Online Psychological Intervention in Breast Cancer Survivors: a Review
REVIEW ARTICLE
Online Psychological Intervention in Breast Cancer Survivors: a Review
M Popovic1, V Rico1, C DeAngelis1, H Lam1, FMY Lim2
1 Odette Cancer Centre, Sunnybrook Health Science Centre, University of Toronto, Toronto, Ontario, Canada
2 Department of Oncology, Prince Margaret Hospital, Hong Kong
Correspondence: Dr FMY Lim, Department of Oncology, Prince Margaret Hospital, Hong Kong. Email: fionalimmy@gmail.com
Submitted: 25 Mar 2020; Accepted: 23 Dec 2020.
Contributors: All authors designed the study. MP and VR acquired the data. All authors analysed the data. MP draft the manuscript. All authors critically revised the manuscript for important intellectual content.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available upon request from the corresponding author.
Acknowledgement: We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Oteia Cancer Research
Fund.
Abstract
Introduction
Online psychotherapy has shown promise in a variety of settings. The goal of this review was to
compare outcomes following online psychotherapy in breast cancer survivors.
Methods
We searched Ovid MEDLINE for randomised controlled trials investigating the benefit of online
psychotherapy relative to controls in breast cancer survivors. We sought to capture data on a standardised pre- and
post-intervention symptom scale. Baseline characteristics were collected, including highest education level achieved,
breast cancer treatment, and description and duration of the psychosocial intervention. Trials were stratified based
on behavioural or psychological indications for treatment. Effect sizes were computed using Cohen’s d.
Results
From an initial search of 99 articles, 838 participants across five relevant studies were included. The
mean age of the women was 51.7 years (range, 50.2-56.9). Each study had a unique indication: insomnia, fatigue,
sexual dysfunction, psychological adjustment, and stress management. Two primary and one secondary outcome
were recorded for each study, for a total of 15. Of the 10 included primary outcomes, women in the intervention
groups showed a statistically significant improvement in nine outcomes. Of the five secondary outcomes, women
in the intervention groups showed a significant improvement on four scales. Effect sizes ranged from 0.33 to 1.10.
Conclusion
Overall, online psychotherapies are effective across a variety of symptom states in breast cancer
survivors. Limitations of online psychotherapy include logistical factors, privacy, personal factors, and availability.
Future studies should compare in-person psychotherapy with online psychotherapy.
Key Words: Internet-based intervention; Psychotherapy; Patient reported outcome measures; Breast neoplasms; Cancer survivors
中文摘要
乳癌康復者線上心理干預的綜述
M Popovic、V Rico、C DeAngelis、H Lam、林美瑩
引言
線上心理治療已在各種場景中顯示其前景。本綜述旨在比較乳癌康復者接受線上心理治療後的效果。
方法
我們從Ovid MEDLINE 搜索隨機對照研究,用以檢視接受線上心理治療的乳癌康復者相比對照組的益處。我們試圖在標準化的干預前和干預後症狀量表上獲取數據。收集基線特徵,包括康復者的教育水平、乳癌治療方案及心理社會干預的描述和持續時間。根據治療的行為或心理指徵對研究進行分層。使用Cohen’s d 計算效應量。
結果
從最初搜索的99份文獻中,納入5份相關研究涉及838名參與者均為女性,平均年齡51.7歲(介乎50.2-56.9歲)。這5項研究分別針對不同的適應症,包括失眠、疲勞、性功能障礙、心理調節和壓力管理,記錄共15個主要結果和次要結果。每項研究分別記錄2個主要結果和1個次要結果。干預組在其中9個主要結果以及5個次要結果中的4個量表均有顯著改善。效應大小範圍介乎0.33至1.10。
結論
總體而言,線上心理治療能有效改善乳癌康復者的多種症狀。線上心理治療的局限性包括後勤因素、隱私、個人因素和可獲取性。未來研究應考慮將面對面的心理治療與線上心理治療進行比較。
INTRODUCTION
Psychotherapy is an interpersonal process designed
to modify several aspects of an individual’s psycho-emotional
state, including feelings, cognition, and
behaviours. Several different types of psychotherapies
(e.g., cognitive behaviour therapy (CBT), interpersonal
therapy, psychodynamic therapy) have been shown to
be efficacious.[1] [2] Data have shown that psychotherapy
has an efficacy similar to that of psychotropic drugs
for disorders such as anxiety and depression,[3] [4] with a
moderate-to-large effect size for depression (d= -0.66,
95% confidence interval [CI]= -0.73 to -0.60) compared
to waitlist controls.[2] [4]
Cancer is a common disease, representing the second
leading cause of death in the United States.[5] Both
cancer itself,[6] and its associated therapies, such as
chemotherapy,[7] produce physical and psychological
adverse effects. The reaction to a cancer diagnosis
can cause neuropsychological stress, such as anxiety,
depression, and fear of recurrence or death, all of which
can adversely impact a patient’s quality of life.[6] There
is increasing support for integrating psychotherapy
in oncology practice. For example, Saeedi et al[6] and
Breitbart et al[8] found that psychotherapy increased the perceived meaning of life[6] and quality of life[8] of cancer
patients, respectively, relative to traditional care. This
supports the notion that psychotherapy can improve a
variety of symptoms in cancer patients.
Given the advances in electronic communication in
the past several decades, there has been increasing
interest in online psychotherapy as an alternative to
face-to-face therapy. Chakrabarti[9] reviewed studies
performing this comparison. The results revealed that
online psychotherapy is reliable, and outcomes are
comparable to that of in-person psychotherapy in many
heterogeneous samples for a variety of measures. These
findings suggest that online psychotherapy may be seen
as a viable alternative to traditional psychotherapy, due
to its similar efficacy for various populations. Due to the
nature of CBT, such as a heavy focus on skills training
and homework, it is the therapeutic approach that is
easiest to transfer to an online format.[10]
There are several studies that have examined the efficacy
of online psychotherapy for breast cancer patients.
Cheung et al[11] aimed to teach women with metastatic
breast cancer positive affect skills through an online
intervention paradigm. Intervention participants showed reductions in both depression and negative affect by the
1-month follow-up (d= -0.81). These participants fell
below the clinical threshold for depression at follow-up,
whereas control participants did not fall below clinical
threshold.
Despite the positive oncologic treatment outcomes that
are experienced by many patients with breast cancer,
psycho-emotional, behavioural, and physical symptoms
may still persist even after breast cancer has been treated
and/or cured.[12] Such challenges tend to be overlooked by
healthcare professionals, since the individual has been
deemed ‘cured’,[13] resulting in reduced support when
transitioning from active cancer to the survivorship
stage. A study conducted by Mitchell[13] examined the
occurrence of depression in long-term survivors of
breast cancer, and found that 10% of these individuals
exhibited clinical depression, despite being diagnosed
≥3 years prior. Another study[12] looked at the
symptomology of breast cancer survivors (BCS) and
described four presentation classes: symptoms within
normal limits, pain with fatigue and sleep disturbances,
depression with fatigue and symptom disturbances,
and high symptom burden. Other issues that have been
linked to additional stress for BCS are the financial
burdens associated with treatment,[14] and a fear of cancer
recurrence.[15] This suggests that when women shift to the
survivor stage of breast cancer, there are still a multitude
of factors that can trigger or exacerbate psychological
symptomatology.
The purpose of this review was to examine the efficacy
of online therapy treatments for BCS. By identifying
useful therapies, we aimed to raise awareness of useful
support available for BCS.
METHODS
Search Strategy, Inclusion Criteria, Study
Selection
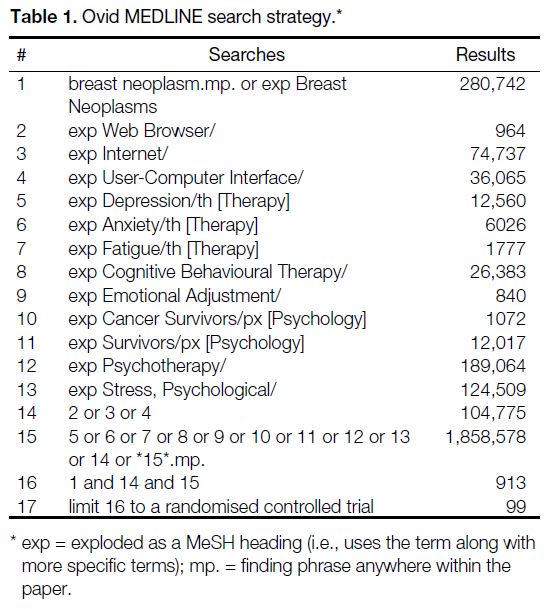
A literature search was conducted using Ovid MEDLINE
and MEDLINE In-Process (inception to July 2019) to
identify relevant studies (Table 1). Articles were eligible
for inclusion if they (1) were a randomised controlled trial
(RCT), (2) included only adult BCS (aged ≥18 years),
(3) compared online psychosocial therapy to any control
group not receiving psychotherapy; and (4) provided
baseline information and post-intervention psycho-emotional
outcomes. One reviewer (MP) screened the
identified search results in a two-stage process, with a title
and abstract screening followed by a full-text screening. Studies that met all criteria were included in the review.
Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA) reporting guidelines were
implemented in the preparation of the manuscript.
Table 1. Ovid MEDLINE search strategy.
Data Extraction
Data extraction was completed independently by two
authors (MP and VR). Information extracted included
studies at baseline: country of origin, number of
participants in both the intervention and control groups,
age, education, type and duration of treatment for breast
cancer, as well as the type and duration of psychotherapy
received.
Data Analysis
Studies were divided into subgroups based on indications
for psychotherapy. For each included study, baseline
demographics and study endpoints were reported using
descriptive statistics. For continuous parameters, means
and standard deviations were reported where available,
while categorical variables were reported as proportions
of the study sample. Commercial software (Microsoft
Excel; Microsoft, Inc., Redmond [WA], United States)
was used to collect all data. Study statistics were
summarised, and a p value < 0.05 was used as a threshold
to establish statistical significance.
