Single-centre Initial Experience of Transradial Access for Abdominal Interventional Radiology
ORIGINAL ARTICLE
Single-centre Initial Experience of Transradial Access for Abdominal Interventional Radiology
MC Lee, YK Wong, ACW Lee, HS Fung, JB Chiang, CH Kwok, LF Chiu
Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong
Correspondence: Dr Dr MC Lee, Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong.. Email: lmc753@ha.org.hk
Submitted: 3 Jun 2021; Accepted: 12 Aug 2021.
Contributors: All authors designed the study, acquired and analysed the data. MCL, YKW and ACWL drafted the manuscript, and critically
revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: The research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This retrospective study was approved by the Kowloon Central/Kowloon East Research Ethics Committee (Ref: KC/KE-21-0013/ER-2). The requirement for patient consent was waived by the ethics board. The patients provided written informed consent for all treatments and procedures.
Abstract
Background
Transradial access (TRA) has long been used for coronary and noncoronary angiographic procedures
with substantial benefits when compared with transfemoral access, including earlier ambulation, readily achieved
haemostasis, and shorter hospital stay. However, the transfemoral technique remains the mainstay of vascular access
in interventional radiology. We herein present a single institution’s experience with transradial intervention and
evaluates its feasibility and safety.
Methods
A total of 94 TRA procedures were performed in 69 patients (16 women and 53 men) between April 2017
and May 2020. These included 68 chemoembolisations of liver tumours, 15 procedures for selective internal radiation
therapy with yttrium-90, which included mapping and administration, eight renal angiomyolipoma embolisations,
one uterine artery embolisation, one left internal iliac embolisation for abdominal aortic aneurysm, and one pelvic
angioembolisation for trauma.
Results
Mean age of the patients was 65.9 years. Technical success was achieved in 90 of the 94 cases (95.7%).
Four cases (4.3%) required a change to transfemoral access (failed catheterisation of celiac axis or superior
mesenteric artery, very small radial artery, and an aortic anatomical variant). Two patients (2.1%) developed small
access site haematomas after the procedures. Mortality, stroke and radial artery occlusion rates at 30 days after
TRA procedures were 0%.
Conclusion
TRA is a safe, feasible and effective technique for abdominal interventional radiology procedures.
Key Words: Angiography; Femoral artery; Radial artery; Radiology, interventional
中文摘要
腹部介入放射學經橈動脈通路的單中心初步經驗
李文祚、黃汝麒、李昭穎、馮漢盛、蔣碧茜、郭昶熹、趙朗峰
背景
經橈動脈通路(TRA)長期用於冠狀動脈和非冠狀動脈血管造影術,與經股動脈通路相比的顯著優勢包括更早行走、易於止血和更短住院時間。然而,經股動脈技術仍然是介入放射學中血管通路的常用通路。我們分享單中心經橈動脈介入治療的經驗,並評估其可行性和安全性。
方法
2017年4月至2020年5月期間,69名患者(16名女性和53名男性)共進行94例TRA手術。其中包括68例肝腫瘤化療栓塞、15例包括定位和給藥的選擇性內放射治療、8例腎血管平滑肌脂肪瘤栓塞術、1例子宮動脈栓塞術、1例因腹主動脈瘤需要進行左髂內動脈栓塞術,以及1例因創傷需要進行盆腔血管栓塞術。
結果
患者平均年齡65.9歲。94例中技術成功佔90例。4例(4.3%)需要改用經股動脈通路(腹腔軸或腸系膜上動脈導管插入失敗、橈動脈非常小和主動脈解剖變異)。兩名患者(2.1%)術後出現通路部位小血腫。TRA術後30天死亡率、中風率和橈動脈閉塞率均為 0%。
結論
TRA是一種安全、可行和有效的腹部介入放射學技術。
INTRODUCTION
Transradial access (TRA) was initially described for
coronary angiography in 1989 by Campeau.[1] There has
been a growing body of evidence suggesting that TRA has
substantial benefits over transfemoral access (TFA) since
that time. Findings from meta-analyses such as RIVAL,[2]
MATRIX,[3] RIFLE-STEACS,[4] and STEMI-RADIAL,[5]
published in the cardiology literature, have driven the
switch from TFA to TRA. These studies demonstrated
statistically significant reduction in bleeding, access site
complications, and mortality with TRA compared with
TFA. TRA has increased in popularity in non-coronary
endovascular procedures more recently. The aim of this
study was to depict a single institution’s experience in
the technical approach of transradial intervention and
evaluate corresponding feasibility and safety.
