Sonographic and Mammographic Features of Different Echogenic Breast Lesions: A Pictorial Essay
PICTORIAL ESSAY
Sonographic and Mammographic Features of Different Echogenic Breast Lesions: A Pictorial Essay
RLS Chan, T Wong, WY Fung, TS Chan, CM Chau, CY Lui, KF Ma
Department of Radiology, Princess Margaret Hospital, Hong Kong
Correspondence: Dr RLS Chan, Department of Radiology, Princess Margaret Hospital, Hong Kong. Email: roischan@gmail.com
Submitted: 17 Oct 2019; Accepted: 28 Oct 2019.
Contributors: All authors designed the study. RLSC and TW acquired the data, analysed the data, and drafted the manuscript. All authors
critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the
final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Kowloon West Cluster Research Ethics Committee (Ref: KWC-2019-0091). Because of the
retrospective nature of the study, the requirement for informed consent from the patients was waived.
INTRODUCTION
Ultrasonography is useful in the evaluation of clinically
and mammographically detected breast masses. It is
particularly useful in dense breasts that are more common
in Asian women than in Caucasian women. According
to the ACR BI-RADS Atlas (2013), hyperechogenicity
is defined as having increased echogenicity relative
to fat or equal to fibroglandular tissue.[1] This pictorial
essay reviews breast lesions that are hyperechoic
or heterogeneous with hyperechoic components on
ultrasonography. Imaging features are highlighted to
help differentiate between different echogenic lesions,
and additional sonographic features that warrant biopsy.
Benign and malignant lesions with pathological proof are
shown with imaging and causes of echogenic appearance
of breast lesions; their diagnosis, investigation and
management are discussed.
BENIGN LESIONS
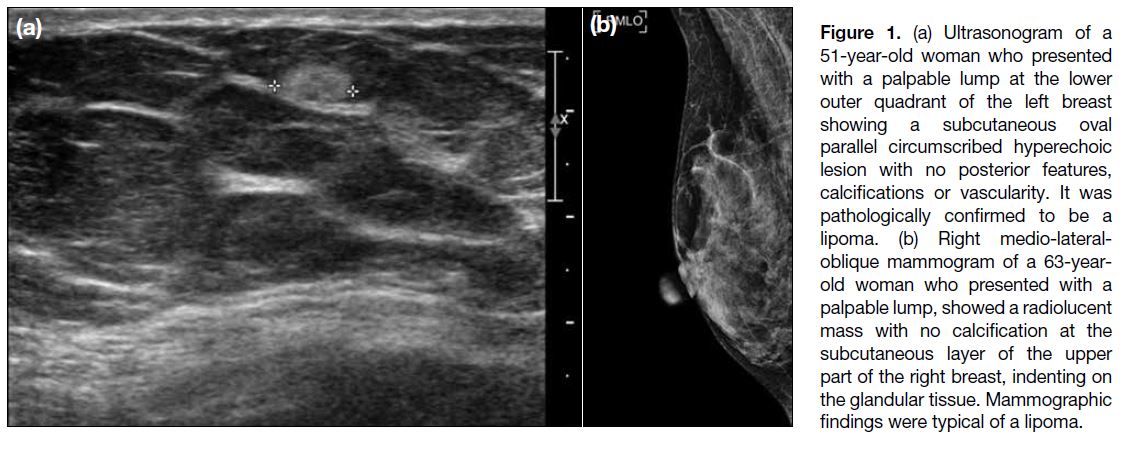
Lipoma
Lipoma is the most common echogenic breast lesion,
and the most common pathology of biopsied echogenic
lesions at our hospital. Clinically, they present as
painless mobile soft lumps. Biopsy proven lipomas are typically homogenously echogenic because of closely
packed adipose tissue due to proliferation. When small,
they are usually oval and show no vascularity (Figure 1).
They are often not evident on mammogram due to their
small size and location at the subcutaneous fat that is also
of fat density. When large, they appear as a fat-density
lesion with thin rim on mammogram which confirms the
diagnosis. If atypical features such as hypoechogenicity
or isoechogenicity are present, these lesions may be
followed up or biopsied. Enlargement of lipomas on
serial scanning is possible as they can enlarge with
hormonal stimulation.[2]
Figure 1. (a) Ultrasonogram of a
51-year-old woman who presented
with a palpable lump at the lower
outer quadrant of the left breast
showing a subcutaneous oval
parallel circumscribed hyperechoic
lesion with no posterior features,
calcifications or vascularity. It was
pathologically confirmed to be a
lipoma. (b) Right medio-lateral-oblique
mammogram of a 63-year-old
woman who presented with a
palpable lump, showed a radiolucent
mass with no calcification at the
subcutaneous layer of the upper
part of the right breast, indenting on
the glandular tissue. Mammographic
findings were typical of a lipoma.
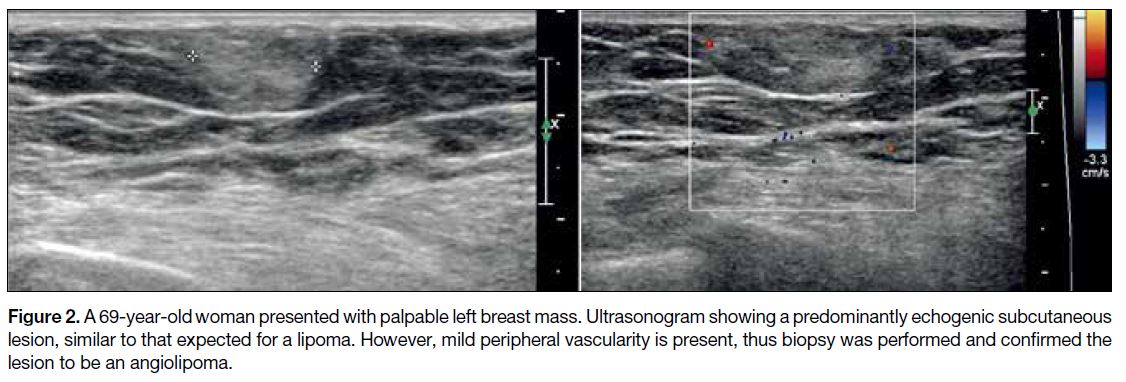
Angiolipoma
Angiolipomas are variants of lipomas, with vascular
proliferation among mature adipocytes. Similar to
lipomas, angiolipomas present as painless palpable
masses and are benign. Angiolipomas are described as
uncommon in the literature[3] but are quite commonly
encountered in our pathology specimens of echogenic
lesions. Sonographic features are similar to those of
lipomas, appearing as subcutaneous circumscribed
isoechoic to echogenic lesions, but they sometimes
show increased vascularity. Angiolipomas cannot be differentiated from lipomas if no increased vascularity is
seen on sonography (Figure 2). If increased vascularity
is present, biopsy is warranted to exclude a malignant
cause.[4]
Figure 2. A 69-year-old woman presented with palpable left breast mass. Ultrasonogram showing a predominantly echogenic subcutaneous
lesion, similar to that expected for a lipoma. However, mild peripheral vascularity is present, thus biopsy was performed and confirmed the
lesion to be an angiolipoma.