RESULTS
Study Inclusions and Baseline Characteristics
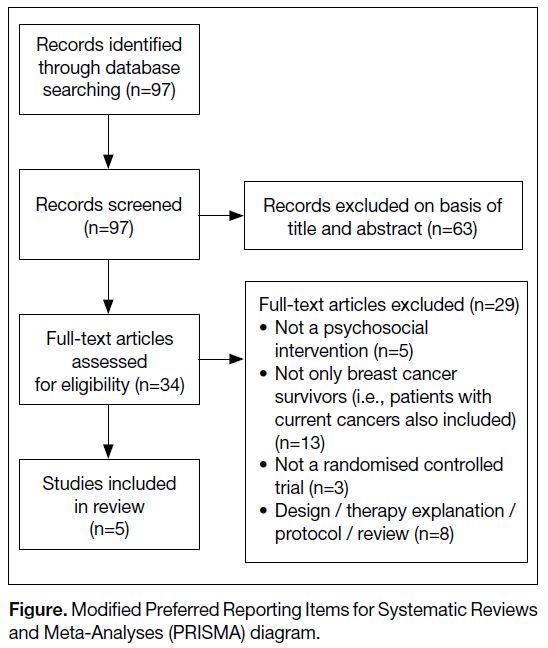
The database search revealed a total of 97 articles,
63 of which were excluded in title and abstract screening
(Figure). Twenty-nine articles were then excluded in the
full-text screening stage, leaving five studies with a total
of 838 participants at baseline and 719 at final follow-up.
[16] [17] [18] [19] [20]
Figure. Modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram.
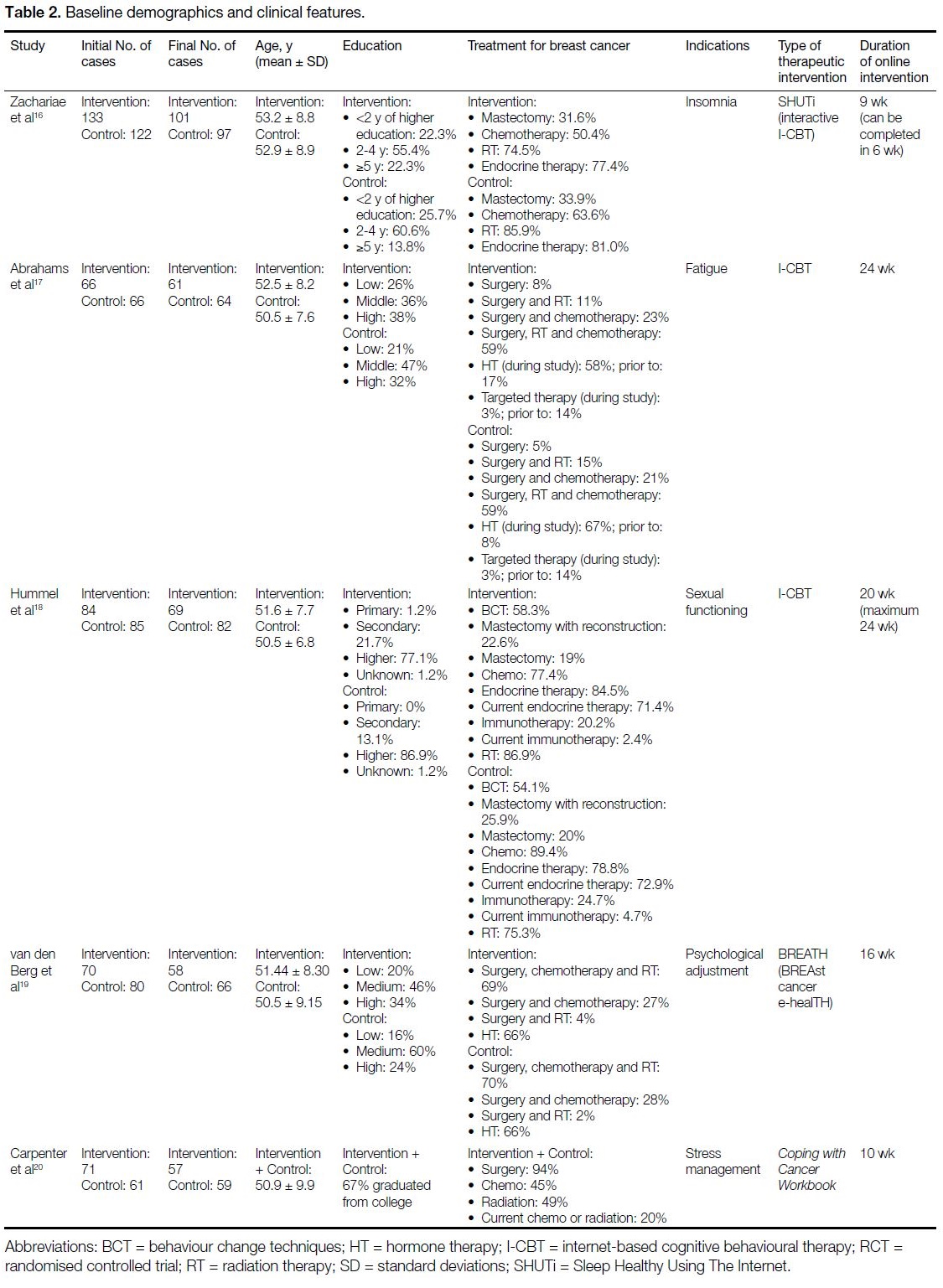
Baseline characteristics of participants and clinical
features of the online psychotherapies are shown in
Table 2. All five studies were RCTs.[16] [17] [18] [19] [20] Across the five
included studies, all participants were female and were
BCS. The mean age was 51.7 years (range = 50.2-56.9).
Education levels of the women varied, with most women
having completed some higher education. Treatments
that were received by participants included surgery,
chemotherapy, radiation therapy, endocrine/hormone
therapy, immunotherapy, or a combination of treatments
(Table 2). Stages of cancer included stage 0 to III,[16] [20]
stages I-III,[17] stages T1-T4,[18] and not specified.[19]
Patients that were not cancer-free, or that experienced
any recurrence, were removed from the study. Each
study specified diagnoses and/or treatment completion
timeframe for inclusion prior to recruitment. Online
psychotherapy ranged from 6 weeks[16] to 24 weeks,[17] with a mean duration of 15.1 weeks. The included studies
involved CBT[16] [17] [18] or incorporated certain properties of
CBT.[19] [20]
Table 2. Baseline demographics and clinical features.
Behavioural Indications
Zachariae et al[16] assessed internet-delivered CBT for
insomnia, which consisted of six cores which aimed
to improve patients’ sleep hygiene. Participants were
included in the study if they suffered from insomnia,
which was defined as a score >5 on the Pittsburgh Sleep
Quality Index (PSQI),[21] with higher scores representing
poorer sleep quality. They randomised 133 participants to
the intervention group and 122 participants to the control
group. The online therapy (SHUTi [Sleep Healthy Using
The Internet])[22] was interactive internet-delivered CBT
for insomnia (Table 2). SHUTi can be completed in
6 weeks, but participants were given 9 weeks to complete
the modules. Researchers performed a pre-assessment,
and a final follow-up 15 weeks later. Primary outcomes
were tested using the PSQI for sleep quality and using
the Insomnia Severity Index[23] for insomnia severity.
A secondary outcome, fatigue, was tested using the
FACIT-F (Functional Assessment of Chronic Illness
Therapy–Fatigue[24]). Baseline parameters between the
intervention and control groups were similar for all three
scales (p > 0.05). Following the intervention, a greater
proportion of participants in the intervention group
reported better sleep quality, lower insomnia severity
(p < 0.0001), and lower fatigue levels (p < 0.001)
compared to controls. The proportion of participants who
no longer met the criteria for PSQI >5 was much higher
for participants in the intervention arm as compared to
the control group (p = 0.011).
Abrahams et al[17] examined an eight-module online
CBT for severe fatigue in a sample of BCS in the
Netherlands. The sample consisted of 66 women in
the intervention group, and 66 women in usual care as
the control group. To be included in the study, patients
had to have significant fatigue based on a score of ≥35
on the Checklist Individual Strength–Fatigue Severity
subscale.[25] Participants initiated their internet-based
CBT (I-CBT) first with two in-person sessions with a
therapist, and then subsequent online sessions (Table 2).
Participants aimed to work on improving their fatigue
and related symptoms. At baseline, both groups were
well beyond the cut-off of 35 on the Checklist Individual
Strength–Fatigue Severity subscale, indicating severe
fatigue. After 6 months, scores of both groups decreased,
however, the women in the intervention group had
significantly lower levels of fatigue (mean difference: p < 0.0001). Similar improvements in functional
impairment (using the Sickness Impact Profile 8[26])
and psychological distress (using the Brief Symptom
Inventory 18[27]) were also demonstrated. Scores of both
groups were similar at baseline, however after 6 months,
a larger improvement was seen in the intervention
group, both for functional impairment and psychological
distress, with a significant mean difference (p < 0.0001).
In total, 73% of patients in the I-CBT group had
improved fatigue symptoms and/or severity, while only
28% women in the control group improved.[17]
Hummel et al[18] conducted a study in the Netherlands
looking at the efficacy of online psychotherapy for sexual
functioning in BCS. The intervention group consisted
of 84 women, while the control group consisted of 85
individuals. All women had to have a prior Diagnostic and
Statistical Manual of Mental Disorders Text Revision,
4th edition[28] diagnosis of sexual dysfunction. The
therapy was guided by one of four female psychologists/sexologists. The 10-module I-CBT was composed of
approximately 20 weekly sessions that were completed
in 24 weeks (Table 2). The goal of the intervention was
to improve sexual functioning, relationship intimacy
and body image. The primary outcome was based on
the Female Sexual Function Index,[29] which looked at
sexual functioning; higher scores indicate better sexual
functioning. The study also evaluated sexual pleasure via
the Sexual Activity Questionnaire Pleasure subscale,[30]
and sexual distress via the Female Sexual Distress Scale–Revised.[31] At pre-assessment, the intervention group was
similar to the control group on all three measures, while at
the post-assessment, sexual functioning, sexual pleasure,
and sexual distress were all significantly improved in
the intervention group compared to the control group
(p = 0.031, 0.001, and 0.002, respectively).[18]
Psychological Indications
van den Berg et al[19] examined the efficacy of online
therapy for BCS in the hopes of improving psychological
adjustment. Women were recruited to participate in this
RCT and were randomised either into a control group
(n=80) or an intervention group (n=70). The 16-week
online therapy, called BREATH,[32] used principles of
CBT to create this online self-management intervention
to help participants cope with survivorship (Table 2).
The two primary outcomes were general psychological
distress (tested by the Symptom Checklist 90)[33] and
psychological empowerment (assessed using the Cancer
Empowerment Questionnaire; CEQ).[34] At the baseline
assessment, both groups had similar mean scores on both measures. After controlling for baseline levels
of psychological distress, the intervention group had
significantly less psychological distress than the control
group (p < 0.05). However, while both groups showed a
slight improvement in the CEQ, there was no significant
difference between the scores of the two groups (p =
0.336; value adjusted for the baseline level). One of
the secondary outcomes tested was general negative
adjustment by the Hospital Anxiety and Depression
Scale[35] total score, where lower scores represent
improvement. At baseline, the intervention and control
groups had similar mean scores, while at follow-up,
those in the intervention group had significantly higher
scores than those in the control group when adjusting for
baseline Hospital Anxiety and Depression Scale score
(p < 0.05).[19]
Carpenter et al[20] conducted a study looking at the benefit
of an online workbook for stress management levels
in BCS. In total, 132 women agreed to participate in
the study (intervention group: 71; control group: 61).
Inclusion was determined by multiple indications of
distress. This pilot study helped determine the efficacy
of the online workbook Coping with Cancer Workbook,
which teaches participants coping strategies, and
relaxation management strategies through cognitive
and behaviourally based homework. This workbook is
typically completed in 10 weeks (Table 2). Two of the
primary outcomes tested were (1) self-efficacy for coping
with cancer, tested with the Cancer Behavior Inventory
v2.0[36]; and (2) self-efficacy for coping with negative
mood, assessed with the Negative Mood Regulation
Scale.[37] Finding benefit in the cancer experience was a
secondary outcome completed by the Benefit Finding
Scale (BFS).[38] Baseline measures were all reported as a
composite for all participants, regardless of intervention.
At follow-up, there was a significant difference for
self-efficacy for coping with cancer, with an increase
in the intervention group’s mean score compared to the
control group (p = 0.019). At follow-up, individuals in
the intervention group had significantly higher scores
than those in the control group for the Negative Mood
Regulation Scale (p = 0.007). For the BFS, there was no
significant improvement at follow-up for either group.[20]
DISCUSSION
The aim of this review was to assess published clinical
outcomes following online psychotherapy for BCS.
Overall, there were three studies (60%) that focused on
behavioural indications,[16] [17] [18] and two studies (40%) that
focused on psychological indications[19] [20] (Table 2). For the behavioural-based studies, one study treated patients
with insomnia,[16] one study focused on patients with
fatigue,[17] and one study examined sexual dysfunction.[18]
Of the psychological indications, one study focused
on psychological adjustment[19] and the other examined
stress management.[20]
Online interventions generally resulted in favourable
outcomes with a statistically significant reduction in
symptom severity following therapy. Of the 11 primary
outcomes assessed,[16] [17] [18] [19] [20] the scores of the women in the
intervention groups significantly improved on nine
scales, with associated effect sizes of 0.33[19] to 1.10[16] as
measured by Cohen’s d. Indications that improved were
insomnia,[16] sleep quality,[16] fatigue,[17] sexual functioning,[18]
sexual pleasure,[18] sexual distress,[18] general psychological
distress,[19] self-efficacy for coping with cancer,[20] and
self-efficacy for coping with negative mood.[20] One
primary outcome that was not significant was the CEQ,[19]
which measures how efficiently patients can derive
psychological empowerment from their interpersonal
and intrapersonal environments.[34] Also, there were no
differences seen between the control and intervention
groups on the BFS,[20] which evaluates one’s ability to find
positive outcomes from the cancer experience.[38] Among
the four secondary outcomes examined from three
different studies,[16] [17] [19] women in the intervention group
showed significant improvements on all four indications
(fatigue,[16] functional impairment,[17] psychological
distress,[17] and general negative adjustment[19]).
Traditionally, psychotherapies are used to diminish
bothersome symptoms.[39] As was demonstrated, the online
psychotherapies reviewed were able to decrease a variety
of psychosocial and behavioural symptoms. However,
whether this can be translated into clinically significant
outcomes is not well documented, especially since many
of the included scales do not have published estimates of
the minimal patient-important differences. As well, the
non-significant parameters should be investigated. Both
the CEQ and BFS are non-traditional measures, as they
measure strengths rather than weaknesses. It is possible
that there are smaller effect sizes associated with scales
that evaluate strengths, as opposed to those worded with
respect to reduction of symptoms.[19] For example, for
the primary outcomes, of the nine that were statistically
significant, seven dealt with a decrease of symptoms as
opposed to improving strengths.[16] [17] [18] [19]
The question still remains whether online therapy is
more beneficial than in-person therapy for BCS. Women often find face-to-face psychotherapy intimidating when
talking about sexual and intimate problems and are
more likely to opt out of these programmes than if the
psychotherapy is online.[40] Since sexual dysfunction is a
possible lingering symptom in BCS, online therapy may
be a more attractive alternative. In addition, due to the
harsh negative outcomes (e.g., hair loss, disfigurement,
weight loss, etc.) following cancer treatment[11] many
women may feel self-conscious.[18] They also may feel
too unwell to go out of the house to attend therapy,
leaving online therapy as a possible alternative. Overall,
the results indicate that online therapy for a variety of
symptoms in BCS is beneficial. Due to the unique nature
of a survivor’s life, it may even be more desirable than
traditional therapy.
Online therapies have not only been proven effective for
BCS, but also across other cancer populations, including
the reduction of post-traumatic stress symptoms in long-term
survivors of paediatric cancers[41] and the reduction
of psychological distress in men with prostate cancer.[42]
This invites a search for the benefits of online therapy
for other populations, especially given the present need
to physically distance during the coronavirus disease
2019 pandemic. During the pandemic lockdowns, most
in-person therapy services were either not running or
switched to an online format. Online psychotherapy
can alleviate time constraints, increase accessibility to a
more heterogeneous population,[43] reduce the stigma of
seeking therapy, and eliminate other barriers associated
with seeking therapy in person.[10] It is also perceived
as convenient and comfortable both by patients and by
clinicians.[10]
Despite the benefits presented, practical concerns and
challenges exist that hinder its use in routine practice.
First of all, patient privacy and confidentiality must
be considered. As is common practice for therapeutic
interventions, patients disclose personal information
continuously during therapy. Even though privacy
settings can be monitored, and data encryption solutions
can be employed, one needs to be wary that privacy
still cannot completely be guaranteed online.[10] [44] If one
is accessing online therapy to avoid the stigma of face-to-face appointments,[45] this privacy concern may impact
an individual’s decision to complete therapy online and
may prove to be counterintuitive. In addition, online
therapy is only feasible for individuals who can read,
write, and are proficient with technology. Those who
have poor literacy skills will have difficulty grasping
the knowledge that the therapy provides and hence are not likely to benefit from the programme. An individual
with poor technology skills or those from marginalised
backgrounds may not be able to access online therapy.
Certain techniques, such as body focusing, would be more
difficult to apply in the context of an online environment.
Finally, one practical concern may ensue with the use
of online therapy. How can one know whether there
is a congruency between behaviours, cognitions, and
emotions experienced in reality compared with what
the client reports online? It is possible that individuals
may report improvements that are not truly there, and
due to the limited non-verbal cues and facial expressions
from both parties, the therapist may have difficulties
being more certain that their intention was met and that
the client has shown improvements.[10] With the present
pandemic hindering accessibility to in-person services,
both clients and clinicians must carefully weigh the pros
and cons of online therapy to determine their comfort
with the proposed alternative.
Some limitations of the studies included in this review
should be considered. First, given the relatively short
duration of follow-up, compared to the survivorship
journey, it is unclear whether the demonstrated
improvement at post-intervention assessment could
lead to the long-term remission of their psychiatric
co-morbidities and symptoms. It is thus plausible that
women continue to have subclinical symptoms that are
still present or may later recur. The psychotherapies
presented in the review were typically focused on a
specific symptom (e.g., fatigue, sexuality). As such, it is
possible that women enrolled in these programmes had
multiple psychological comorbidities (e.g., as suggested
by Lee et al[12]), some of which were unaddressed by the
specific intervention they were receiving. In the future,
researchers should investigate the potential of a holistic
care approach, focusing on a comprehensive model
of change, as opposed to specific symptomology.[46]
Also, the types of treatments included in the studies
had different treatment protocols, including duration,
number, and type of modules, symptoms addressed, and
extent of therapist-guidance (Table 2). For example,
Abrahams et al[17] began their procedure with three
face-to-face sessions, while the other four studies had
no in-person therapist contact. This makes it difficult
to identify the optimal interventional model through
indirect comparisons across studies. Another limitation
relates to the online nature of the therapy. Based on
literature estimates, most BCS are aged 60 to 75 years.[17]
Across all five studies, the mean age was 51.7 years.[16] [17] [18] [19] [20]
This might suggest that online psychotherapies attract younger women on average and may be less appealing
to or practical for older BCS given the necessity
for technological proficiency. Moreover, it is well-established
that individuals with higher socioeconomic
status have better overall health.[30] Since individuals of
high SES are more likely to have access to technology
and have superior health outcomes than those of low
socioeconomic status, this might overestimate the true
efficacy of online psychotherapy treatments.[47]
Alongside the limitations of the studies included in this
review, there are also limitations of the present study.
Only RCTs were included in this paper. Although
this improved the internal validity of the study, while
decreasing the effects of confounding, this has the
potential to limit generalisability. As described above, this
review is heterogenous, including studies with diverse
treatment protocols (e.g., session duration) and varying
indicators. Although this may serve as a benefit for some
studies, due to the small number of studies included in
this review, it is more of a hinderance. The heterogeneity
of the studies, combined with a small sample size, yields a
review paper that must be interpreted with caution. These
two limitations are reflective of the lack of literature on
the topic. Future studies should continue to investigate
the efficacy of online therapy for BCS who are struggling
with behavioural, psychological, or social symptoms.
Once enough studies are compiled, it is suggested that
larger reviews and/or meta-analyses are conducted. By
conducting these larger reviews, future research will be
able to make better sense of the outcomes, without being
swayed by high variability.
CONCLUSION
Individuals who have recovered from breast cancer often
have residual behavioural, physical, or social symptoms
from the cancer experience.[12] Due to these problems,
BCS may be a population that may particularly benefit
from online psychotherapy. The purpose of this review
was to investigate whether online psychotherapy is
effective for the behavioural and psychological sequelae
of BCS. This study found support for improving
behavioural (e.g., insomnia) and psychological (e.g.,
stress management) symptomology using an online
psychotherapeutic paradigm.[16] [17] [18] [19] [20] All five studies
included in the review were based on CBT, suggesting
that this type of therapy may be particularly useful
within the BCS population. Although the conclusions
of this review are encouraging, limitations must be
considered. This review is highly heterogenous and
has a small sample size. As such, the generalisability of this study may be limited. More controlled research
must be done in this setting. Once enough literature
exists, researchers are encouraged to evaluate the studies
comprehensively using meta-analytic or other systematic
review methodologies.