METHODS
Retrospective analysis of the technical success and
associated complications was conducted for all TRA
procedures between April 2017 and May 2020.
Demographics of the patients, including age and sex,
indications for the procedures, the type of procedure,
technical success (defined by procedure completion
through the chosen method of access), and postprocedural
complications were obtained from electronic patient
records.
Transradial Access Technique
Preprocedural Assessment and Setup
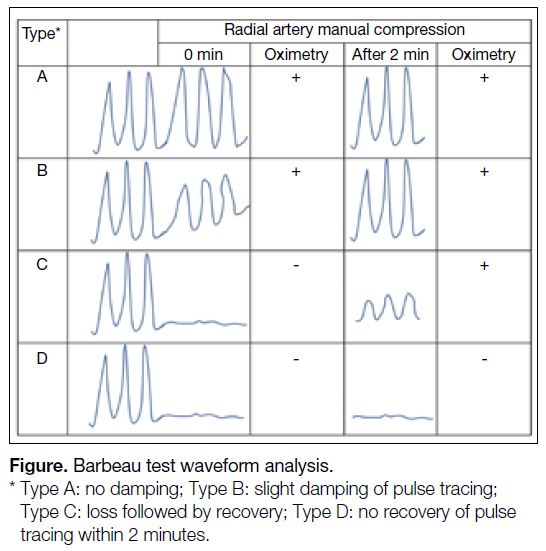
The Barbeau test[6] was performed on each patient before
TRA procedures to assess the completeness of the palmar
arch in order to reduce the risk of digital ischaemia. The
left radial artery is exclusively accessed to minimise
catheter length requirement and to limit manipulation
at the aortic arch. In this test, a pulse oximeter is
clamped on the patient’s thumb and the corresponding
morphology of the plethysmography tracing is recorded.
Waveform analysis is then continued for 2 minutes with
manual compression of the radial artery. Waveforms
are categorised into four types (A-D [Figure]). Patients
with types A and B responses have uninterrupted arterial
filling during radial artery occlusion (RAO) while those
with a type C response represents the recruitment of
collaterals in which there is initially absent interrupted
arterial filling with recovery of the waveform within
2 minutes. Type A to C waveforms suggest ulnopalmar
arch patency. The Type D waveform suggests absence
of sufficient arterial collateralisation and excludes the
patient from transradial catheterisation. The size of the
radial artery is ensured to be at least 1.7 mm in diameter
as measured by ultrasound with a compact linear array
(hockey-stick) ultrasound probe.
Figure. Barbeau test waveform analysis
Patients lie on the angiography table in the supine
position. There are two methods of positioning the patient’s arm, depending on the operator’s preferences
and the patient’s body build. In one, the left arm is
abducted at 90 degrees and placed on an arm board. The
second one would be the left shoulder adducted with
flexed elbow and pronated wrist which is placed over
the left groin, allowing placement of instruments over
the patient’s draped body, which enables operator and
monitor positioning comparable to that of TFA, although
it may be more difficult to achieve in obese patients.
If a distal transradial approach is adopted, the patient’s hand is partially clenched with the anatomic snuffbox
facing upwards.
Access
Depended on operators’ preferences, one of two
different methods of radial access, conventional radial
access or a distal transradial approach (dTRA, “snuffbox
approach”), was used. In conventional radial access, after
standard aseptic surgical preparation of the radial access
site, 1% lignocaine is injected into the subcutaneous
tissue around the radial artery from approximately 1 to
2 cm proximal to the radial styloid over a distance of 4 to
5 cm. Aseptic technique and local anaesthetic application
are similarly performed for dTRA at the anatomical
snuffbox.
The operator may choose a double-wall through-and-through approach or a single-wall anterior puncture. The
double-wall approach is mainly used for radial arterial puncture at the wrist level while the single-wall puncture
method is employed for dTRA at the anatomical
snuffbox.
In the double-wall approach, a 20-gauge angiocatheter
is angled at approximately 45˚ from the skin and is
slowly inserted to puncture the anterior wall of the
radial artery under ultrasonic guidance or by palpation.