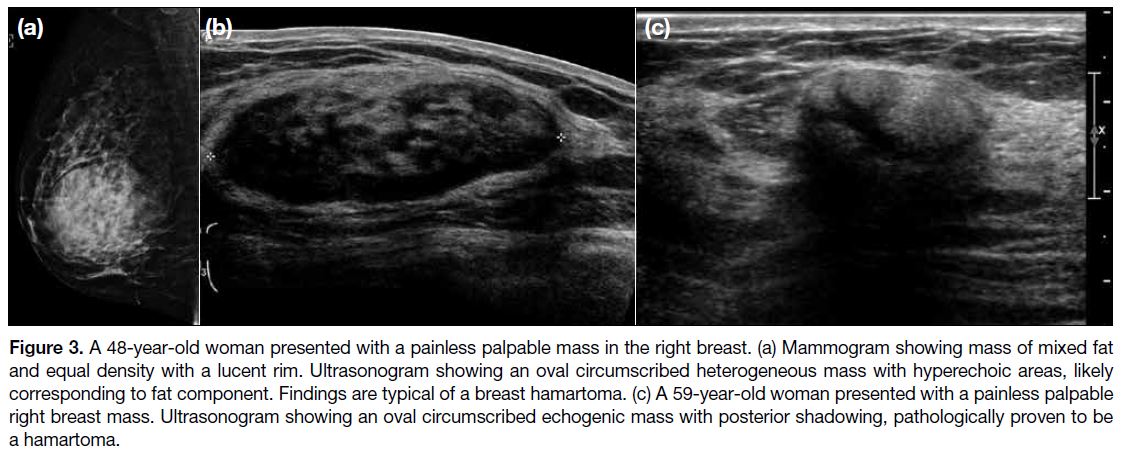
Hamartoma
Hamartomas are benign lesions that contain glandular,
fibrous, and fatty tissue. They usually present as painless
masses or as an incidental finding. Breast-within-a-breast
appearance describes the typical mammographic finding
of a well-defined mixed density mass with similar
appearance to the breast itself. A thin lucent rim of fatty
glandular tissue on mammogram, and a corresponding
echogenic rim on sonography may be seen (Figure 3).
Echogenicity of the lesion varies depending on the
amount of fat inside the hamartoma.[2] Biopsy is not
required in cases with a typical appearance.
Figure 3. A 48-year-old woman presented with a painless palpable mass in the right breast. (a) Mammogram showing mass of mixed fat
and equal density with a lucent rim. Ultrasonogram showing an oval circumscribed heterogeneous mass with hyperechoic areas, likely
corresponding to fat component. Findings are typical of a breast hamartoma. (c) A 59-year-old woman presented with a painless palpable
right breast mass. Ultrasonogram showing an oval circumscribed echogenic mass with posterior shadowing, pathologically proven to be
a hamartoma.
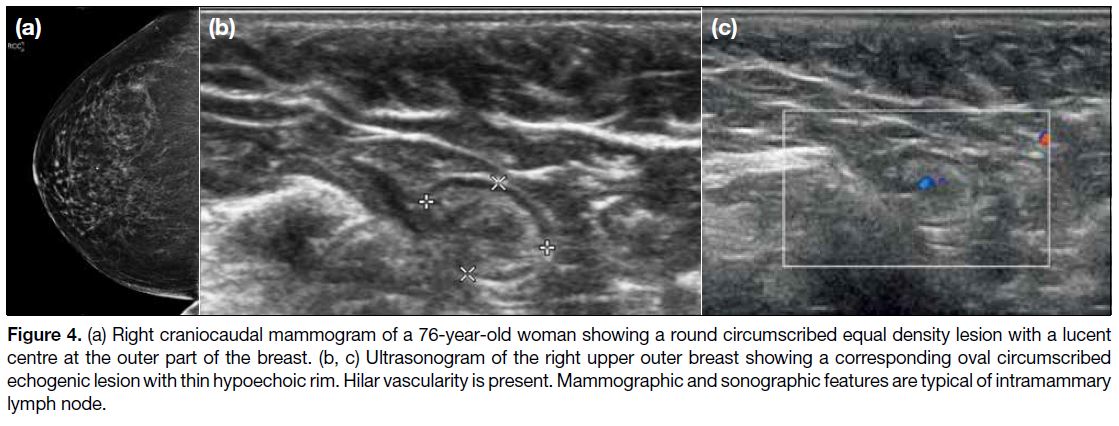
Intramammary Lymph Node
Intramammary lymph nodes are most commonly located
at the upper outer quadrant of the breast. Typical features
of echogenic fatty hilum, oval shape, and hilar vascularity
are often present (Figure 4). They may be obscured on
mammogram due to the presence of adjacent glandular
breast tissue. If imaging features are typical, biopsy is
not required.[5]
Figure 4. (a) Right craniocaudal mammogram of a 76-year-old woman showing a round circumscribed equal density lesion with a lucent
centre at the outer part of the breast. (b, c) Ultrasonogram of the right upper outer breast showing a corresponding oval circumscribed
echogenic lesion with thin hypoechoic rim. Hilar vascularity is present. Mammographic and sonographic features are typical of intramammary
lymph node.
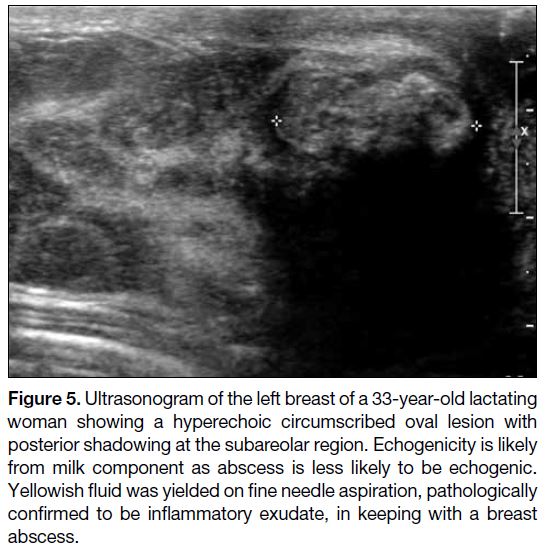
Abscess/Infected Galactocele
Abscesses often occur in lactating women who first
present with fever, breast erythema and pain due to
background mastitis, then later with a developing lump.
Less commonly, abscesses may occur in non-lactating
women with predisposing factors such as diabetes,
smoking, and superimposed infection in cysts or duct
ectasia. Diagnosis is usually made by history and sonographic appearance. Abscesses are often hypoechoic
or of mixed cystic-solid appearance, although they may
sometimes be hyperechoic due to the presence of debris
or retention of infected milk (Figure 5). Often there is
increased vascularity on Doppler assessment. Diagnosis
by imaging is often adequate, but if it does not resolve on
interval imaging, biopsy is necessary to exclude the rare
possibility of inflammatory breast cancer. If the abscess
is already liquefied or partially liquefied, treatment is
usually a combination of antibiotics and drainage by fine
needle aspiration, which often needs to be repeated. If it is
just early inflammatory change or phlegmon, antibiotics
and interval close follow-up scan are sufficient.[6]
Figure 5. Ultrasonogram of the left breast of a 33-year-old lactating
woman showing a hyperechoic circumscribed oval lesion with
posterior shadowing at the subareolar region. Echogenicity is likely
from milk component as abscess is less likely to be echogenic.
Yellowish fluid was yielded on fine needle aspiration, pathologically
confirmed to be inflammatory exudate, in keeping with a breast
abscess.
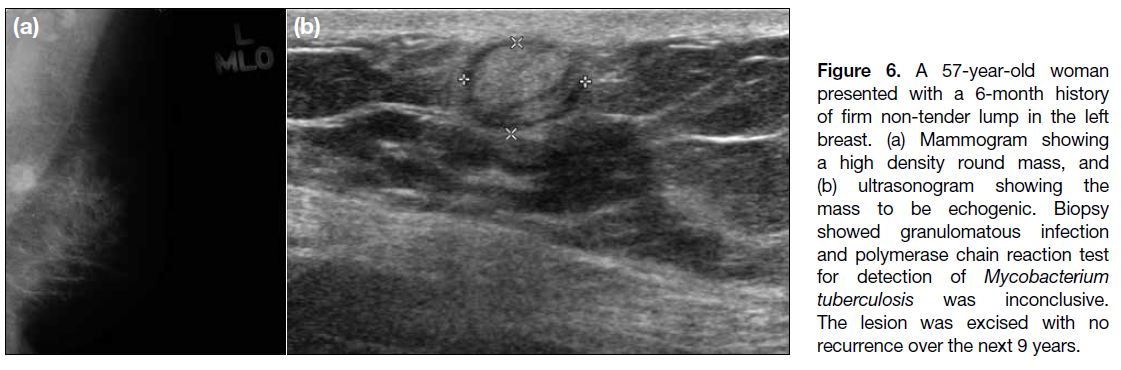
Granulomatous Mastitis
Granulomatous mastitis is considered rare in Caucasian
patients, but is commonly encountered in Asian patients
in Hong Kong.[7] It presents with a hard, often painless, mass. Mammography usually shows an equal to high
density mass, with corresponding echogenic lesion
on sonography (Figure 6).[8] With a biopsy result of
granulomatous reaction, the specimen is usually sent
for a polymerase chain reaction test for detection of
Mycobacterium tuberculosis, but most cases are shown
to be idiopathic (or related to autoimmune disease) rather
than related to infection. Treatment involves monitoring,
corticosteroids, antibiotics, or surgical resection,
depending on the cause and size of the lesion.
Figure 6. A 57-year-old woman
presented with a 6-month history
of firm non-tender lump in the left
breast. (a) Mammogram showing
a high density round mass, and
(b) ultrasonogram showing the
mass to be echogenic. Biopsy
showed granulomatous infection
and polymerase chain reaction test
for detection of Mycobacterium
tuberculosis was inconclusive.
The lesion was excised with no
recurrence over the next 9 years.
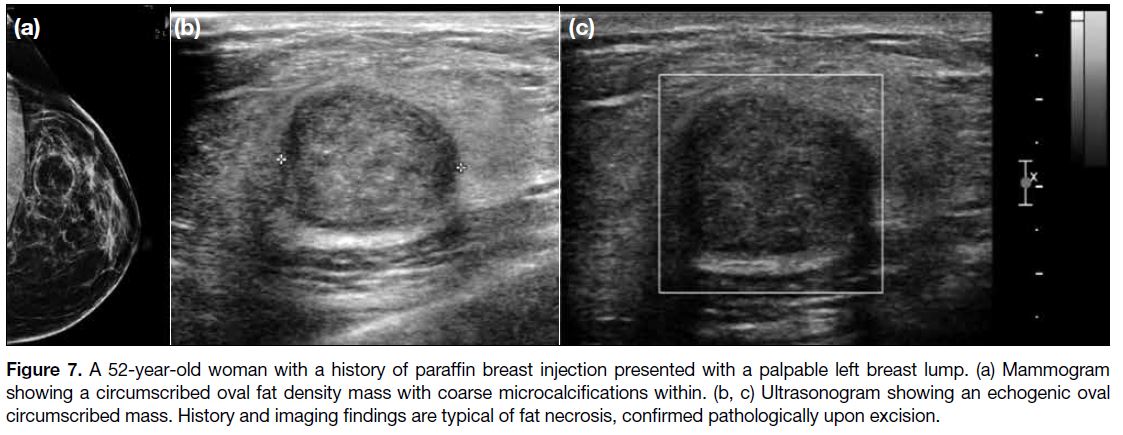
Fat Necrosis
Fat necrosis is a common condition that has a variety
of mammographic and sonographic appearances. It
mimics the appearance of other breast lesions due to the
variable mixture of fat, fibrotic and calcific components
(Figure 7).[2] Biopsy is often required unless there is a typical history of trauma or previous intervention,
together with typical fat appearance with calcifications
on mammography.
Figure 7. A 52-year-old woman with a history of paraffin breast injection presented with a palpable left breast lump. (a) Mammogram
showing a circumscribed oval fat density mass with coarse microcalcifications within. (b, c) Ultrasonogram showing an echogenic oval
circumscribed mass. History and imaging findings are typical of fat necrosis, confirmed pathologically upon excision.
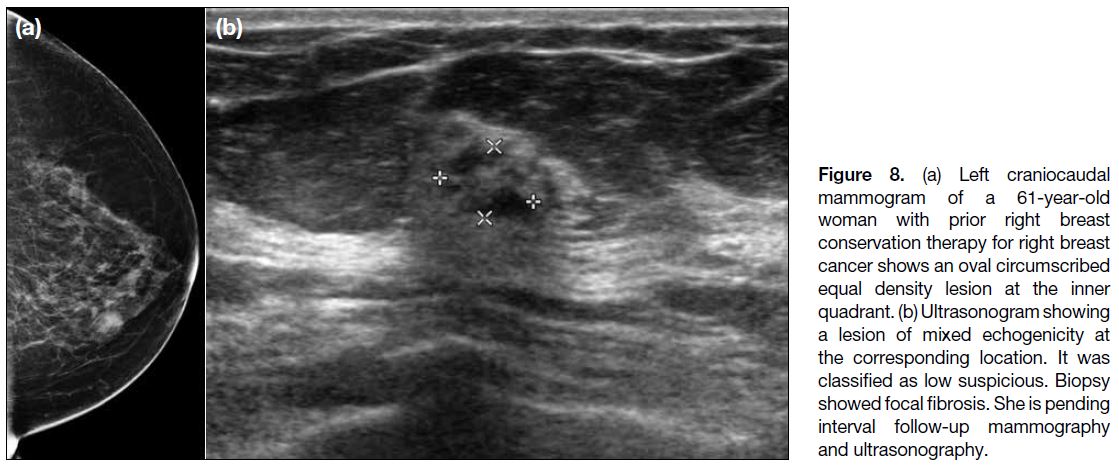
Focal Fibrosis
Focal fibrosis is another common pathological result of
echogenic breast lesions, but not frequently described in
the literature. It is often of equal density on mammogram
and mixed echogenicity on ultrasonography (Figure 8),
due to clustering of thick fibrous stroma.[9] There are no
pathognomonic imaging features to distinguish it from
tumours that can appear similar, thus diagnosis is by
biopsy. When biopsy yields a pathological result of focal
fibrosis, careful review of pathological-radiological
concordance should be carried out.[10] For slightly
discordant cases, follow-up imaging may be considered
but a false-negative result is rare.[11]
Figure 8. (a) Left craniocaudal
mammogram of a 61-year-old
woman with prior right breast
conservation therapy for right breast
cancer shows an oval circumscribed
equal density lesion at the inner
quadrant. (b) Ultrasonogram showing
a lesion of mixed echogenicity at
the corresponding location. It was
classified as low suspicious. Biopsy
showed focal fibrosis. She is pending
interval follow-up mammography
and ultrasonography.
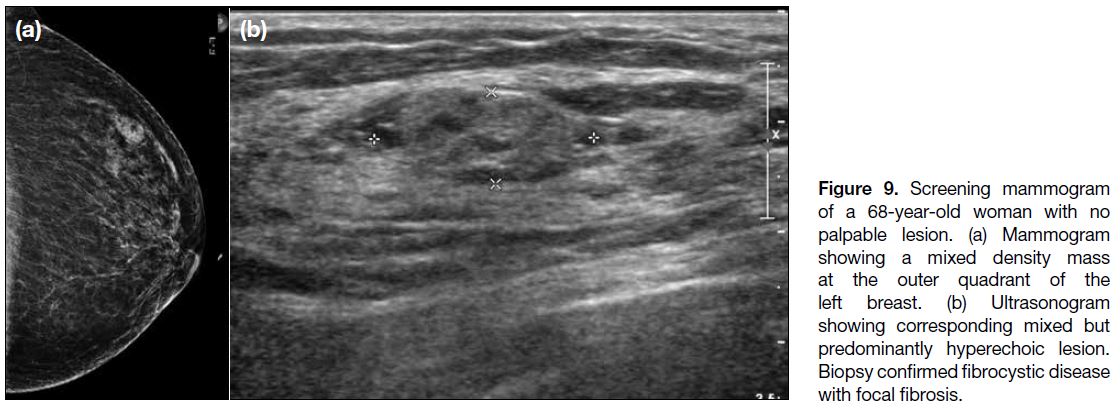
Fibrocystic Disease/Apocrine Metaplasia
Fibrocystic disease usually presents with cyclical breast
pain and palpable tender nodules and is often bilateral. Its
imaging appearance is variable. On mammography, the
breasts are often heterogenous or dense, with partially
circumscribed masses that probably correspond to the
cystic component. On ultrasonography, there is often
diffuse heterogeneous echogenicity, with microcysts
within (Figure 9). Occasionally, fibrocystic disease may
appear mass-like. Imaging features overlap with other
echogenic breast lesions that also appear as an equal
density mass on mammogram, thus diagnosis is usually
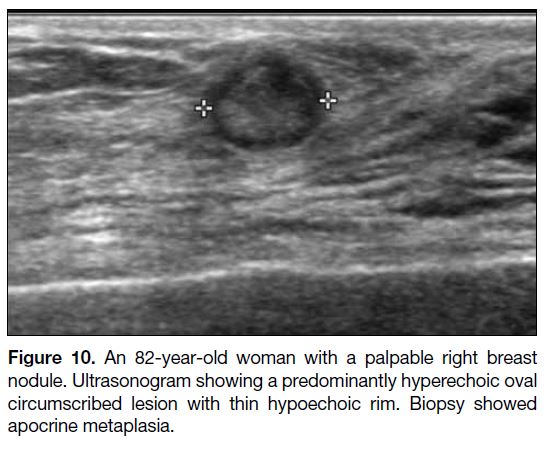
by biopsy. Apocrine metaplasia is a variant of fibrocystic
change and usually appears as a cluster of microcysts but
occasionally mimics an intracystic echogenic nodule
(Figure 10).[12]
Figure 9. Screening mammogram
of a 68-year-old woman with no
palpable lesion. (a) Mammogram
showing a mixed density mass
at the outer quadrant of the
left breast. (b) Ultrasonogram
showing corresponding mixed but
predominantly hyperechoic lesion.
Biopsy confirmed fibrocystic disease
with focal fibrosis.
Figure 10. An 82-year-old woman with a palpable right breast
nodule. Ultrasonogram showing a predominantly hyperechoic oval
circumscribed lesion with thin hypoechoic rim. Biopsy showed
apocrine metaplasia.
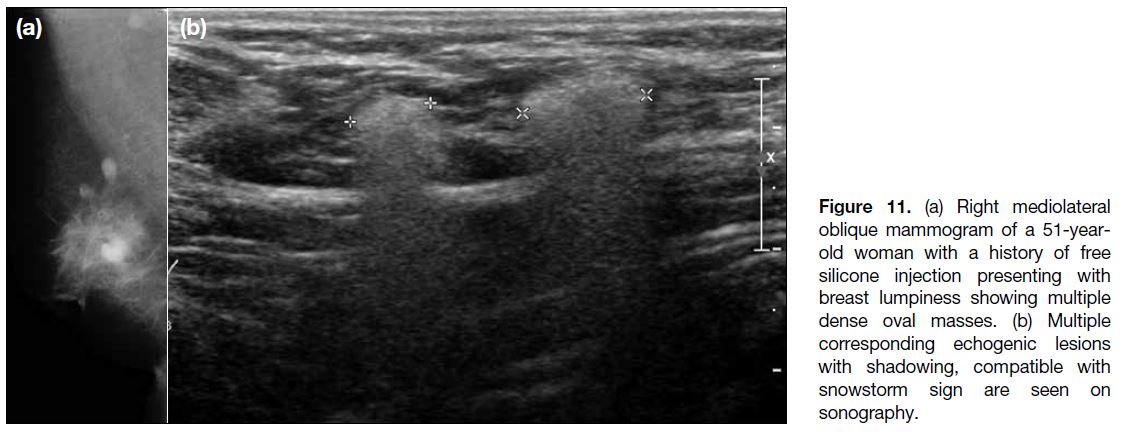
Free Silicone/Silicone Implant
Silicone within the parenchyma, including free silicone
injection, extravasated silicone from a ruptured implant
or silicone confined within an implant bag, should
all have a characteristic snowstorm appearance on
ultrasonography (due to silicone acoustic scattering)
[Figure 11].[13] Silicone granulomas are inflammatory
lesions due to a foreign body reaction to free silicone
in the breast. In patients with breast implants,
they can be associated with extracapsular rupture.
Extravasated silicone or silicone gel bleed can travel
through the lymphatics and lodge in the lymph nodes,
which then exhibit similar characteristics. Common
locations of silicone granuloma are therefore at the
edge of the implant or the axilla. Magnetic resonance
imaging is another imaging modality of choice to
evaluate augmented breasts.[14] Silicone granuloma may
sometimes mimic malignancy. Biopsy is needed when
there are other suspicious features or if there is clinical
concern.
Figure 11. (a) Right mediolateral
oblique mammogram of a 51-year-old
woman with a history of free
silicone injection presenting with
breast lumpiness showing multiple
dense oval masses. (b) Multiple
corresponding echogenic lesions
with shadowing, compatible with
snowstorm sign are seen on
sonography.
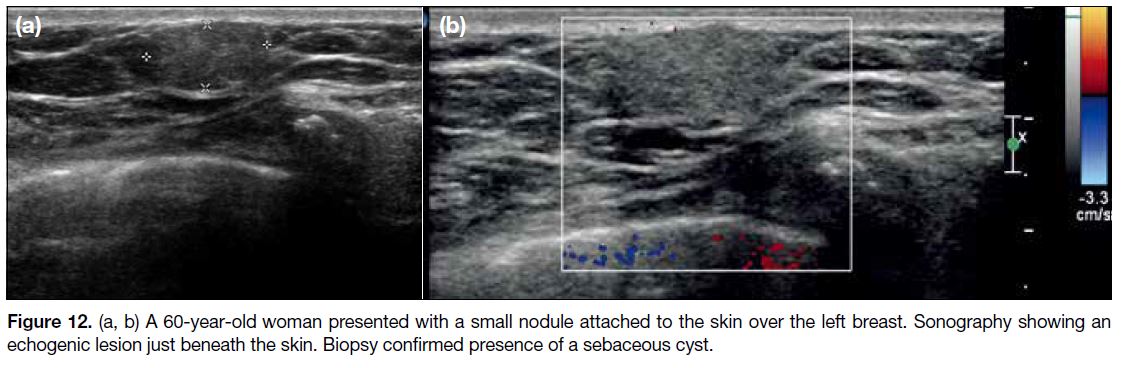
Sebaceous Cyst
Sebaceous cyst is a lesion located at or just below the
skin, often related to hair follicles. It can be of any
echogenicity, but usually shows no increased vascularity
unless inflamed (Figure 12). Biopsy and treatment are
not required.[12]
Figure 12. (a, b) A 60-year-old woman presented with a small nodule attached to the skin over the left breast. Sonography showing an
echogenic lesion just beneath the skin. Biopsy confirmed presence of a sebaceous cyst.
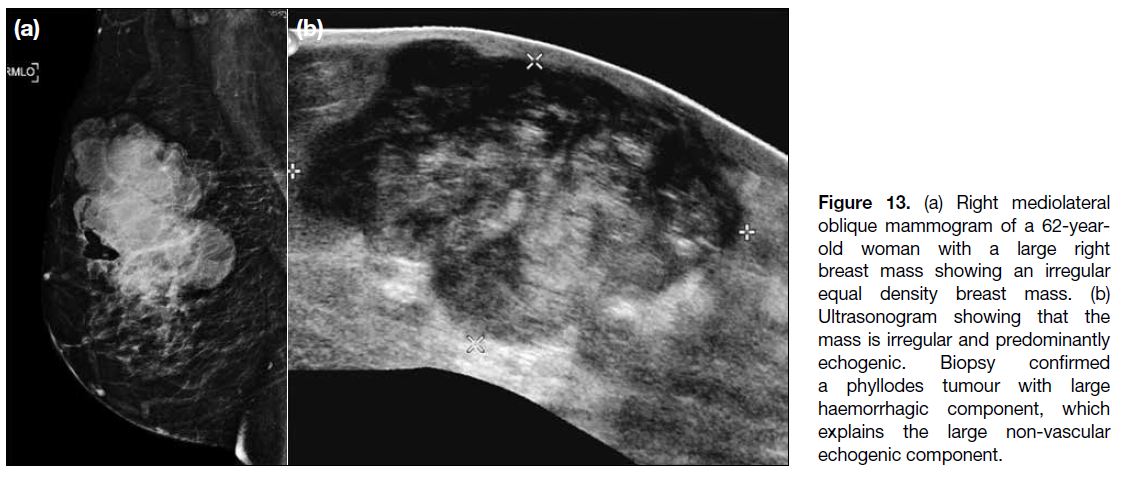
Haematoma
This diagnosis is considered when patients volunteer
a clear history of trauma, interventional procedure,
or surgery. Most breast tumours are hypoechoic, but
haemorrhage in vascular tumours will add an echogenic
component to the mass. Sonographic appearance is
variable dependent on the age of the haematoma.
Hematomas are hypoechoic at the acute stage, complex
cystic-solid at the subacute stage and become hyperechoic
when chronic (Figure 13). With a clear history, early
follow-up for shrinkage is adequate. Biopsy is indicated
for non-resolving or enlarging lesions to exclude
bleeding tumour.[12]
Figure 13. (a) Right mediolateral
oblique mammogram of a 62-year-old
woman with a large right
breast mass showing an irregular
equal density breast mass. (b)
Ultrasonogram showing that the
mass is irregular and predominantly
echogenic. Biopsy confirmed
a phyllodes tumour with large
haemorrhagic component, which
explains the large non-vascular
echogenic component.
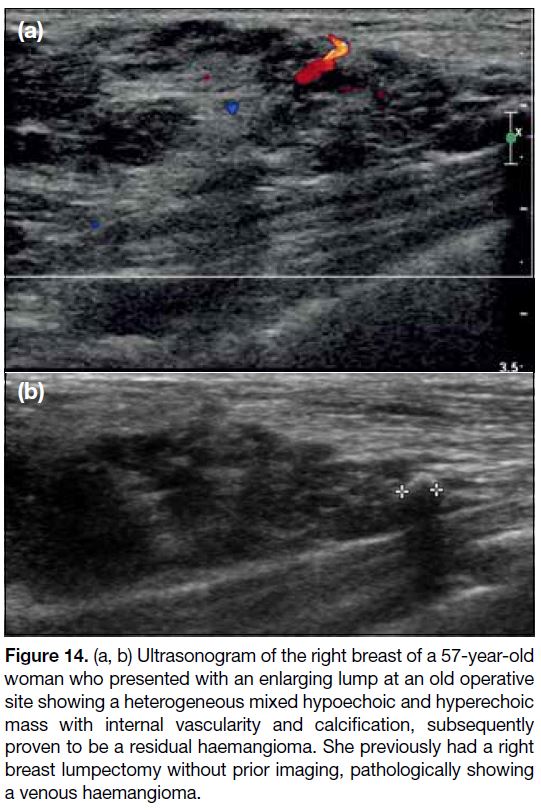
Haemangioma
Haemangiomas are rare benign breast tumours that are
often asymptomatic and usually an incidental finding
on screening mammograms. They are often located
superficially. The most common mammographic
appearance is that of a lobulated mass, rarely with coarse
or punctate calcifications. On sonography, they are
usually oval with circumscribed margins. Echogenicity
and vascularity on Doppler examination are variable,
depending on the proportion of capillary, venous and
fibrous components (Figure 14).[3] [15] Diagnosis is usually
made on biopsy in view of the non-specific appearance.
Lesions with non-classic imaging or pathological
features should be excised, as angiosarcoma should
be excluded.[15] Management of haemangiomas with
pathological-radiological concordance is controversial,
and the decision for conservative versus surgical
management should be made following discussion
between the patient and surgeon.[16]
Figure 14. (a, b) Ultrasonogram of the right breast of a 57-year-old
woman who presented with an enlarging lump at an old operative
site showing a heterogeneous mixed hypoechoic and hyperechoic
mass with internal vascularity and calcification, subsequently
proven to be a residual haemangioma. She previously had a right
breast lumpectomy without prior imaging, pathologically showing
a venous haemangioma.
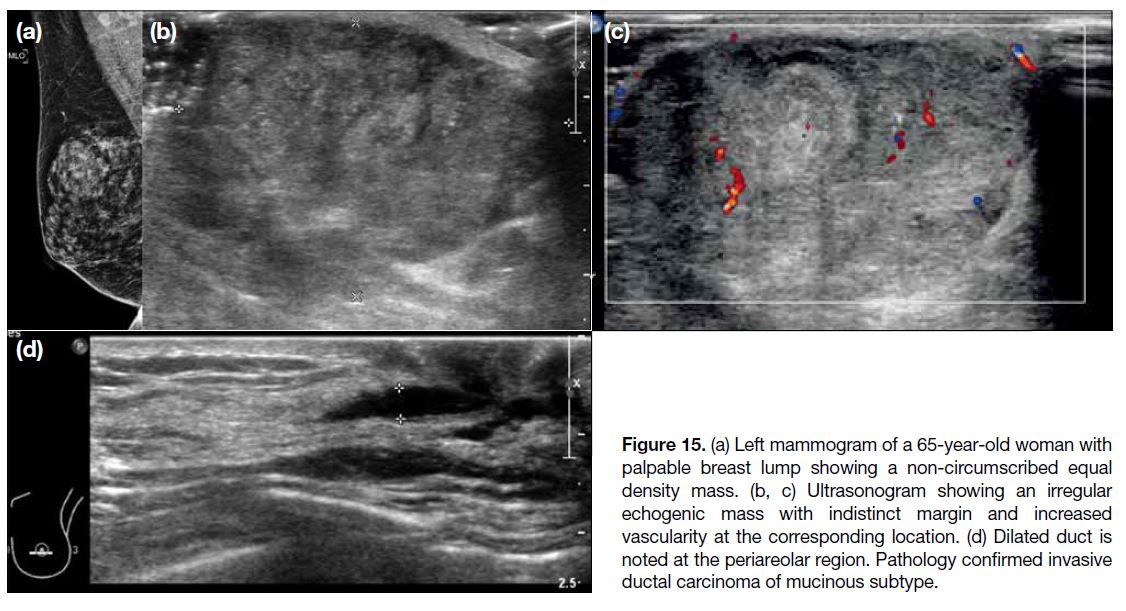
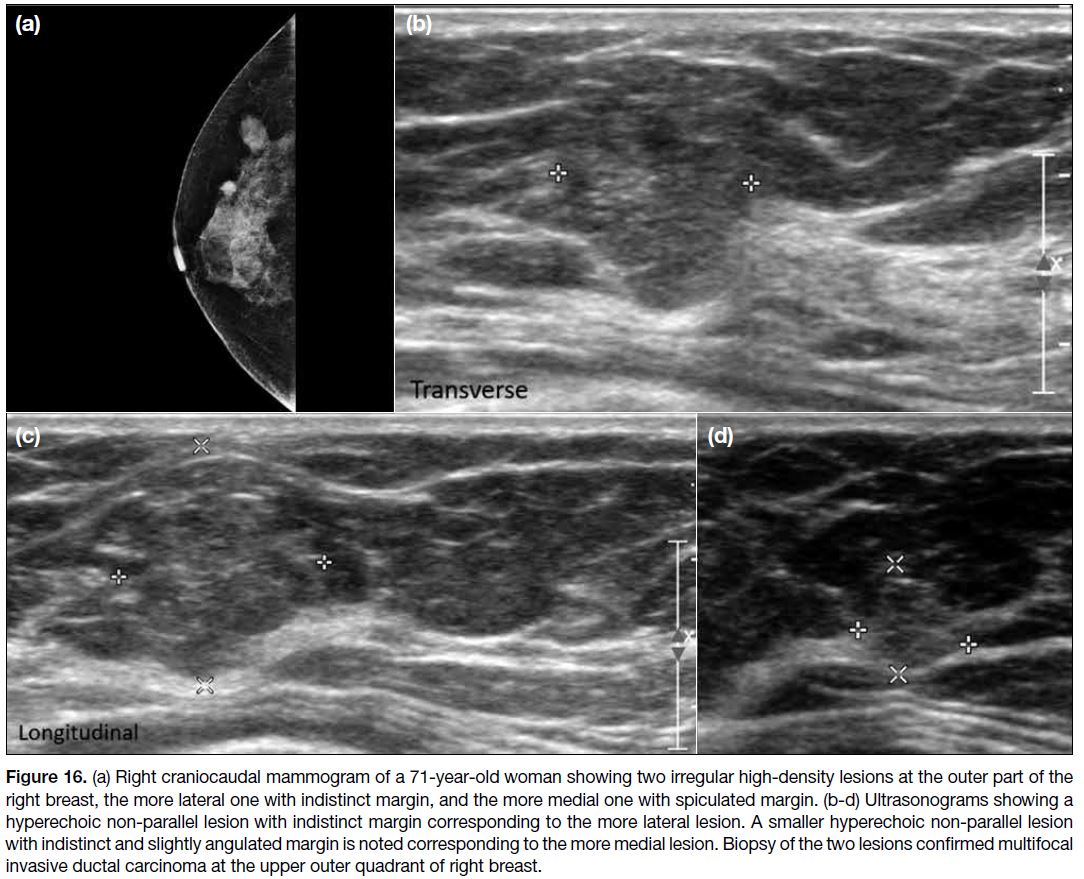
MALIGNANT LESIONS
Primary Breast Carcinomas
The majority of primary breast carcinomas are
hypoechoic on ultrasonography; however, a minority
appears hyperechoic. The question is then how to
distinguish a malignant hyperechoic tumour from a benign
one. In our experience, breast carcinomas with echogenic
appearance on sonography have a corresponding equal or
high-density mass on mammogram (Figures 15 and 16).
In addition, pathologically confirmed breast cancers with
echogenic appearance have at least one of the following
sonographic features: indistinct, spiculated or angular margins; irregular shape; non-parallel and/or increased
internal vascularity (Figures 15 and 16). These features
also correspond with sonographic features described
in the literature to differentiate between malignant and benign lesions.[17] In other words, echogenicity does not
trump morphological appearance. These features may
provide reassurance to our future practice in deciding
which echogenic lesions to biopsy, and to safely label
other lesions as benign or probably benign.
Figure 15. (a) Left mammogram of a 65-year-old woman with
palpable breast lump showing a non-circumscribed equal
density mass. (b, c) Ultrasonogram showing an irregular
echogenic mass with indistinct margin and increased
vascularity at the corresponding location. (d) Dilated duct is
noted at the periareolar region. Pathology confirmed invasive
ductal carcinoma of mucinous subtype.
Figure 16. a) Right craniocaudal mammogram of a 71-year-old woman showing two irregular high-density lesions at the outer part of the
right breast, the more lateral one with indistinct margin, and the more medial one with spiculated margin. (b-d) Ultrasonograms showing a
hyperechoic non-parallel lesion with indistinct margin corresponding to the more lateral lesion. A smaller hyperechoic non-parallel lesion
with indistinct and slightly angulated margin is noted corresponding to the more medial lesion. Biopsy of the two lesions confirmed multifocal
invasive ductal carcinoma at the upper outer quadrant of right breast.
In addition, in our experience, echogenic primary breast
tumours are typically invasive ductal carcinomas, with
the majority being a mucinous subtype. However, in the
literature, hyperechoic lesions are reported to be more
frequent in invasive lobular carcinoma than invasive
ductal carcinoma.[18]
Sarcomas
Sarcomas are rare aggressive stromal neoplasms of the
breast, constituting 0.04% of all breast cancers.
Angiosarcomas are rare malignant tumours that arise
from the endothelial cells of vascular channels. They
may present as skin plaques or palpable masses. Prior
radiation therapy is a risk factor. To differentiate
from haemangiomas, angiosarcomas are usually
intraparenchymal (rather than subcutaneous), and usually
are larger (>3 cm) at diagnosis. Mammographically,
they are usually an ill-defined irregular mass with
no calcifications. Sonographically, they are often
hypoechoic, but have been reported as hyperechoic.[19]
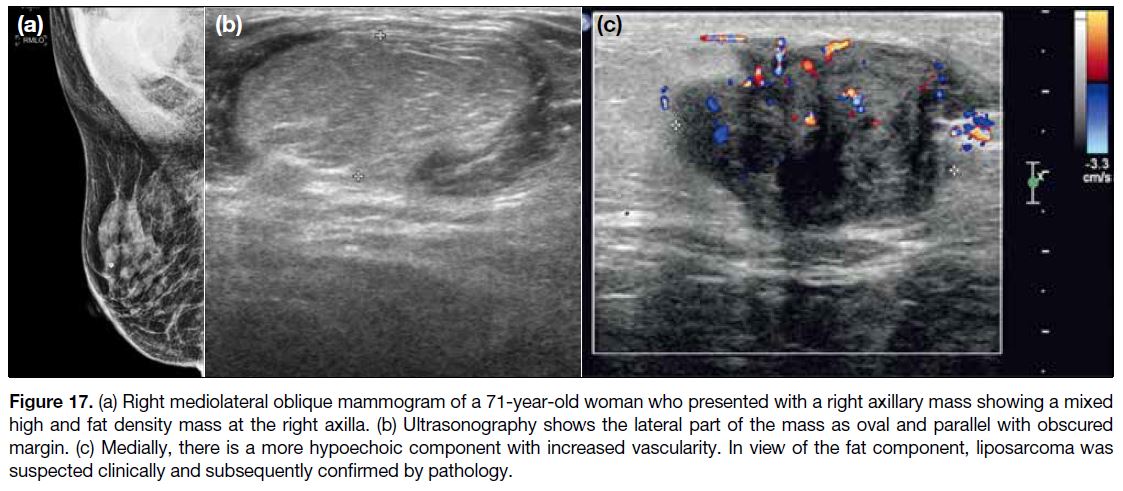
Liposarcomas of the breast are extremely rare
constituting only 0.3% of all mammary sarcomas.
They occur de novo or derive from a phyllodes tumour.
On mammography, liposarcomas are of high density,
mixed with fat density. On ultrasonography, they are
predominantly hypoechoic, with echogenic regions
corresponding to fat, dense vascular and stromal
components (Figure 17). Increased vascularity is often
present.[20]
Figure 17. (a) Right mediolateral oblique mammogram of a 71-year-old woman who presented with a right axillary mass showing a mixed
high and fat density mass at the right axilla. (b) Ultrasonography shows the lateral part of the mass as oval and parallel with obscured
margin. (c) Medially, there is a more hypoechoic component with increased vascularity. In view of the fat component, liposarcoma was
suspected clinically and subsequently confirmed by pathology.
These patients are treated surgically with or without
adjuvant radiation and chemotherapy. Prognosis is
grave due to the high rate of recurrence and metastasis.
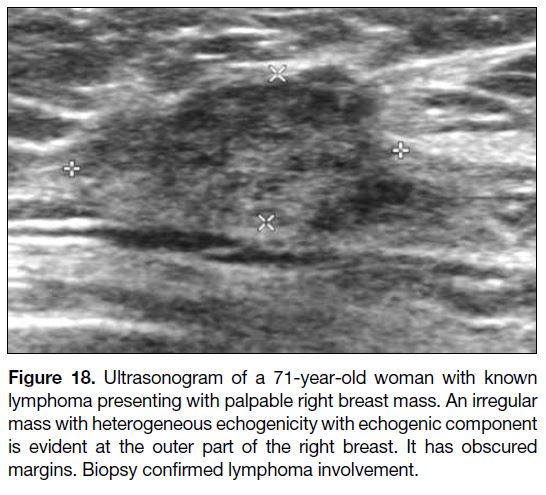
Primary Breast Lymphoma
Primary breast lymphoma is rare and constitutes less than
0.5% of all breast cancers. It is defined as lymphoma with
breast the only organ affected. It usually presents as a
palpable solitary mass. The most typical mammographic
feature is of a solitary lobular or irregular mass; non-calcified
and non-spiculated, unlike primary breast
carcinoma. Sonographically, it is usually hypoechoic
with increased vascularity, but mixed hyperechoic
and hypoechoic appearance has also been described
(Figure 18).[21] Diagnosis is by biopsy. There is no
standard treatment regimen.
Figure 18. Ultrasonogram of a 71-year-old woman with known
lymphoma presenting with palpable right breast mass. An irregular
mass with heterogeneous echogenicity with echogenic component
is evident at the outer part of the right breast. It has obscured
margins. Biopsy confirmed lymphoma involvement.
Metastasis
Metastasis to the breast is uncommon, constituting less
than 2% of breast cancers. The more common primary
tumours to metastasise to the breast include secondary
lymphoma and melanoma. Lung cancer, ovarian cancer
and rhabdomyosarcoma are less commonly indicated.[22]
Lymphoma is the most common tumour to metastasise
to the breast. Melanoma has also been described
to metastasise to the breast, but no case has been
encountered at our unit, likely because melanoma is rare in Hong Kong.
Most metastases present as multiple bilateral palpable
painless breast masses. Breast metastases are usually
non-calcified and non-spiculated on mammography,
unlike primary breast carcinoma. Sonographically, they
are more often hypoechoic, but hyperechoic lesions have
also been described.[23]
CAUSES OF ECHOGENIC APPEARANCE IN BREAST LESIONS
Lesions appear echogenic because they reflect more
of the sound emitted by the ultrasound probe. More
reflection occurs when two adjacent tissues have greater
differences in acoustic impedance, such as at an interface
between fat and soft tissue, or between fibrous tissue and
soft tissue. As fat, fibrous tissue, milk, silicone and blood
products all have a lower acoustic impedance than soft
tissue, such lesions have a typical or not uncommon
echogenic appearance on ultrasonography.
The majority of echogenic lesions are benign. Fat-containing
benign lesions include lipoma, angiolipoma,
hamartoma, intramammary lymph node (fatty hilum),
fat necrosis and sebaceous cysts. Fibrous lesions include
focal fibrosis, fibrocystic disease and haemangioma
(fibrous stroma). Galactoceles, silicone granulomas, and
haematomas are echogenic because of the milk content,
silicone, and blood products, respectively. Malignant
echogenic lesions are uncommon, the main cause being
liposarcoma, where assessment of its ultrasound features
may differentiate from other benign entities.
Some echogenic lesions that we have encountered
have a more common hypoechoic appearance. They
include non-lactation-related abscesses, granulomatous
mastitis, primary breast carcinoma, sarcoma, secondary
lymphoma, and metastases. In particular, tumours are
usually hypoechoic as they have higher density than
normal soft tissue, and thus have a higher acoustic
impedance.
The likely reason for the echogenic appearance in isolated
tumour cases is unclear although a previous case report
described an unusual case of hyperechoic liver nodule
caused by Hodgkin’s lymphoma, showing increased
fat deposition inside the hepatocytes surrounded by
lymphoma infiltrates in the pathological specimen.[22]
Increased fat deposition has been postulated as a cause of
increased echogenicity in secondary breast lymphoma,
although there is no similar case report correlating
the sonographic appearance to histopathological
characteristics of breast tumours.
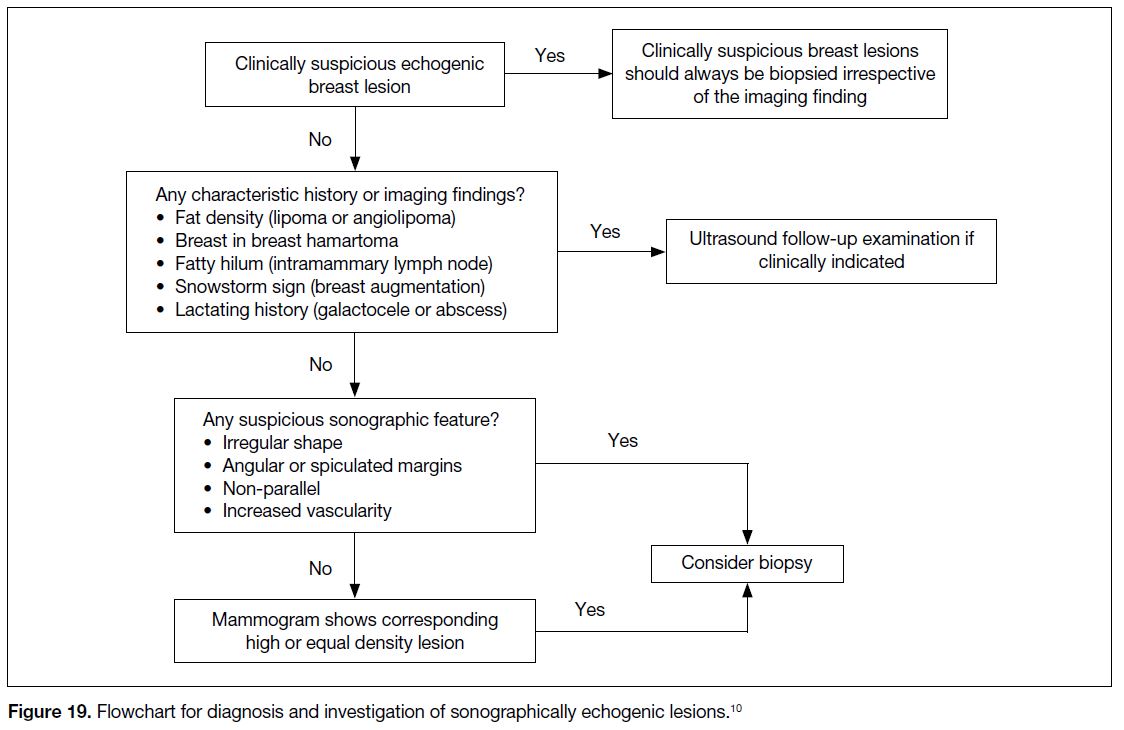
DIAGNOSIS INVESTIGATION AND MANAGEMENT
Particular patient characteristics and additional
sonographic and mammographic features help
differentiate between various benign and malignant
echogenic breast lesions (Figure 19 [10]).
Figure 19. Flowchart for diagnosis and investigation of sonographically echogenic lesions.[10]
Patient history should always be reviewed, as previous
breast augmentation; lactating history and septic features
in a patient with suspected breast abscess; and history
of recent intervention in a patient with suspected
haematoma will aid diagnosis and prevent unnecessary
biopsy.
Recognising certain specific appearances, such as the
breast-in-breast appearance of hamartomas, echogenic
fatty hilum of intramammary lymph nodes and snowstorm sign in augmented breasts will prevent biopsy of certain
benign echogenic breast lesions.
CONCLUSION
The vast majority of echogenic breast lesions are benign,
but it is vital to not miss diagnosis of the minority that
are malignant. Lesions with suspicious sonographic
features—such as spiculated or angular margins, irregular
shape, or non-parallel or increased internal vascularity—or with corresponding equal or high-density mass on
mammogram should be biopsied.
REFERENCES
1. Mendelson EB, Böhm-Vélez M, Berg WA, Whitman GJ,
Feldman MI, Madjar H, et al. ACR BI-RADS® Ultrasound. In:
ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System.
Reston, VA, American College of Radiology; 2013. p 309.
2. Pui MH, Movson IJ. Fatty tissue breast lesions. Clin Imaging. 2003;27:150-5. Crossref
3. Adrada B, Wu Y, Yang W. Hyperechoic lesions of the breast: radiologic-histopathologic correlation. AJR Am J Roentgenol.
2013;200:W518-30. Crossref
4. Darling ML, Babagbemi TO, Smith DN, Brown FM, Lester SC,
Meyer JE. Mammographic and sonographic features of angiolipoma
of the breast. Breast J. 2000;6:166-70. Crossref
5. Dialani V, Westra C, Venkataraman S, Fein-Zachary V, Brook A, Mehta T. Indications for biopsy of imaging-detected intramammary
and axillary lymph nodes in the absence of concurrent breast cancer.
Breast J. 2018;24:869-75. Crossref
6. Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N,
et al. Breast abscesses: evidence-based algorithms for diagnosis,
management, and follow-up. Radiographics. 2011;31:1683-99. Crossref
7. Patel RA, Strickland P, Sankara IR, Pinkston G, Many W,
Rodriguez M. Idiopathic granulomatous mastitis: case reports and
review of literature. J Gen Intern Med. 2010;25:270-3. Crossref
8. Al-Khawari HA, Al-Manfouhi HA, Madda JP, Kovacs A,
Sheikh M, Roberts O. Radiologic features of granulomatous
mastitis. Breast J. 2011;17:645-50. Crossref
9. Venta LA, Wiley EL, Gabriel H, Adler YT. Imaging features of focal breast fibrosis: mammographic-pathologic correlation of noncalcified breast lesions. AJR. Am J Roentgenol. 1999;173:309-16. Crossref
10. Revelon G, Sherman ME, Gatewood OM, Brem RF. Focal fibrosis of the breast: imaging characteristics and histopathologic
correlation. Radiology. 2000;216:255-9. Crossref
11. Rosen EL, Soo MS, Bentley RC. Focal fibrosis: a common breast
lesion diagnosed at imaging-guided core biopsy. AJR Am J
Roentgenol. 1999;173:1657-62. Crossref
12. Gao Y, Slanetz PJ, Eisenberg RL. Echogenic breast masses at US: to biopsy or not to biopsy? Radiographics. 2013;33:419-34. Crossref
13. DeBruhl ND, Gorczyca DP, Ahn CY, Shaw WW, Bassett LW. Silicone breast implants: US evaluation. Radiology. 1993;189:95-8. Crossref
14. Wong T, Lo LW, Fung PY, Lai HY, She HL, Ng WK, et al. Magnetic resonance imaging of breast augmentation: a pictorial
review. Insights Imaging. 2016;7:399-410. Crossref
15. Mesurolle B, Sygal V, Lalonde L, Lisbona A, Dufresne MP,
Gagnon JH, Kao E. Sonographic and mammographic appearances
of breast hemangioma. AJR Am J Roentgenol. 2008;191:W17-22. Crossref
16. Jesinger RA, Lattin Jr GE, Ballard EA, Zelasko SM, Glassman LM.
Vascular abnormalities of the breast: arterial and venous disorders,
vascular masses, and mimic lesions with radiologic-pathologic
correlation. Radiographics. 2011;31:E117-36. Crossref
17. Hong AS, Rosen EL, Soo MS, Baker JA. BI-RADS for sonography: positive and negative predictive values of sonographic features.
AJR Am J Roentgenology. 2005;184:1260-5. Crossref
18. Cawson JN, Law EM, Kavanagh AM. Invasive lobular carcinoma: sonographic features of cancers detected in a BreastScreen Program. Australas Radiol. 2001;45:25-30. Crossref
19. Glazebrook KN, Magut MJ, Reynolds C. Angiosarcoma of the
breast. AJR Am J Roentgenol. 2008;190:533-8. Crossref
20. Mardi K, Gupta N. Primary pleomorphic liposarcoma of breast: a rare case report. Indian J Pathol Microbiol. 2011;54:124-6. Crossref
21. Lyou CY, Yang SK, Choe DH, Lee BH, Kim KH. Mammographic and sonographic findings of primary breast lymphoma. Clin
Imaging. 2007;31:234-8. Crossref
22. Bartella L, Kaye J, Perry NM, Malhotra A, Evans D, Ryan D, et al. Metastases to the breast revisited: radiological–histopathological
correlation. Clin Radiol. 2003;58:524-31. Crossref
23. Hann A, Trenker C, Westhoff CC, Goerg C. Unusual hyperechoic appearance of Hodgkin’s lymphoma in the liver. Ultrasound Int Open. 2015;1:E25-6. Crossref