REFERENCES
1. Cuijpers P, Karyotaki E, Reijnders M, Huibers MJ. Who benefits from psychotherapies for adult depression? A meta-analytic update of the evidence. Cogn Behav Ther. 2018;47:91-106. Crossref
2. Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, et al.
Comparative efficacy of seven psychotherapeutic interventions
for patients with depression: a network meta-analysis. PLoS Med.
2013;10:e1001454. Crossref
3. Smith GC. Psychotherapy. In: Fink G, editor. Encyclopedia of
Stress. 2nd ed. Amsterdam: Elsevier Press; 2007. p 302-7. Crossref
4. Cuijpers P, Andersson G, Donker T, van Straten A. Psychological
treatment of depression: results of a series of meta-analyses. Nord
J Psychiatry. 2011;65:354-64. Crossref
5. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer
J Clin. 2019;69:7-34. Crossref
6. Saeedi B, Khoshnood Z, Dehghan M, Abazari F, Saeedi A. The
effect of positive psychotherapy on the meaning of life in patients
with cancer: a randomized clinical trial. Indian J Palliat Care.
2019;25:210-7. Crossref
7. van Eenbergen MC, van den Hurk C, Mols F, van de Poll-Franse LV.
Usability of an online application for reporting the burden of side
effects in cancer patients. Support Care Cancer. 2019;27:3411-9. Crossref
8. Breitbart W, Pessin H, Rosenfeld B, Applebaum AJ, Lichtenthal
WG, Li Y, et al. Individual meaning-centered psychotherapy
for the treatment of psychological and existential distress: a
randomized controlled trial in patients with advanced cancer.
Cancer. 2018;124:3231-9. Crossref
9. Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation
of videoconferencing-based approaches. World J Psychiatry.
2015;5:286-304 Crossref
10. Stoll J, Müller JA, Trachsel M. Ethical issues in online
psychotherapy: a narrative review. Front Psychiatry. 2020;10:993. Crossref
11. Cheung EO, Cohn MA, Dunn LB, Melisko ME, Morgan S,
Penedo FJ, et al. A randomized pilot trial of a positive affect skill
intervention (lessons in linking affect and coping) for women with
metastatic breast cancer. Psychooncology. 2017;26:2101-8. Crossref
12. Lee L, Ross A, Griffith K, Jensen RE, Wallen GR. Symptom
clusters in breast cancer survivors: a latent class profile analysis.
Oncol Nurs Forum. 2020;47:89-100. Crossref
13. Mitchell AJ. New developments in the detection and treatment of
depression in cancer settings. Prog Neurol Psychiatry. 2011;15:12-20. Crossref
14. Semin JN, Palm D, Smith LM, Ruttle S. Understanding breast
cancer survivors’ financial burden and distress after financial
assistance. Support Care Cancer. 2020;28:4241-8. Crossref
15. Simard S, Thewes B, Humphris G, Dixon M, Hayden C,
Mireskandari S, et al. Fear of cancer recurrence in adult cancer
survivors: a systematic review of quantitative studies. J Cancer
Surviv. 2013;7:300-22. Crossref
16. Zachariae R, Amidi A, Damholdt MF, Clausen CD, Dahlgaard J,
Lord H, et al. Internet-delivered cognitive-behavioral therapy for
insomnia in breast cancer survivors: a randomized controlled trial.
J Natl Cancer Inst. 2018;110:880-7. Crossref
17. Abrahams HJ, Gielissen MF, Donders RR, Goedendorp MM,
van der Wouw AJ, Verhagen CA, et al. The efficacy of internet-based
cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: a randomized
controlled trial. Cancer. 2017;123:3825-34. Crossref
18. Hummel SB, van Lankveld JJ, Oldenburg HS, Hahn DE,
Kieffer JM, Gerritsma MA, et al. Efficacy of internet-based
cognitive behavioral therapy in improving sexual functioning of
breast cancer survivors: results of a randomized controlled trial. J
Clin Oncol. 2017;35:1328-40. Crossref
19. van den Berg SW, Gielissen MF, Custers JA, van der Graaf WT,
Ottevanger PB, Prins JB. BREATH: web-based self-management
for psychological adjustment after primary breast cancer-results
of a multicenter randomized controlled trial. J Clin Oncol.
2015;33:2763-71. Crossref
20. Carpenter KM, Stoner SA, Schmitz K, McGregor BA, Doorenbos AZ. An online stress management workbook for breast
cancer. J Behav Med. 2014;37:458-68. Crossref
21. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The
Pittsburgh Sleep Quality Index: a new instrument for psychiatric
practice and research. Psych Res. 1989;28:193-213. Crossref
22. Ritterband LM, Bailey ET, Thorndike FP, Lord HR,
Farrell-Carnahan L, Baum LD. Initial evaluation of an Internet
intervention to improve the sleep of cancer survivors with insomnia.
Psychooncology. 2012;21:695-705. Crossref
23. Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia
Severity Index as an outcome measure for insomnia research. Sleep
Med. 2001;2:297-307. Crossref
24. Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E.
Measuring fatigue and other anemia-related symptoms with the
Functional Assessment of Cancer Therapy (FACT) measurement
system. J Pain Symptom Manage. 1997;13:63-74. Crossref
25. Vercoulen J, Alberts M, Bleijenberg G. De Checklist Individual
Strength (CIS) [in Dutch]. Gedragstherapie. 1999;32:131-6.
26. Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness
Impact Profile: development and final revision of a health status
measure. Med Care. 1981;19:787-805. Crossref
27. Derogatis LR. BSI 18, Brief Symptom Inventory 18: Administration,
Scoring and Procedures Manual. NCS Pearson, Inc.; 2001. Crossref
28. American Psychiatric Association. Diagnostic and Statistical
Manual of Mental Disorders: DSM-IV-TR. Washington D.C.:
American Psychiatric Association; 2011.
29. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R,
et al. The Female Sexual Function Index (FSFI): a multidimensional
self-report instrument for the assessment of female sexual function.
J Sex Marital Ther. 2000;26:191-208. Crossref
30. Thirlaway K, Fallowfield L, Cuzick J. The Sexual Activity
Questionnaire: a measure of women’s sexual functioning. Qual
Life Res. 1996;5:81-90. Crossref
31. Derogatis LR, Rosen R, Leiblum S, Burnett A, Heiman J. The
Female Sexual Distress Scale (FSDS): Initial validation of a
standardized scale for assessment of sexually related personal
distress in women. J Sex Marital Ther. 2002;28:317-30. Crossref
32. van den Berg SW, Gielissen MF, Ottevanger PB, Prins JB.
Rationale of the BREAst cancer e-healTH (BREATH) multicentre
randomised controlled trial: an internet-based self-management
intervention to foster adjustment after curative breast cancer by
decreasing distress and increasing empowerment. BMC Cancer.
2012;12:394. Crossref
33. Schauenburg H, Strack M. Measuring psychotherapeutic change
with the symptom checklist SCL 90 R. Psychother Psychosom.
1999;68:199-206. Crossref
34. van den Berg SW, van Amstel FK, Ottevanger PB, Gielissen MF,
Prins JB. The Cancer Empowerment Questionnaire: Psychological
empowerment in breast cancer survivors. J Psychosoc Oncol.
2013;31:565-83. Crossref
35. Vodermaier A, Millman RD. Accuracy of the Hospital Anxiety and
Depression Scale as a screening tool in cancer patients: a systematic
review and meta-analysis. Support Care Cancer. 2011;19:1899-908. Crossref
36. Merluzzi TV, Nairn RC, Hegde K, Martinez Sanchez MA, Dunn L.
Self-efficacy for coping with cancer: revision of the Cancer
Behavior Inventory (version 2.0). Psychooncology. 2001;10:206-17. Crossref
37. Catanzaro SJ, Mearns J. Measuring generalized expectancies
for negative mood regulation: initial scale development and
implications. J Pers Assess. 1990;54:546-63. Crossref
38. Carver CS, Antoni MH. Finding benefit in breast cancer during the
year after diagnosis predicts better adjustment 5 to 8 years after
diagnosis. Health Psychology. 2004;23:595-8. Crossref
39. Priebe S, Omer S, Giacco D, Slade M. Resource-oriented therapeutic models in psychiatry: conceptual review. Br J Psychiatry. 2014;204:256-61. Crossref
40. Hummel SB, van Lankveld JJ, Oldenburg HS, Hahn DE,
Broomans E, Aaronson NK. Internet-based cognitive behavioral
therapy for sexual dysfunctions in women treated for breast cancer:
design of a multicenter, randomized controlled trial. BMC Cancer.
2015;15:321. Crossref
41. Seitz DC, Knaevelsrud C, Duran G, Waadt S, Loos S, Goldbeck L. Efficacy of an internet-based cognitive-behavioral intervention for
long-term survivors of pediatric cancer: a pilot study. Support Care
Cancer. 2014;22:2075-83. Crossref
42. Wootten AC, Abbott JA, Meyer D, Chisholm K, Austin DW,
Klein B, et al. Preliminary results of a randomised controlled trial
of an online psychological intervention to reduce distress in men
treated for localised prostate cancer. Eur Urol. 2015;68:471-9. Crossref
43. Cartreine JA, Ahern DK, Locke SE. A roadmap to computer-based
psychotherapy in the United States. Harv Rev Psychiatry.
2010;18:80-95. Crossref
44. Taylor CB, Luce KH. Computer- and internet-based psychotherapy
interventions. Curr Dir Psychol Sci. 2003;12:18-22. Crossref
45. Thomas A, Grandner M, Nowakowski S, Nesom G, Corbitt C,
Perlis ML. Where are the behavioral sleep medicine providers and
where are they needed? A geographic assessment. Behav Sleep
Med. 2016;14:687-98. Crossref
46. Zamanzadeh V, Jasemi M, Valizadeh L, Keogh B, Taleghani F.
Effective factors in providing holistic care: a qualitative study.
Indian J Palliat Care. 2015;21:214-24. Crossref
47. Adler NE, Snibbe AC. The role of psychosocial processes in
explaining the gradient between socioeconomic status and health.
Curr Dir Psychol Sci. 2003;12:119-23. Crossref