Once backflow of arterial blood is observed, the whole
apparatus is advanced further to puncture the posterior
wall of the artery. The needle is then removed and the
angiocatheter is slowly withdrawn until pulsatile blood
is observed. The second method is to use a 21-gauge
38-mm needle (Radifocus Introducer Transradial Kit;
Terumo Interventional System, Somerset [NJ], United
States) to puncture the anterior wall of the radial artery
under ultrasonic guidance. Once pulsatile arterial blood
return is confirmed, a 0.021-inch guidewire is advanced
into the radial artery. A 5-Fr hydrophilic sheath is
placed over the wire using Seldinger technique. A total
of 3000 IU of heparin and 200 μg of nitroglycerin is
injected into the arterial sheath after insertion to prevent
vasospasm and radial artery thrombosis during and after
the procedure.
For repeat procedures, most patients who underwent
TRA for the first time again undergo TRA for subsequent
interventions due to its benefits and also because of
technical success achieved in the first attempt. For the
remaining few who underwent TFA in their second
or subsequent interventions, the choice of vascular
access was largely based on operator’s dependence and
experience.
Among the cases performed, none was omitted from
heparin administration due to its intrinsic purpose to
reduce the risk of RAO which is the primary procedure-related
complication of concern.
Catheter Selection
In majority of the cases, a 5-Fr 125 cm (Merit Ultimate
1; Merit Medical Systems, Inc, South Jordan [UT],
United States) or a 5-Fr 120-cm catheter (Terumo TIG
diagnostic catheter; Terumo Interventional System,
Tokyo, Japan), and a 150-cm Terumo guidewire are
used for catheterisation. Fluoroscopic guidance is
used for investigation when resistance is encountered
during advancement into the left arm and is universally
used from the level of the axillary artery and beyond
to prevent entry or over-manipulation of the vertebral
artery. The target vessels are selected and catheterised as desired following access to the abdominal aorta, and
angiography of the desired site is then performed.
Haemostasis
Haemostasis is achieved using compression.
Compression tape with haemostatic foam (STEPTY;
Nichiban, Tokyo, Japan) is applied over the puncture site
after removal of the sheath. Palpation of the radial pulse
with corresponding waveform analysis is performed
to confirm its patency to achieve non-occlusive
haemostasis. The STEPTY foam is kept in place for
4 hours before removal. If secondary bleeding is observed,
manual compression is applied. When haemostasis is
achieved, simple dressing is applied to the wound.
Discharge from Hospital
In general, patients are monitored by the referring
clinical team for secondary bleeding and postprocedural
complications until they are deemed fit for discharge.
RESULTS
From April 2017 to May 2020, a total of 94 TRA
procedures were performed on 69 patients (16 female
and 53 male) at our institution for abdominal
interventions with a technical success rate of 95.7% (90
of 94 procedures). More than one TRA procedures were
performed in some of the patients. The radial artery was
re-assessed before each repeated procedure.
Of the 94 TRA procedures performed, the dTRA/snuffbox approach was employed in 18 cases while the
transradial approach was adopted in the other 76 cases.
Procedures included 68 chemoembolisations of liver
tumours in 44 patients; 15 procedures for selective
internal radiation therapy with yttrium-90 in 14 patients,
which included mapping and administration; eight
renal angiomyolipoma embolisations in eight patients;
one uterine artery embolisation; one left internal iliac
embolisation for abdominal aortic aneurysm; and one
pelvic angioembolisation for trauma.
The mean age of the patients was 65.9 years. Four cases (4.3%) required crossover to TFA (failed catheterisation
of celiac axis or superior mesenteric artery, very small
radial artery, and aortic anatomical variation).
Barbeau’s test results were documented in 55 of 94
procedures (58.5%) in which all of them demonstrated
types A to C waveforms (type A: 29, type B: 19, type C: 6).
There is no standardised follow-up after each TRA
procedure in our institution and therefore the incidence
of RAO after TRA procedures is unknown. Among
the repeated TRA procedures, none of the patients was
discovered to have RAO during preprocedural assessment.
Small haematomas at the insertion site developed after two out of 94 (2.1%) TRA procedures and these were
treated conservatively.
The mortality and stroke rates at 30 days after TRA
procedures were 0%.
DISCUSSION
TRA is a safe, feasible and effective technique for
abdominal interventional radiology procedures.
Benefits of Radial Access
Dual blood supply of the hand and the superficial
position of the radial artery are intrinsic advantages when
compared with the transfemoral approach. Anastomosis
from the ulnar artery prevents harm if inadvertent injury
to the radial artery occurs. Haemostasis via compression
without the need of a vascular closure device is also
easier, as the radial artery is more superficial. In contrast,
there is risk of retroperitoneal haemorrhage in TFA due
to inadvertently high punctures. Haemostasis is also
more difficult in TFA.
Mobilisation after the procedure is immediate for TRA
patients, while those with TFA require monitoring and
bed rest to ensure haemostasis. The TRA therefore
reduces patients’ discomfort and the risks of bleeding
complications.
For cases with moderate bleeding risk, it is recommended
that the international normalised ratio should be <1.5
according to The Society of Interventional Radiology
and Cardiovascular and Interventional Radiology
Society of Europe consensus guidelines. However,
Titano et al[7] concluded from 2271 patients that those
with an international normalised ratio >1.5 are still safe to
undergo TRA. Due to easier haemostasis, TRA can also
be adopted in patients with uncorrectable coagulopathy
or thrombocytopenia. The TRA is therefore superior to
TFA for transarterial chemoembolisation in patients with
liver disease–related coagulopathy or thrombocytopenia.
In addition, anticoagulation therapy in patients with
conditions such as metallic heart valves or, rarely, protein
C or S deficiencies can remain uninterrupted during the
procedure.
It can be challenging to locate the common femoral artery
in obese patients. Moreover, atherosclerotic calcifications
may render TFA cannulation of the femoral arteries
difficult. Radial arteries are easier to access and less
often affected by calcified plaque. As such, transradial
approach is more favourable in obese patients.
Yamada et al[8] demonstrated that 81% of patients who
experienced both approaches would prefer TRA over
TFA due to less pain and earlier mobilisation.
Potential Complications of Radial Access
Significant haematoma formation, pseudoaneurysm
formation, symptomatic RAO, temporary or permanent
ischaemic or neurological events including stroke are the
potential complications. During TRA access, the great
vessels are crossed with wires and catheters, which may
increase the risk of stroke. In abdominal intervention, the
risk of stroke in TFA is negligible but not absent in TRA.
In the two patients who developed local haematomas
at puncture sites, neither was on antiplatelet nor
anticoagulant therapy. The complication was attributed
to either inadequate manual compression or suboptimal
positioning of the STEPTY haemostatic material, for
which further training should be given to interventionists
for outcome improvement. No other particular adjustment
for haemostasis is made in patients on antiplatelet drugs
or anticoagulants, as TRA itself imposes a lower bleeding
risk than that in TFA.
There are studies reviewing neurological complications
after TRA. Patel et al[9] concluded that TRA is not
associated with a significant increase in stroke rate
compared with TFA in coronary arterial intervention.
Posham et al[10] analysed more than 1500 TRA
procedures for non-coronary interventions and none of
them experienced a stroke event up to 30 days after the
procedure. Regardless, potential complications including
stroke are discussed and explained in the informed
consent.
For our patients with documented Barbeau test results,
none showed the type D waveform. Barbeau et al[6]
revealed among 1010 consecutive patients that only
1.5% showed the type D waveform and were excluded
from TRA. In short, TRA is feasible in most cases.
In four of the cases in which TRA could not be achieved, one of them was related to a very small radial artery.
Although Barbeau’s test revealed a type B waveform, TRA was unsuccessful under ultrasound guidance and
by palpation due to the very small calibre. Crossover to a
right transfemoral approach was therefore performed to
complete embolisation of a left renal angiomyolipoma.
Anatomical variation at the aortic arch may also render TRA unsuccessful. We had a patient with a type 3 aortic
arch in which the guidewire could not be manipulated
into the descending aorta, and crossover to a right
transfemoral approach was required.
It can be challenging to catheterise small vessels
originating near the aortic arch in TRA, as significant
catheter manipulation is required. This is demonstrated
in cases of bronchial artery embolisation, in which
acute turns or forming reverse curves are necessary to
catheterise the bronchial arteries.
Other drawbacks of TRA include increased distance
from the lower torso as compared with the transfemoral
approach, limiting its application in intervention beyond
the inguinal regions owing to unavailability of catheters of
sufficient length. The radial artery cannot accommodate
arterial sheaths larger than 6 Fr, which limits the size
of stents or balloons that can be deployed. TFA may
therefore be preferable to TRA in such circumstances.
Emergency cases requiring intervention usually involve pathology in the abdominopelvic region, and under life-threatening conditions, rapid vascular access is of the
utmost importance. In these situations, TFA remains
the preferred route of vascular access due to the shorter
distance from the lower torso and shorter time taken to
secure access.
There are no standardised follow-up protocols and
documentations of complications following TRA
procedures in our institution. This retrospective analysis
may therefore underestimate the number of complications.
However, there was no significant morbidity after TRA
procedures documented in the electronic patient records,
such as severe bleeding requiring transfusion, stroke,
or death. The incidence of radial artery thrombosis is
probably underestimated, as there is no regular interval
follow-up Doppler ultrasound assessment of the radial
artery after TRA procedures. It is typically asymptomatic
for mild radial artery thrombosis and may therefore
not be called to the physicians’ attention. A systematic
review and meta-analysis[11] showed that the incidence of
RAO varied from 1% to 33%. It also revealed that the
incidence was 7.7% within 24 hours after TRA.
In recent years, the dTRA/snuffbox approach was
proposed to overcome some of the limitations of TRA,
such as the risk of RAO. Kiemeneij et al[12] first evaluated
the safety and feasibility of this approach in 2017. The
radial artery branches before reaching the anatomical
snuffbox. In dTRA, access is acquired distal to the branch
point, which ensures preservation of vascular flow to the
palm from other branches in case of vessel occlusion
occurring at the puncture site. Flow interruption to the
palm is therefore also minimised during haemostatic
compression over the access branch in this approach.
Positioning is flexible, as the snuffbox is in the dorsum
of the hand. For instance, it permits shoulder adduction
with the left wrist pronated over the lower abdomen or
suprapubic region. This is beneficial for patients with
frozen shoulder who have limited shoulder abduction
and in patients with upper limb contractures (e.g., due
to prior stroke) with difficulty in exposing the palmar
aspect of the wrist for conventional radial access.[13]
From a prospective analysis,[14] absence of blood
flow during haemostasis increases the risk of RAO.
Another retrospective analysis comparing the duration
of haemostasis concluded that occlusive haemostasis
was the only independent predictor of RAO, while
maintenance of flow in the radial artery after sheath
removal (patent haemostasis) has been shown to reduce
the rate of RAO after TRA, where dTRA would therefore
serve as a more favourable approach.
Patent haemostasis or non-occlusive haemostasis can
be adopted to minimise the chance of RAO. A radial
compression device — the “TR Band” (Terumo) may
help to achieve this goal. After the procedure, the device
can be placed on the patient’s wrist with the strap fixed
tightly to prevent excessive movement. The TR band
balloon is inflated slowly by injecting 15 to 18 mL
of air on top of the puncture site while the sheath is
simultaneously removed. The amount of air in the
balloon can then be titrated until the bleeding stops. A
reverse Barbeau test is performed in which both ulnar
and radial arteries are compressed simultaneously at first
until the plethysmographic wave is lost. Pressure on the
radial artery is then released to evaluate the waveform.
The waveforms indicating the degree of flow in the radial
artery can guide the extent of balloon inflation.
We applied STEPTY haemostatic foam instead of the
TR band in our institution as the former is more cost-effective.
Limitations
This was a retrospective study without a control group. However, the aim of this study was to show the safety
and feasibility of TRA rather than any superiority of
TRA over TFA. Patients were not randomised to TRA
or TFA but based largely on the operator’s preferences.
Results may therefore be affected by selection bias. As
discussed above, the number of complications may be
underestimated, as there are no standardised follow-up
protocols and documentation after TRA procedures.
Finally, results observed may not apply to all institutions
and should depend on the experience of operators and
number of TRA procedures performed.
CONCLUSION
TRA is a safe, feasible, and effective technique for
abdominal interventional radiology procedures. In view
of its substantial benefits, TRA might be considered
in conditions not limited to abdominal interventional
radiology procedures.
REFERENCES
1. Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3-7. Crossref
2. Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P,
et al. Radial versus femoral access for coronary angiography
and intervention in patients with acute coronary syndromes
(RIVAL): a randomised, parallel group, multicentre trial. Lancet.
2011;377:1409-20. Crossref
3. Valgimigli M, Gagnor A, Calabró P, Frigoli E, Leonardi S, Zaro T, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomized multicentre trial. Lancet. 2015;385:2465-76. Crossref
4. Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S,
Pendenza G, et al. Radial versus femoral randomized investigation
in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS
(Radial versus Femoral Randomized Investigation in
ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol.
2012;60:2481-9. Crossref
5. Bernat I, Horak D, Stasek J, Mates M, Pesek J, Ostadal P, et al.
ST-segment elevation myocardial infarction treated by radial
or femoral approach in a multicenter randomized clinical trial:
the STEMI-RADIAL trial. J Am Coll Cardiol. 2014;63:964-72. Crossref
6. Barbeau GR, Arsenault F, Dugas L, