopists, including hepatobiliary team surgeons
and gastrointestinal physicians, performed approximately
1000 ERCP procedures in the year prior to the study at
our institution. All endoscopists were unaware that the
study, with changes to protocol parameters, was being
undertaken.
Among the available metrics for radiation exposure,
DAP was appropriate for monitoring patient radiation
dose.[5] DAP is defined as the absorbed dose multiplied
by the X-ray beam cross-sectional area at the point of
measurement. Our fluoroscopic machine was equipped
with a DAP meter. The DAP was shown on the live
screen in the examination room, on the data display in
the examination room, and on the console monitor in the
control room. The DAP meter was calibrated at regular
intervals.
Procedure Indication, Intent, and Difficulty
Although related, procedure indication and intent were
distinct issues. The indication related to the reason for
the procedure. The intent was the goal for a specific
procedure. For example, an ERCP might be indicated in
a patient with obstructive jaundice, whereas the intent
could be either to find the cause of jaundice (diagnostic)
or to relieve the jaundice (therapeutic). It was necessary
to assess indication and intent because both were integral
components of determining procedure success.
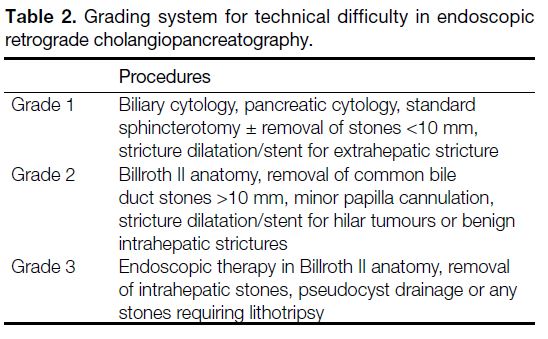
ERCP difficulty was determined by a published grading
system that was developed for the assessment of ERCP
outcomes.[6] All ERCPs are classified into three levels
based on the technical difficulty of each manoeuvre
(Table 2). This classification provides a simple and
objective measure of the clinical complexity of an ERCP
and may also provide a measure of procedure risk. The
difficulty of a procedure was also important for assessing
procedure success.
Table 2. Grading system for technical difficulty in endoscopic retrograde cholangiopancreatography.
Complications and Technical Success
The specific method of identifying and collecting
unplanned events/complications remains controversial
for ERCP.[6] Complications such as pancreatitis or
perforation are obvious and should be tracked. The
significance of other events associated with the procedure
remains unclear. Further research is required before the
optimal method to record delayed complications can be
firmly established. Nevertheless, unplanned events were
tracked in our study.
Technical success was based on the technical difficulty
of ERCP. Thus, technical success was stratified based on
technique and described as complete success (diagnostic
and therapeutic), partial success (access to desired duct
with incomplete or partial therapy) or failed (failure to
access or drain the desired duct). For example, a simple
cannulation was not sufficient to represent success in
cases where basic therapeutic measures were necessary.
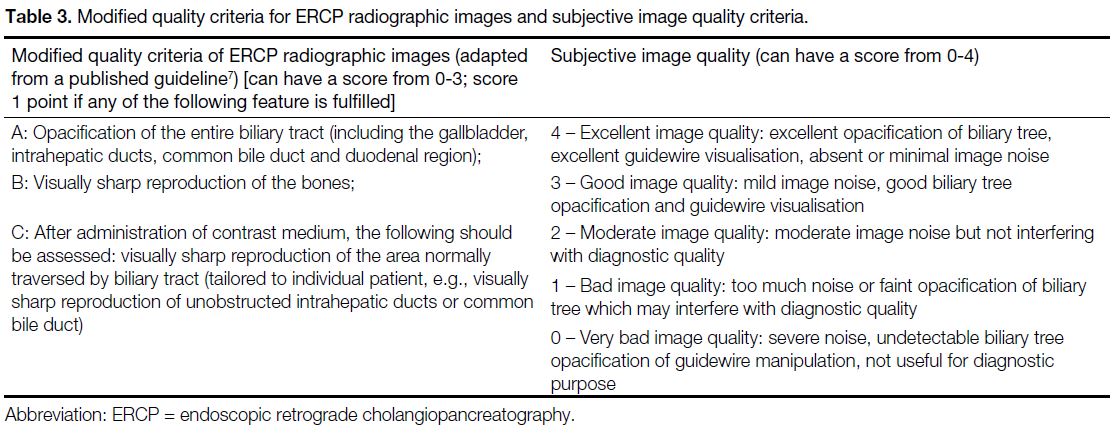
Image Quality Evaluation
To the best of our knowledge, there are no objective
quality criteria for ERCP radiographic images to date. In
order to better assess the quality of ERCP radiographic
images, we adopted the quality criteria for urinary tract
radiographic images before and after administration of
contrast medium according to a published guideline,[7]
with some modifications for the biliary tract (Table 3).
Subjective evaluation of image quality was also
performed using a scoring system, with particular
attention to image contrast and noise, ranking from 0 to
4 (Table 3).
Table 3. Modified quality criteria for ERCP radiographic images and subjective image quality criteria.
Two independent radiologists were aware of the clinical
information and assessed the image quality of the spot
ERCP radiographic images of different patients in
randomised order. They were blinded to each other’s
results and the parameters used to acquire the images
(both the low-dose and standard-dose protocols). They
were asked to record the image quality score according
to the above proposed criteria. All images were
reviewed on a dedicated workstation (Carestream PACS
Workstation, Carestream, Genova, Italy).
Statistical Analysis
Statistical analysis was performed with commercially
available statistical software SPSS (Windows version
22.0; IBM Corp, Armonk [NY], United States).
Comparison of demographics, radiation dose, ERCP
outcome, and image quality were done with t test, Mann-Whitney U test, or Chi-square test as appropriate.
Standard multiple regression was used to identify
any possible predictors/confounding factors for DAP. Relevant variables known to have an association with
DAP were included in the model. Age, body mass index
(BMI), fluoroscopy time, number of spot images taken,
and ERCP difficulty grade were added into the regression
model as predictors. A general linear model was
performed to mitigate any potential confounding effects
of the confounders on DAP. Statistical significance for
all of the tests was set at p < 0.05.
Inter-observer agreement of the image quality scores
were assessed using the kappa statistic. The κ strengths
were categorised as follows: <0.20, poor; 0.21 to 0.40,
fair; 0.41 to 0.60, moderate; 0.61 to 0.80, good; and 0.81
to 1.00, very good.
RESULTS
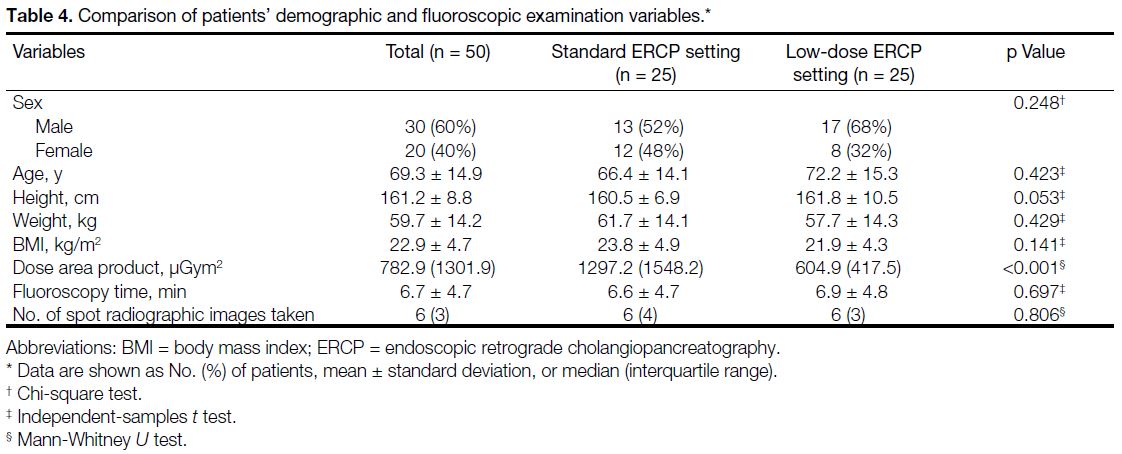
Radiation Dose Reduction
The median DAP was 13.0 Gycm2 for standard ERCP
settings and 6.1 Gycm2 for low-dose ERCP settings.
The difference in median DAP between the two groups
was statistically significant (Mann-Whitney U test,
p < 0.001). The median DAP for the low-dose
examination was 53.4% lower than the standard-dose
examination (Table 4).
Table 4. Comparison of patients’ demographic and fluoroscopic examination variables.
There were no statistically significant differences in age,
gender, height, weight, or BMI between the two groups
(Chi-square test or t test, p > 0.05). There were also no
statistically significant differences in fluoroscopy time
and number of spot images taken between the two groups
(t test and Mann-Whitney U test, respectively; Table 4).
In the regression model with DAP as the dependent
variable (adjusted R square = 0.561, p < 0.001), BMI (standardised beta = 0.233, p = 0.031), number of spot
images taken (standardised beta = 0.334, p = 0.004), and
fluoroscopy time (standardised beta = 0.481, p < 0.001)
made statistically significant contributions to the
prediction of the dependent variable.
A general linear model was conducted to further explore
differences in DAP between the two groups while
controlling for possible covariates/confounders. BMI,
number of spot images taken, and fluoroscopy time were
used as covariates in the analysis of DAP. After adjusting
for the above-named covariates/confounders, there was
a statistically significant difference in DAP between the
two groups (adjusted R squared = 0.652, p < 0.001).
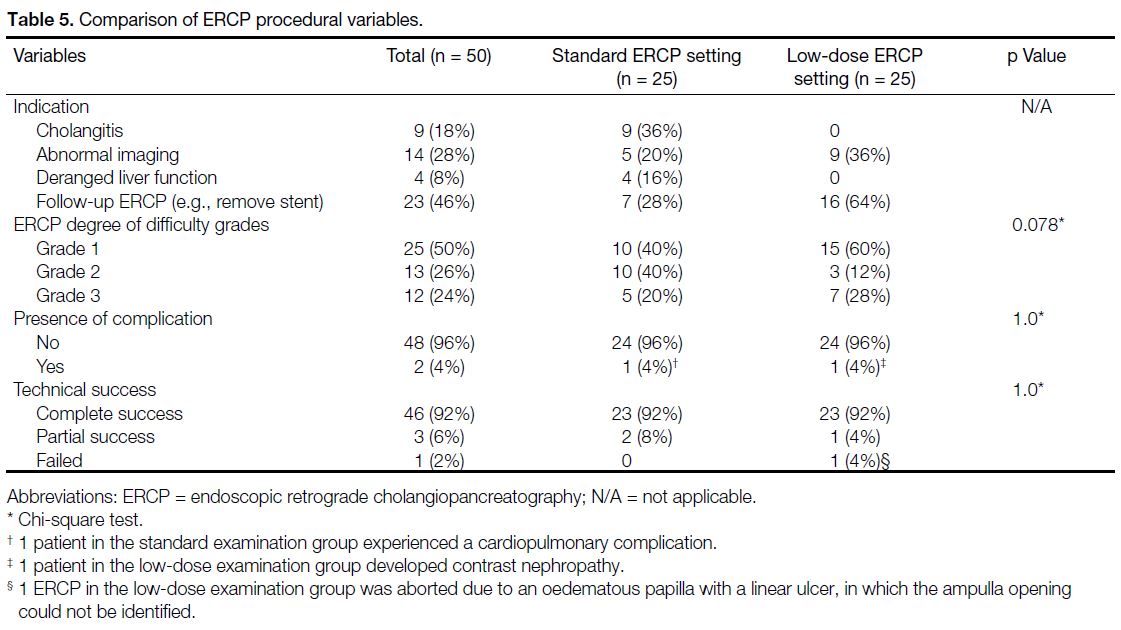
Endoscopic Retrograde Cholangiopancreatography Procedural Variables
All ERCPs were performed for therapeutic purposes.
Nearly half of the ERCPs were performed for follow-up
(e.g., after removal of a stent). There were no statistically
significant differences in ERCP degree of difficulty,
complication rate, or technical success rate between the
standard and low-dose examination groups (Chi-square
test, p > 0.05) [Table 5]. Median follow-up time for post-ERCP complication was 3 months (range, 2-6 months).
For patients with complications following ERCP, none
of them was definitely attributed to the low-dose
setting.
Table 5. Comparison of ERCP procedural variables.
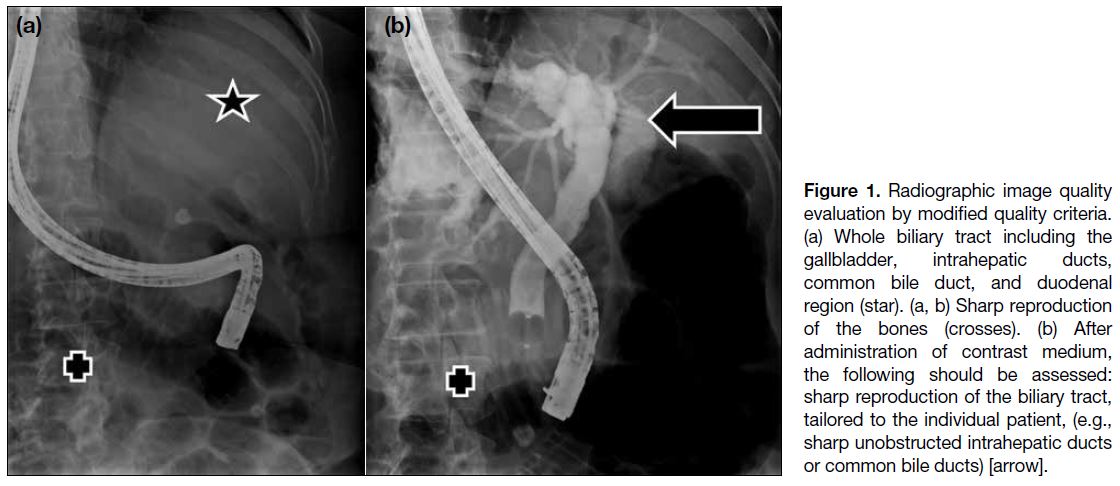
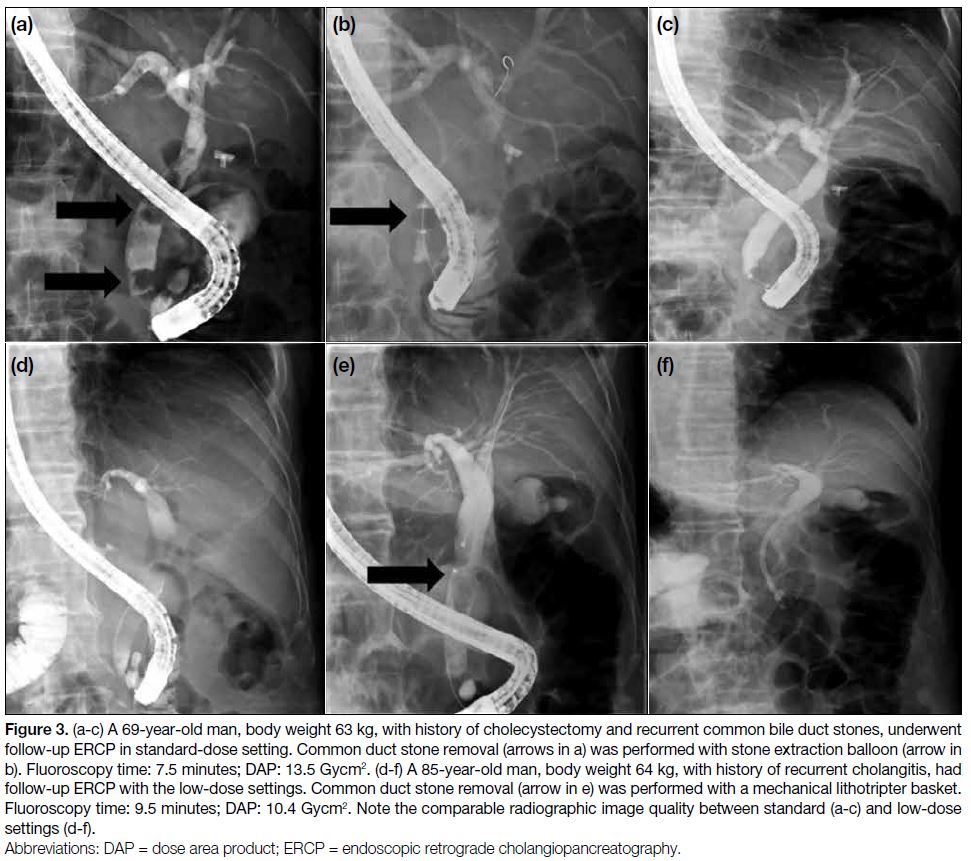
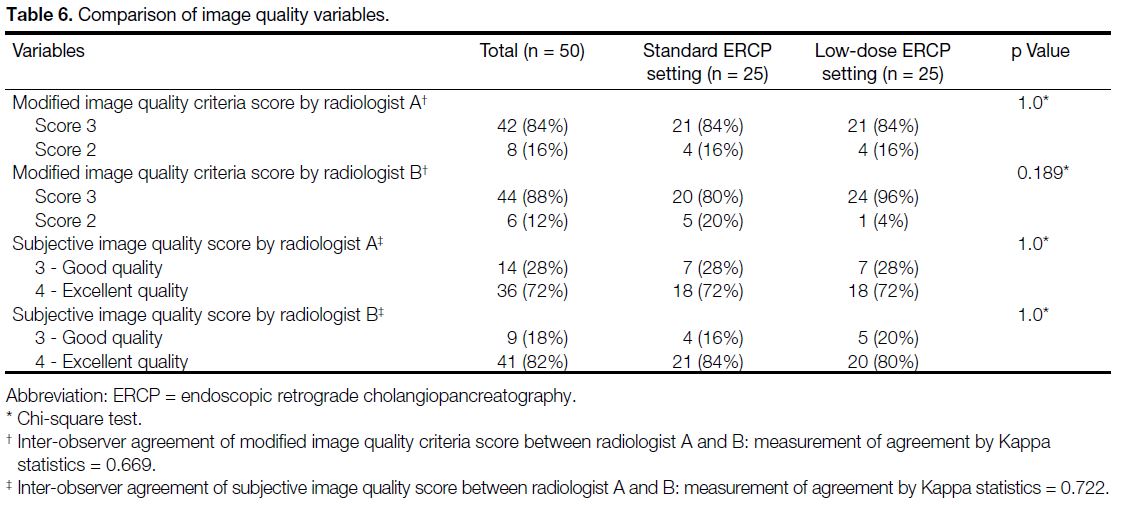
Image Quality Evaluation
Radiographic and subjective image quality evaluation
(Figures 1 2 3) by the two independent radiologists
showed no significant difference in the scores among the two patient groups (Chi-square test, p > 0.05). The inter-observer
agreement on modified image quality criteria
and subjective image quality were good (kappa = 0.669
and 0.722, respectively) [Table 6].
Figure 1. Radiographic image quality evaluation by modified quality criteria. (a) Whole biliary tract including the gallbladder, intrahepatic ducts, common bile duct, and duodenal region (star). (a, b) Sharp reproduction of the bones (crosses). (b) After administration of contrast medium, the following should be assessed: sharp reproduction of the biliary tract, tailored to the individual patient, (e.g., sharp unobstructed intrahepatic ducts or common bile ducts) [arrow].
Figure 2. Subjective image quality evaluation. Excellent image
quality: excellent opacification of biliary tree, excellent guidewire
visualisation, absent or minimal image noise.
Figure 3. (a-c) A 69-year-old man, body weight 63 kg, with history of cholecystectomy and recurrent common bile duct stones, underwent
follow-up ERCP in standard-dose setting. Common duct stone removal (arrows in a) was performed with stone extraction balloon (arrow in
b). Fluoroscopy time: 7.5 minutes; DAP: 13.5 Gycm2. (d-f) A 85-year-old man, body weight 64 kg, with history of recurrent cholangitis, had
follow-up ERCP with the low-dose settings. Common duct stone removal (arrow in e) was performed with a mechanical lithotripter basket.
Fluoroscopy time: 9.5 minutes; DAP: 10.4 Gycm2. Note the comparable radiographic image quality between standard (a-c) and low-dose
settings (d-f).
Table 6. Comparison of image quality variables.
DISCUSSION
The two basic principles of radiation protection of
the patient as recommended by the International
Commission on Radiological Protection are justification of practice and optimisation of protection, including the
consideration of dose reference levels. Justification is
the first step in radiation protection. It is accepted that
no diagnostic exposure is justifiable without a valid
clinical indication, no matter how good the imaging
performance may be. Every examination must result in
a net benefit for the patient. This only applies when it
can be anticipated that the examination will influence the
clinical decision with respect to the following: diagnosis, patient management and therapy, and final outcome for
the patient.
With respect to diagnostic examinations, the
International Commission on Radiological Protection
does not recommend the application of dose limits to
patient irradiation but draws attention to the use of dose
reference levels as an aid to optimisation of protection
in medical exposure. Once a diagnostic examination
has been clinically justified, the subsequent imaging
process must be optimised. The optimal use of ionising
radiation involves the interplay of three important
aspects of the imaging process: the diagnostic quality of
the radiographic image, the radiation dose to the patient,
and the choice of radiographic technique.
Radiation dose to patients during ERCP depends on many
factors.[5] Some factors are related to the endoscopist,
including fluoroscopy time, number of digital spot
images taken, and use of collimation. The endoscopist
cannot control some variables, such as patient size or
procedure type (diagnostic vs. interventional). Other
factors are intrinsic to the equipment. For instance,
pulsed fluoroscopy, whereby the X-ray beam is turned on
and off at a fixed rate, can significantly reduce exposure
without having the X-ray beam on continuously[8]; copper
X-ray beam filtration, which limits patient dose from low-energy X-rays; fluoroscopic loop review, and last-image
hold options that allow review of images without
additional X-ray exposure. There is often a trade-off
between image quality and radiation exposure. For
example, choosing a low dose may result in a noisy
image, especially for an obese patient, so for such
patients, the endoscopist will often choose a medium- or
high-dose setting.
In our study, radiation and image acquisition parameters
were adjusted. For radiation parameters, the fluoroscopic
tube voltage was increased from 73 kVp to 81 kVp.
The fluoroscopic tube voltage in kV was maintained
automatically for as long as possible. For extremely thin
or small patients, the kV value was reduced. In case of
lower transparency (thicker objects), the kV value would
be increased to ensure correct image brightness. It was
recommended by the manufacturer to set the X-ray tube
voltage as high as possible (not forgetting the image
quality and image contrast). It is reported that a high kV
technique (80-100 kV) could reduce the dose to a patient
up to 50%, compared to the conventional technique
(75-96 kV).[8] The dose in the scanning protocol
parameters refers to dose per spot image. It was a nominal
value which applied to the measuring conditions at
70 kV, 2.1-mm Cu pre-filtering, 16-cm flat detector
input field. It was decreased from 55 nGy per pulse to
36 nGy per pulse, which decreased the dose from every
single fluoroscopic image. According to manufacturer
instructions, ‘kV dose’ was the value at which the dose
was switched over for dose reduction. Dose reduction
would be performed at a preselected kV.
For image parameters, edge enhancement was increased
from 15% to 20%. It resulted in a clearer display of
contrast differences (e.g., outline of biliary tree).
However, this also caused more noise. The iNoise
reduction setting (Artis zee multi-purpose system)
compensated for increased noise. If the dose is reduced,
additional noise will be perceived as poor image quality.
To compensate for the increased image noise, the
acquisition program can be configured to adjust the
edge enhancement value. DDO-Kernel refers to digital
density optimisation Kernel. DDO (harmonisation)
reduces the dynamic range of an image (bright areas are
less bright, dark areas are less dark). By reducing the
dynamic range, this allowed us to increase the contrast
without saturation of the image in bright or dark areas.
According to manufacturer instructions, K-factor was
based on averaging over time. Reduction of image
noise could be achieved by weighted averaging by the factor √(2k-1). However, noise reduction by averaging
may result in reduced contrast and ‘ghost images’ of
fast-moving objects. The K-factor influences the noise
impression of the image. A high K-factor means less, and
a low K-factor, more image noise. If high K-factors were
used, lag effects (in which the image becomes blurred
due to patient’s movement) appeared in the image.
The fluoroscopic machine uses various copper filters.
These filter out the low-energy components of the X-ray
spectrum that are not needed to create the image. This
causes hardening of the beam, reducing not only the skin
dose to the patient but also the scattered radiation to not
only endoscopist, but also other staff in the room. The
copper filters were from 0.2 to 0.6 mm thickness in our
setting.
A reduced pulse rate would help reduce the radiation
load on the patient and other personnel, but it would
require endoscopists’ adjustment. It was kept constant at
7.5 fps in our study. Perhaps the most readily reliable
method of reducing radiation exposure is the reduction
of the fluoroscopy time. However, a very complex
combination of patient-, endoscopist-, and procedure-related
factors contribute to determine the final
fluoroscopy time.
Several limitations have to be addressed in this study.
First, there are no well-validated objective quality criteria
for ERCP radiographic images, rendering the assessment
of image quality not standardised. The proposed
modified quality criteria adopted from European
guidelines[6] may not necessarily be truly representative
of objective image quality. Further study is warranted to
establish quality criteria for ERCP radiographic images
so that the diagnostic quality can be better assessed
under a standardised approach. Second, the use of a
dedicated fluoroscopic machine (Artis zee multi-purpose
system) may render the results not generalisable. The
radiographic techniques and acquisition parameters
in models from various manufacturers differ. Every
effort should be made to ensure good radiographic
techniques and to tailor specific examinations to the
indication, patient and user, in an attempt to achieve
the ALARA principle. Third, use of thermoluminescent
dosimeters may better reflect the effective dose to patients, endoscopists, and assistants. Fourth, several
potential confounding factors were not recorded and
controlled for, including endoscopists’ experience,
trainee involvement, specific ERCP procedures (such
as pre-cut sphincterotomy or hilar stent placement), and
patient positioning.[9] However, we believed there was a
high probability that the low-dose setting in our machine
could still offer substantial radiation dose reduction, after
the above-named covariates being adjusted for.
CONCLUSION
Our study devised a simple practical dose reduction
method by adjusting the acquisition parameters on the
fluoroscopy machine during ERCP, without lengthening
the fluoroscopy time or significant compromising image
quality and outcome of ERCP.
REFERENCES
1. Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest
Endosc. 1996;43:1-5. Crossref
2. Kim YJ, Cho KB, Kim ES, Park KS, Jang BK, Chung WJ, et al.
Efficacy of a self-designed protective lead shield in reduction
of radiation exposure dose during endoscopic retrograde
cholangiopancreatography [in Korean]. Korean J Gastroenterol.
2011;57:28-33. Crossref
3. Muniraj T, Aslanian HR, Laine L, Farrell J, Ciarleglio MM,
Deng Y, et al. A double-blind, randomized, sham-controlled
trial of the effect of a radiation-attenuating drape on radiation
exposure to endoscopy staff during ERCP. Am J Gastroenterol.
2015;110:690-6. Crossref
4. Hart D, Hillier MC, Shrimpton PC. Doses to patients from
radiographic and fluoroscopic X-ray imaging procedures in the UK
— 2010 review. Health Protection Agency, Centre for Radiation,
Chemical and Environment Hazards; June 2012.
5. Dumonceau JM, Garcia-Fernandez FJ, Verdun FR, Carinou E,
Donadille L, Damilakis J, et al. Radiation protection in digestive
endoscopy: European Society of Digestive Endoscopy (ESGE)
guideline. Endoscopy 2012;44:408-24. Crossref
6. Johanson JF, Cooper G, Eisen GM, Freeman M, Goldstein JL,
Jensen DM, et al. Quality assessment of ERCP. Endoscopic
retrograde cholangiopancreatography. Gastrointest Endosc.
2002;56:165-9. Crossref
7. European Commission. European Guidelines on Quality Criteria
for Diagnostic Radiographic Images. Luxembourg: European
Commission; 1996.
8. Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM.
Radiation exposure to patients and personnel during interventional
ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287-92. Crossref
9. Jorgensen JE, Rubenstein JH, Goodsitt MM, Elta GH. Radiation
doses to ERCP patients are significantly lower with experienced
endoscopists. Gastrointest Endosc. 2010;72:58-65. Crossref
| Attachment | Size |
|---|---|
| v24n3_Radiation.pdf | 611.62 KB |