Image-guided Localisation of Nonpalpable Breast Lesions: a Comparative Analysis of Magnetic Seeds and Hookwires in an Asian Population
ORIHINAL ARTICLE
Image-guided Localisation of Nonpalpable Breast Lesions: a Comparative Analysis of Magnetic Seeds and Hookwires in an
Asian Population
S Yang, YT Wong, PW Leong, AOC Li, KY Kwok, DLY Chow, AYT Lai
Department of Radiology, Tuen Mun Hospital, Pok Oi Hospital, Hong Kong
Correspondence: Dr S Yang, Department of Radiology, Tuen Mun Hospital, Pok Oi Hospital, Hong Kong. Email: chloe.sy.yeung@gmail.com
Submitted: 6 Jul 2021; Accepted: 24 Aug 2021.
Contributors: SY, PWL and AYTL designed the study. SY and YTW acquired the data. All authors analysed the data. SY drafted the manuscript.
SY, PWL, AOCL, KYK, DLYC and AYTL critically revised the manuscript for important intellectual content. All authors had full access to the
data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This retrospective study was approved by the New Territories West Cluster Research Ethics Committee (NTWC/REC/21020). The requirement to obtain written informed consent was waived.
Abstract
Objectives
To compare the procedural outcomes of magnetic seed localisation and hookwire localisation (HWL)
of nonpalpable breast lesions in an Asian population.
Methods
We performed a retrospective review of 91 nonrandomised female patients who underwent breast surgery
after image-guided magnetic seed localisation or HWL from July 2019 to June 2021. Rates of placement success
(defined as marker-lesion distance <10 mm), lesion detection, marker retrieval, and complications, were compared.
Results
A total of 48 patients received magnetic seeds, and 43 patients received hookwires for preoperative
localisation; a total of 100 lesions (50/100, 50.0% Magseed vs. 50/100, 50.0% hookwire) were marked and excised.
Magnetic seeds were placed 0 to 126 days before surgery (median=14); of the 50 lesions marked, 22 were removed
on the same day and 28 on a later day. Placement success was identical between the two groups, 98.0% magnetic
seeds versus 98.0% hookwire. All lesions were detected at the first operation and successfully excised; all markers
were removed intact without complications.
Conclusion
Magnetic seed localisation demonstrated comparable procedural success and safety to conventional
HWL in Asian patients with thinner and denser breasts. It could be an effective alternative to HWL, with the additional
advantage of decoupling localisation and surgery dates.
Key Words: Breast; Carcinoma; Diagnostic imaging; Neoplasms
中文摘要
亞洲人群隱匿性乳腺病變的影像學引導定位:磁性粒子和金屬線比較分析
楊思悅、黃于庭、梁宝卉、李安慈、郭欣、周朗妍、黎爾德
目的
比較亞洲人群隱匿性乳腺病變的磁性粒子定位和金屬線定位的手術結果。
方法
我們2019年7月至2021年6月期間,對影像學引導下磁性粒子定位或金屬線定位後接受乳腺手術的91名非隨機女性患者進行回顧性分析。比較放置成功率(即標記與病灶距離10 mm以下)、病灶檢出率、標記物回取率和併發症率。
結果
48例患者接受磁性粒子術前定位,43例患者接受金屬線術前定位;標記並切除共100個病灶(磁粒子和金屬線各佔50個)。磁性粒子在術前0至126天放置(中位數14天);在標記的50個病灶中,22個在同一天進行切除,其餘28個在下一天進行切除。兩組的標記成功率相同,均達98.0%。所有病灶均在第一次手術中發現並成功切除;所有標記物都被完整取回和無併發症。
結論
與傳統金屬線定位比較,磁性粒子定位於亞洲乳房較薄和較緻密患者的手術成功率和安全性相若。它可能是金屬線定位的一個有效替代方法,具有分開病灶定位和手術期的額外優勢。
INTRODUCTION
Accurate preoperative localisation is key to successful
surgical excision of nonpalpable breast lesions.
Conventional image-guided hookwire localisation
(HWL) has been the most commonly used method for
decades, owing to its advantages of high accuracy and
cost-effectiveness.[1] However, it has several drawbacks,
including patient discomfort, potential wire transection,
dislocation, and migration due to its protruding external
portion.[2] Moreover, because HWL must be performed
on the day of surgery, close coordination between
surgery and radiology schedules is necessary. In order
to uncouple localisation and surgery times, alternative
non-wire localisation techniques have subsequently
been developed. In 1999, Luini et al[3] first reported on
99mTc-labelled colloidal albumin-guided occult lesion
localisation that can be performed up to 1 day before
surgery. In 2001, Gray et al[4] introduced radioactive seed
localisation as an effective alternative to wire localisation,
and this can be performed up to 5 days before surgery.
These techniques have been shown to be non-inferior to
HWL.[5] [6] [7] [8]
Magnetic seed markers (Magseed; Endomagnetics,
Cambridge, United Kingdom) can be deployed in target
lesions under mammographic or ultrasound guidance.[9]
The advantages of this technique include improved
patient experience and mitigation of the risks of wire transection and dislodgment due to the elimination of the
external wire component. Radiologists and surgeons can
choose the best entry site independently, which can offer
better cosmetic outcomes. It also provides a logistical
advantage by allowing scheduling flexibility. However,
this technique also comes with limitations. The Magseed
marker cannot be repositioned once deployed and causes
susceptibility artefacts on magnetic resonance imaging.[9]
The detectability of the marker is limited by the depth of
placement from the skin, and special non-ferromagnetic
surgical instruments are required to prevent interference
with the signal generated by the Magseed probe in the
operating room.[10] [11]
Several studies on Magseed localisation have
demonstrated satisfactory efficacy and safety in
Western populations.[12] [13] [14] However, the evidence is still
limited in Asian populations, where the breast tissue
is generally denser and thinner. Direct comparison
between the traditional HWL and Magseed localisation
has been rare.[15] To the best of our knowledge, no such
comparison has been conducted on an Asian population.
Non-wire localisation techniques such as Magseed
localisation have been invaluable in view of these
logistical constraints. The aim of the present study was
to assess the procedural success and safety of Magseed
localisation compared with conventional HWL in an
Asian population.
METHODS
Study Design and Patient Population
This was a single-institution retrospective review
of all symptomatic female patients who underwent
preoperative image-guided localisation of nonpalpable
breast lesions by either Magseed or hookwire from July
2019 to June 2021. A total of 91 cases with 100 lesions
were included. The age ranged from 29 to 82 years.
Cases including same-day and decoupled diagnostic
excisional biopsies and therapeutic wide local excisions
were performed by specialised breast surgeons.
The STROBE reporting guideline was implemented in
the preparation of the manuscript.
Localisation Technique
The choice between Magseed localisation or HWL was
based on clinical and radiological discussions, taking into
account lesion location and scheduling practicability.
All localisation procedures were conducted by breast
radiologists with ≥8 years of experience in breast imaging
under ultrasound or stereotactic guidance; the imaging
modality was chosen based on the nature of the lesions.
Hookwires were placed on the day of surgery. The wire
was preloaded into a 20-gauge needle. The insertion site
was decided by the operating radiologist, and depended
on multiple factors, including lesion position and
conspicuity on imaging; usually the shortest path from
skin to the lesion was chosen. Magseed is a paramagnetic
stainless steel pellet containing nickel and measures
5 mm × 1 mm. It becomes detectable by generating a
signal when it is temporarily magnetised by a probe
(Sentimag; Endomagnetics) that emits an alternating
magnetic field. It is preloaded in an 18-gauge needle and
can be placed in a lesion at a depth of up to 3 cm from
the skin surface. Magseed localisation was performed
either in advance or on the day of surgery, depending on
scheduling. Seeds were intraoperatively detected by the
surgeon using Sentimag. Audible and visible numeric
feedback from the detector provided real-time guidance
for the surgeon to locate and excise the lesion.
On the day of localisation, the distance between the
marker and lesion and the distance between the marker
and skin were recorded. These were measured on the
modality under which markers were placed. Placement
success was defined as a shortest marker-lesion distance
of <10 mm in all planes. Post-deployment mammograms
in both mediolateral and craniocaudal views were
obtained for all cases to establish marker location. If significant Magseed or hookwire migration of >10 mm
was observed, the breast radiologist would communicate
with the operating surgeon, and an additional hookwire
would be inserted to re-localise the lesion.
A specimen radiograph and/or ultrasound image was
acquired immediately after surgery to confirm the
retrieval of marker and excision of the lesion.
Data Collection
Clinical information, surgical records, and pathology
reports were retrieved from the electronic patient record
system. Radiological reports, images, and relevant data
were reviewed and recorded from PACS, including breast
density based on BI-RADS (breast imaging reporting
and data system), breast thickness on mammograms
in both mediolateral and craniocaudal views, imaging
modality used for localisation, nature of lesion, size of
lesion measured on ultrasound if visible, marker-lesion
distance on post-deployment mammogram or ultrasound
and on specimen radiograph or ultrasound, marker-skin
distance on post-deployment mammogram or ultrasound,
and complications.
Statistical Analysis
Data are presented as frequency (%) for ordinal or
categorical variables, mean ± standard deviation for
normally distributed variables, and median (interquartile
range [IQR]) for non-normally distributed variables.
A normality test was conducted for all quantitative
variables to test the distribution. Two independent
groups of Magseed localisation (Magseed group) and
HWL (hookwire group) were analysed for statistically
significant differences. The independent-sample t test
was used to compare normally distributed variables,
the Mann-Whitney U test for non-normally distributed
variables, the Kruskal–Wallis H test for ordinal
variables, and the Chi-squared test or Fisher’s exact test
for categorical variables. All statistical analyses were
performed using SPSS (Windows version 27.0; IBM
Corp, Armonk [NY], United States) with two-tailed tests
and a significance level of 0.05.
RESULTS
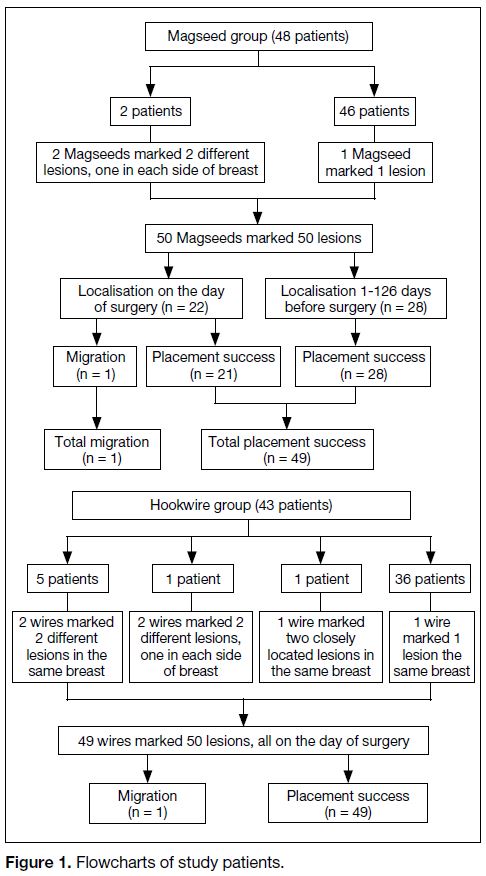
All 91 cases with 100 lesions underwent localisation
using 99 markers. Forty-eight (52.7%) cases with 50
lesions required 50 Magseeds, and 43 (47.3%) cases with
50 lesions required 49 hookwires. Magseeds were placed
0 to 126 days before surgery (median=14, IQR=0-35).
Of the 50 lesions marked by Magseed, 22 (44.0%) were
surgically removed the same day and 28 (56.0%) on a later day. Flow charts of study patients are shown in
Figure 1.
Figure 1. Flowcharts of study patients.
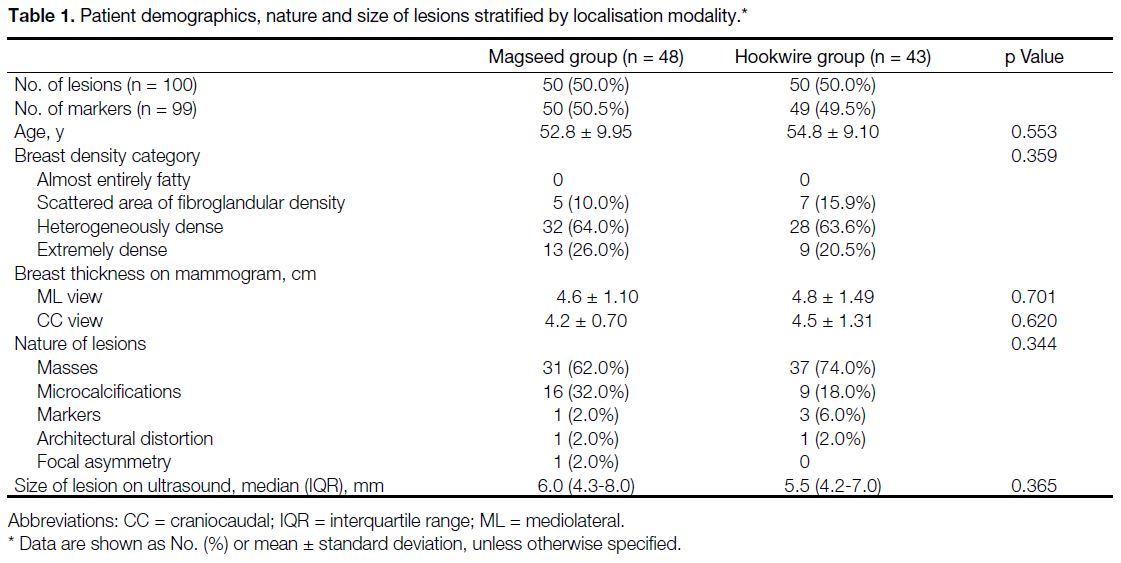
Age (52.8 ± 9.95 years Magseed vs. 54.8 ± 9.10 years
hookwire, p=0.553) and breast thickness (mediolateral
view: 4.6 ± 1.10 cm Magseed vs. 4.8 ± 1.49 cm hookwire,
p=0.701; craniocaudal view: 4.2 ± 0.70 cm Magseed vs.
4.5 ± 1.31 cm hookwire, p=0.620) of both groups showed
no statistically significant difference. Most of the breast
tissue was heterogeneously dense or extremely dense
(heterogeneously dense: 64.0% Magseed vs. 63.6%
hookwire; extremely dense: 26.0% Magseed vs. 20.5%
hookwire); there were only five (10.0%) and seven
(15.9%) breasts of scattered fibroglandular density in the
Magseed and hookwire groups, respectively, and there
was no breast tissue composed of almost entirely fat in
either group (p=0.359) [Table 1].
Table 1. Patient demographics, nature and size of lesions stratified by localisation modality.
Masses were the most common lesions (62.0% Magseed
vs. 74.0% hookwire), followed by microcalcifications
(32.0% Magseed vs. 18.0% hookwire), biopsy markers
(2.0% Magseed vs. 6.0% hookwire), architectural
distortion (2.0% Magseed vs. 2.0% hookwire) and focal
asymmetry (2.0% Magseed vs. 0% hookwire). There
was no statistically significant difference in the nature
of lesion localised for surgery between the two groups
(p=0.344). The size of lesions recorded on ultrasound
was also statistically comparable in the two groups
(median=6.0, IQR=4.3-8.0 for Magseed vs. median=5.5,
IQR=4.2-7.0 for hookwire; p=0.365) [Table 1].
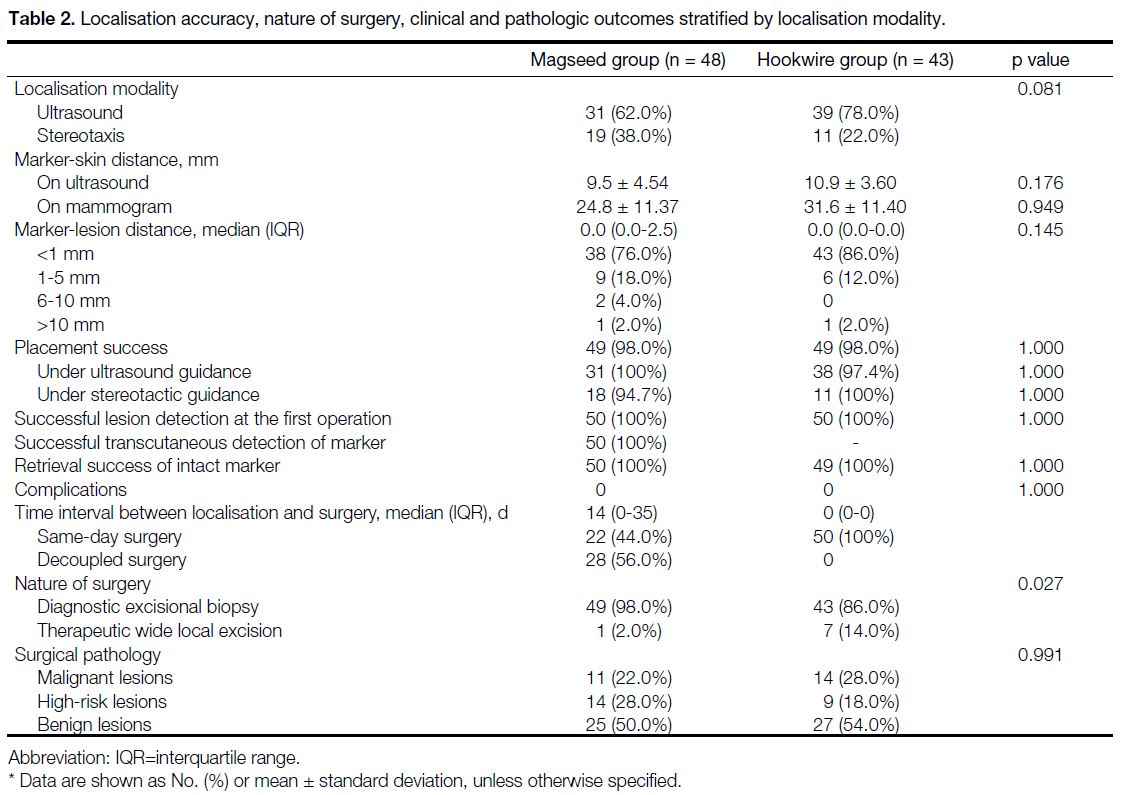
In most cases in both groups, ultrasound was the imaging
modality used for localisation. Under ultrasound
guidance, 62.0% and 78.0% of lesions were marked by
Magseed and hookwire, respectively. The rest of the
lesions were marked under stereotactic guidance. The
modality used for localisation showed no statistically
significant difference between the two groups (p=0.081)
[Table 2].
Table 2. Localisation accuracy, nature of surgery, clinical and pathologic outcomes stratified by localisation modality.
The distance between marker and skin, if inserted
under ultrasound guidance, ranged from 2 to 18 mm
(9.5 ± 4.54) for the Magseed group, and 2 to 19 mm
(10.9 ± 3.60) for the hookwire group; if inserted under
stereotactic guidance, ranged from 9 to 52 mm (24.8 ±
11.37) for the Magseed group and 13 to 54 mm (31.6 ±
11.40) for the hookwire group. Depth of the marker from
the skin was statistically similar between the two groups
(p=0.176 ultrasound guidance, p=0.949 stereotactic
guidance) [Table 2].
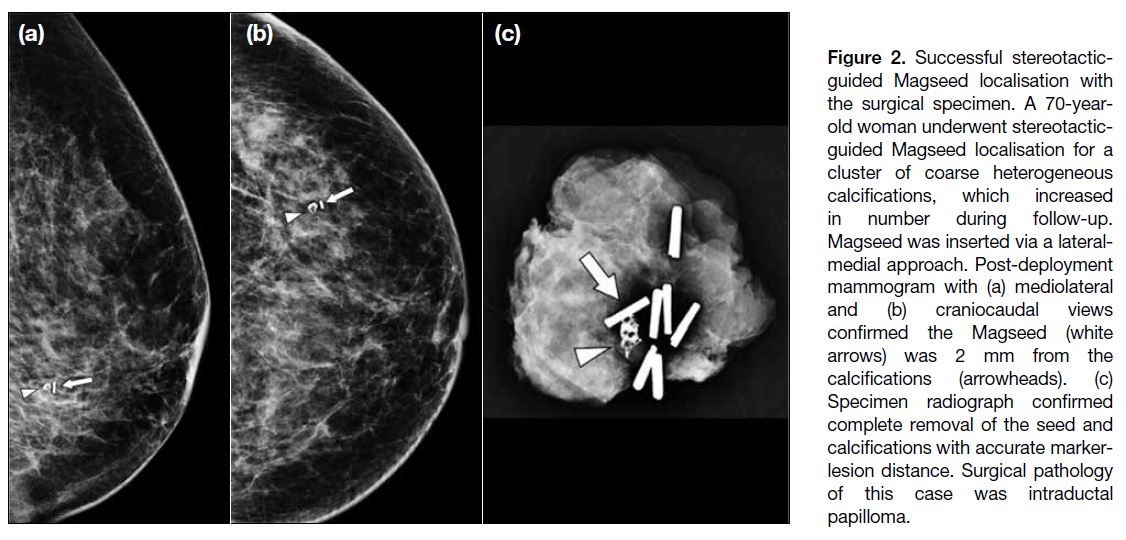
The rate of placement success was statistically
comparable between the two groups (98.0% Magseed vs.
98.0% hookwire; p=1.000), under both ultrasound (100%
Magseed vs. 97.4% hookwire, p=1.000) and stereotactic
guidance (94.7% Magseed vs. 100% hookwire, p=1.000)
[Table 2]. Examples of successful Magseed localisation
are illustrated in Figures 2 and 3. The only incidence of
hookwire migration involved a mass that was localised
under ultrasonic guidance. The wire was noted to have
been displaced at the post-insertion mammogram. An
additional wire was placed to re-localise the lesion. The
only migrated Magseed was deployed under stereotactic
guidance, which was coupled with a same-day surgery. A
subsequent salvage hookwire was placed, and the lesion
was then successfully excised (Figure 4). Performance
of localisation accuracy and clinical outcomes are
summarised in Table 2.
Figure 2. Successful stereotactic-guided Magseed localisation with the surgical specimen. A 70-year-old woman underwent stereotactic-guided Magseed localisation for a cluster of coarse heterogeneous calcifications, which increased in number during follow-up. Magseed was inserted via a lateral-medial approach. Post-deployment mammogram with (a) mediolateral and (b) craniocaudal views confirmed the Magseed (white arrows) was 2 mm from the calcifications (arrowheads). (c) Specimen radiograph confirmed complete removal of the seed and calcifications with accurate marker-lesion distance. Surgical pathology of this case was intraductal papilloma.
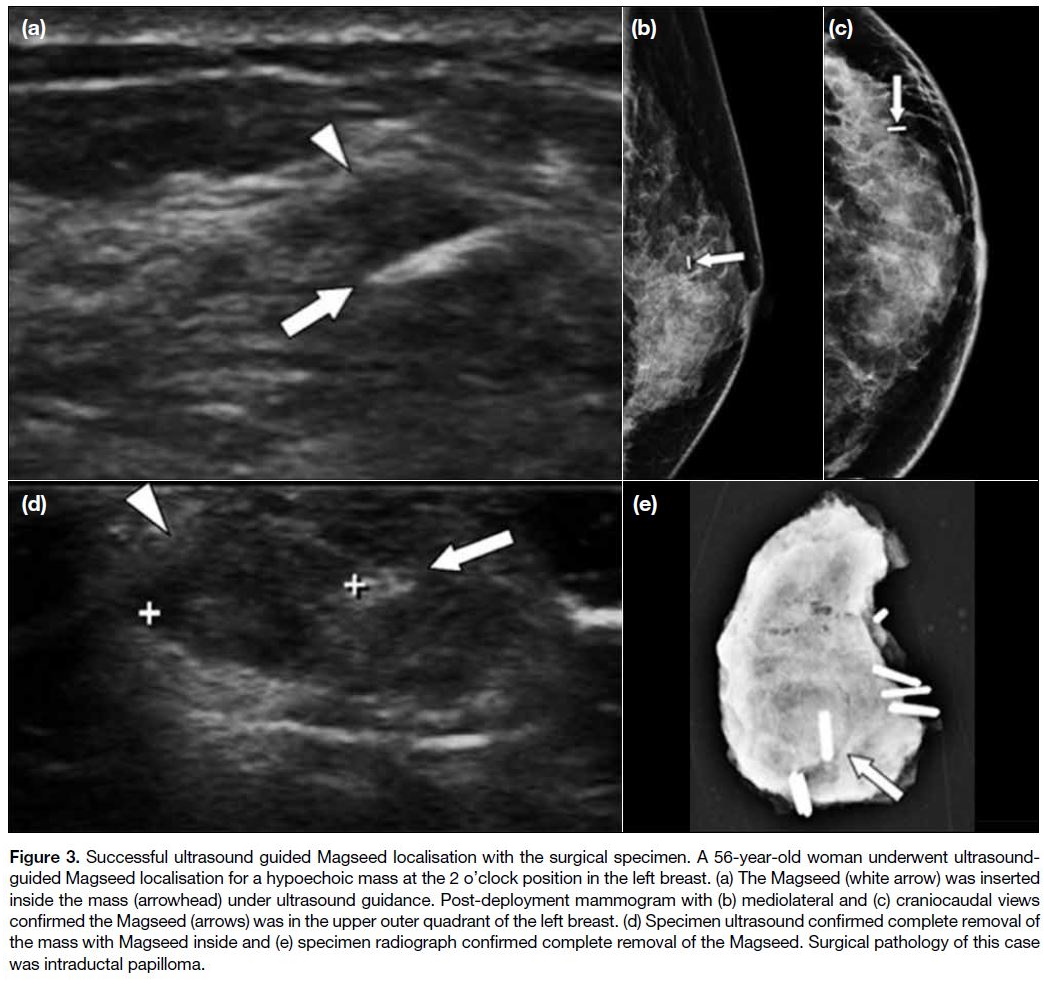
Figure 3. Successful ultrasound guided Magseed localisation with the surgical specimen. A 56-year-old woman underwent ultrasound-guided
Magseed localisation for a hypoechoic mass at the 2 o’clock position in the left breast. (a) The Magseed (white arrow) was inserted
inside the mass (arrowhead) under ultrasound guidance. Post-deployment mammogram with (b) mediolateral and (c) craniocaudal views
confirmed the Magseed (arrows) was in the upper outer quadrant of the left breast. (d) Specimen ultrasound confirmed complete removal of
the mass with Magseed inside and (e) specimen radiograph confirmed complete removal of the Magseed. Surgical pathology of this case
was intraductal papilloma.
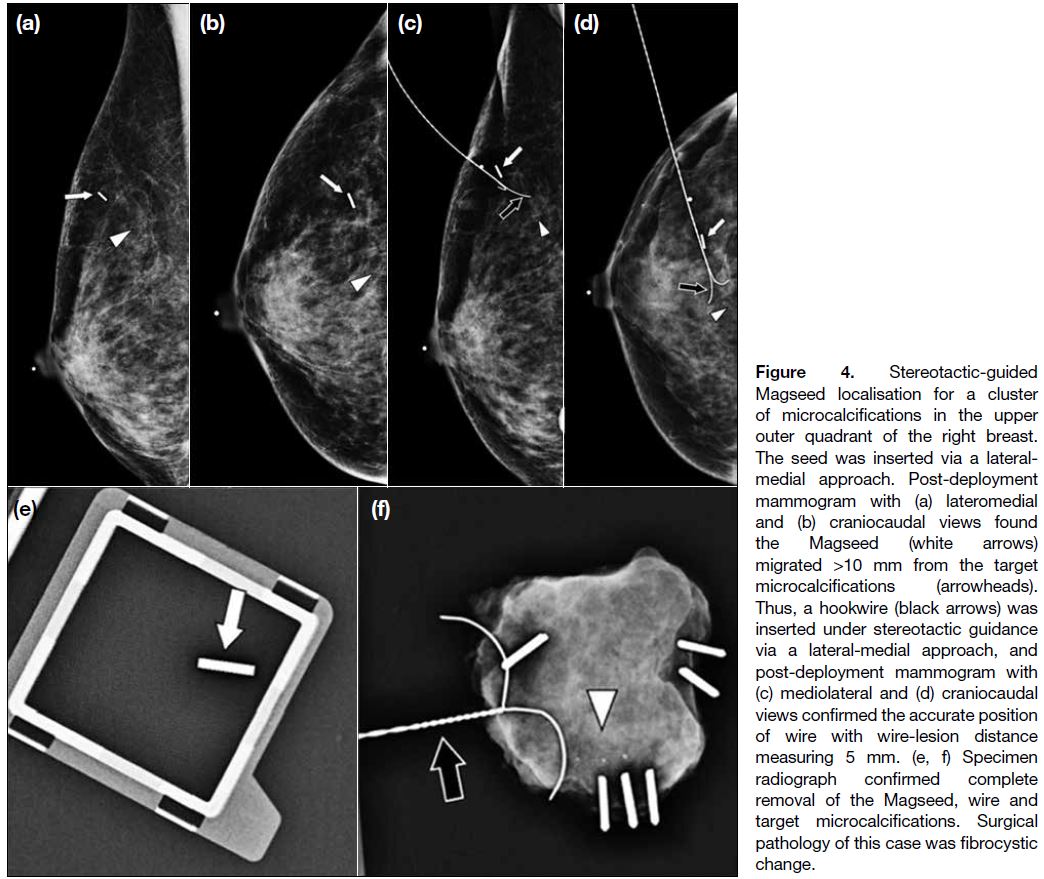
Figure 4. Stereotactic-guided Magseed localisation for a cluster of microcalcifications in the upper outer quadrant of the right breast. The seed was inserted via a lateral-medial approach. Post-deployment mammogram with (a) lateromedial and (b) craniocaudal views found the Magseed (white arrows) migrated >10 mm from the target microcalcifications (arrowheads). Thus, a hookwire (black arrows) was inserted under stereotactic guidance via a lateral-medial approach, and post-deployment mammogram with (c) mediolateral and (d) craniocaudal views confirmed the accurate position of wire with wire-lesion distance measuring 5 mm. (e, f) Specimen radiograph confirmed complete removal of the Magseed, wire and target microcalcifications. Surgical pathology of this case was fibrocystic change.
Both groups had more excisional biopsies than wide local
excision (Magseed: 98.0% vs. 2.0%; hookwire: 86.0%
vs. 14.0%). The surgical intent between the two groups
showed a statistically significant difference (p=0.027)
with the Magseed group more diagnostic excisional
biopsies. No significant difference is observed between
the two groups in surgical pathology results (p=0.991),
with the majority of findings being benign. Details of
surgery and pathology are listed in Table 2.
All markers were detected at the first operation and
successfully retrieved intact. No unplanned readmission
in the window between localisation and surgery was
documented for any patients who received decoupled
Magseed localisation. No complications were reported.
The clinical outcomes are presented in Table 2.
DISCUSSION
Our study demonstrates statistically comparable
effectiveness and safety between the Magseed and
conventional HWL in an Asian population in terms
of placement accuracy, rates of lesion detection,
marker retrieval, and complications. To the best of our
knowledge, this is the first study directly comparing the
performance between Magseed localisation and HWL in
Asians.
The Magseed system has been commercially available
in the United States since 2016.[10] Price et al[14] published the first study of this technique in 2018, documenting
the technical success of accurate marker placement
and lesion excision in a North American population.
Since then, a growing number of studies have been
conducted to provide more evidence of its clinical
feasibility in preoperative breast lesion localisation.[12] [16] [17]
The most commonly used localisation technique is still
the hookwire, based on the results of a recent national
questionnaire about the current practice of nonpalpable
breast lesion localisation in the United Kingdom.[18]
Although the HWL is still the practice standard, more
than half of the centres were dissatisfied with their current
localisation technique and had considered changing,
the Magseed system being the most commonly stated
alternative.[18] The main barriers to change were the higher
cost and lack of evidence base of the Magseed system.[18]
In Hong Kong, Magseed has only been used since 2019,
while HWL remains the most prevalent technique. One
pilot study conducted in Hong Kong has provided initial
insight into the efficacy and safety of Magseed in in an
Asian population.[19] Further robust evaluation of this
new method would be vital to support its wider clinical
application in Asian populations.
There is currently sparse evidence of direct comparison
between hookwire and Magseed pertaining to marker
placement accuracy. One abstract published by Micha
et al[17] found no difference between them, and the wire/seed marker within 5 mm of the lesion in 96% and 97% of cases, respectively. These results concur with
the results of the present study and provide additional
evidence for the use of Magseed in Asian populations.
In our study, one wire placed under ultrasound guidance
migrated after the post-deployment mammogram,
and one Magseed migrated after stereotactic-guided
localisation for same-day surgery, as shown in Figure 4.
The hookwire migration was probably related to
inadvertent dislodgement of its external component
during mammographic positioning. The Magseed
migrated along the direction of the needle track at
insertion, which was also observed in one previous study, and the accordion effect is suspected to be the cause of
this early migration.[16] Fatty breasts have been found to
be susceptible to the accordion effect,[20] and our patients
had dense breasts (Table 1), so we hypothesise that
there might be a lower risk of early migration in Asian
populations. The limitation of seed placement depth
of 3 cm is a big challenge for deeply located lesions.
Harvey et al[12] concluded that smaller breasts allow easier
location of the seed marker during surgery. The median
depth of Magseed on post-insertion ultrasound was
16 mm (range, 3.5-30 mm) in their study,[12] compared
with a mean depth of 9.5 mm (range, 2-18 mm) in the present study. Given that the lesions were generally
superficial in our patients, and breasts are smaller
and denser in Asian populations,[21] [22] we hypothesise
that Magseed is likely to provide more accurate seed
localisation and easier surgical excision in Asian
populations. Further investigation with larger sample
size and collaboration with breast surgeons to review the
surgical outcome are needed to verify our hypothesis.
One of the significant merits of Magseed localisation is
logistical flexibility. Previous studies have demonstrated
the efficacy and safety of decoupled image-guided
procedures and surgery.[14] [17] Our results are broadly
similar; none of the pre-inserted Magseeds migrated
and were successfully retrieved, and all the lesions were successfully excised at the first operation without
complications (Table 2). These findings are promising,
especially under the time and logistical constraints of a
pandemic, as Magseed localisation can provide greater
scheduling flexibility and efficiency in radiology suite
and operating theatre utilisation.
Our study has several limitations. This is a small
sample, retrospective, single-institution review, which
has inherent selection bias. Firstly, some patients were
chosen to have decoupled Magseed placement/surgery
instead of HWL due to rescheduling of their surgery
dates during the COVID-19 outbreak. Hence, the patient
selection was not randomised. Secondly, the surgical
intents between the two groups were statistically significantly different, where wide local excisions were
more common in the hookwire group, and diagnostic
excisional biopsies were more common in the Magseed
group. The differences can be explained by specific
logistical arrangements during the COVID-19 pandemic
period. First, there was a tendency to proceed with the
scheduled HWL and same-day operation for higher
priority therapeutic excision of malignant lesions, and
diagnostic excisional biopsies of non-malignant cases
were more likely to be rescheduled for decoupled
operation using the Magseed. Second, during certain
time periods, some of the malignant cases were referred
out to centres that do not handle suspected or confirmed
COVID-19 patients. Thus, nearly all who underwent
Magseed localisation and subsequent surgery were
those with non-malignant pathology on preoperative
biopsies and surgery with diagnostic intent (Table 2).
These factors may have potentially generated systematic
bias in this study. Based on these objective reasons, we
did not investigate and compare the surgical outcomes
of Magseed localisation and HWL, which is another
limitation. To date, few studies have been conducted
for a direct comparison of surgical outcomes between
Magseed localisation and HWL. Those performed in
European populations observed comparable rates of
margin positivity and re-excision,[23] [24] but no data are
available in Asia. Previously, Walsh et al[25] concluded
that higher breast density is associated with higher
re-excision rates in women having breast-conserving
surgery. Asian populations have denser and smaller
breasts[21] [22]; therefore, further analysis and comparison
of surgical outcomes between Magseed localisation
and HWL, including margin positivity, re-excision rate,
and specimen weight, would be important to look for
additional clinical benefits to justify a change of practice
from wire to Magseed localisation.
CONCLUSION
The results of the present study support the use of Magseed
localisation as a reliable substitute for conventional
HWL in Asian populations. Further investigation of
surgical outcomes, prospective multicentre randomised
studies with larger sample sizes, and cost-effectiveness
studies would be helpful to validate its widespread
clinical adoption.
REFERENCES
1. Frank HA, Hall FM, Steer ML. Preoperative localization of
nonpalpable breast lesions demonstrated by mammography. N
Engl J Med. 1976;295:259-60. Crossref
2. Homer MJ. Transection of the localization hooked wire during
breast biopsy. AJR Am J Roentgenol. 1983;141:929-30. Crossref
3. Luini A, Zurrida S, Paganelli G, Galimberti V, Sacchini V, Monti S,
et al. Comparison of radioguided excision with wire localization
of occult breast lesions. Br J Surg. 1999;86:522-5. Crossref
4. Gray RJ, Salud C, Nguyen K, Dauway E, Friedland J, Berman C,
et al. Randomized prospective evaluation of a novel technique for
biopsy or lumpectomy of nonpalpable breast lesions: radioactive
seed versus wire localization. Ann Surg Oncol. 2001;8:711-5. Crossref
5. Hughes JH, Mason MC, Gray RJ, McLaughlin SA, Degnim AC,
Fulmer JT, et al. A multi-site validation trial of radioactive
seed localization as an alternative to wire localization. Breast J.
2008;14:153-7. Crossref
6. Sharek D, Zuley ML, Zhang JY, Soran A, Ahrendt GM, Ganott MA.
Radioactive seed localization versus wire localization for
lumpectomies: a comparison of outcomes. AJR Am J Roentgenol.
2015;204:872-7. Crossref
7. Dryden MJ, Dogan BE, Fox P, Wang C, Black DM, Hunt K, et al.
Imaging factors that influence surgical margins after preoperative
125I radioactive seed localization of breast lesions: comparison
with wire localization. AJR Am J Roentgenol. 2016;206:1112-8. Crossref
8. Sajid MS, Parampalli U, Haider Z, Bonomi R. Comparison of
radioguided occult lesion localization (ROLL) and wire localization
for non-palpable breast cancers: a meta-analysis. J Surg Oncol.
2012;105:852-8. Crossref
9. Hayes MK. Update on preoperative breast localization. Radiol Clin
North Am. 2017;55:591-603. Crossref
10. Kapoor MM, Patel MM, Scoggins ME. The wire and beyond:
recent advances in breast imaging preoperative needle localization.
Radiographics. 2019;39:1886-906. Crossref
11. Jeffries DO, Dossett LA, Jorns JM. Localization for breast surgery:
the next generation. Arch Pathol Lab Med. 2017;141:1324-9. Crossref
12. Harvey JR, Lim Y, Murphy J, Howe M, Morris J, Goyal A, et al.
Safety and feasibility of breast lesion localization using magnetic
seeds (Magseed): a multi-centre, open-label cohort study. Breast
Cancer Res Treat. 2018;169:531-6. Crossref
13. Lamb LR, Bahl M, Lehman CD. Evaluation of a nonradioactive
magnetic marker wireless localization program. AJR Am J
Roentgenol. 2018;211:W202. Crossref
14. Price ER, Khoury AL, Esserman LJ, Joe BN, Alvarado MD. Initial
clinical experience with an inducible magnetic seed system for
preoperative breast lesion localization. AJR Am J Roentgenol.
2018;210:913-7. Crossref
15. Micha A, Sinnett V, Wilson R, Adams E, Patrick E, Hector L, et al.
Interim analysis of an evaluation of clinical outcome and patient
and clinician satisfaction with magnetic seeds compared with guide
wires for localisation of impalpable breast lesions for surgery. Eur
J Surg Oncol. 2019;45:884. Crossref
16. Lamb LR, Bahl M, Specht MC, D’Alessandro HA, Lehman CD.
Evaluation of a nonradioactive magnetic marker wireless
localization program. AJR Am J Roentgenol. 2018;211:940-5. Crossref
17. Thekkinkattil D, Kaushik M, Hoosein MM, Al-Attar M, Pilgrim S,
Gvaramadze A, et al. A prospective, single-arm, multicentre clinical
evaluation of a new localisation technique using non-radioactive
Magseeds for surgery of clinically occult breast lesions. Clin Radiol.
2019;74:974.e7-11. Crossref
18. Somasundaram SK, Potter S, Elgammal S, Maxwell AJ, Sami AS,
Down SK, et al. Impalpable breast lesion localisation, a logistical
challenge: results of the UK iBRA-NET national practice
questionnaire. Breast Cancer Res Treat. 2021;185:13-20. Crossref
19. Fung WY, Wong T, Chau CM, Yu EL, Chan TS, Chan RL, et al.
Safety and efficacy of magnetic seed localisation of non-palpable
breast lesions: pilot study in a Chinese population. Hong Kong
Med J. 2020;26:500-9. Crossref
20. Esserman LE, Cura MA, DaCosta D. Recognizing pitfalls in early and late migration of clip markers after imaging-guided directional
vacuum-assisted biopsy. Radiographics. 2004;24:147-56. Crossref
21. Maskarinec G, Meng L, Ursin G. Ethnic differences in
mammographic densities. Int J Epidemiol. 2001;30:959-65. Crossref
22. Ko SY, Kim EK, Kim MJ, Moon HJ. Mammographic density
estimation with automated volumetric breast density measurement.
Korean J Radiol. 2014;15:313-21. Crossref
23. Crane J, Photi E, Down S. A DGH’s experience using Magseed as a localisation tool for impalpable breast lesions. Eur J Surg Oncol. 2019;45:923-4. Crossref
24. Zacharioudakis K, Down S, Bholah Z, Lee S, Khan T, Maxwell AJ,
et al. Is the future magnetic? Magseed localisation for non palpable
breast cancer. A multi-centre non randomised control study. Eur J
Surg Oncol. 2019;45:2016-21. Crossref
25. Walsh SM, Brennan SB, Zabor EC, Rosenberger LH, Stempel M, Lebron-Zapata L, et al. Does breast density increase the risk of re-excision for women with breast cancer having breast-conservation therapy? Ann Surg Oncol. 2019;26:4246-53. Crossref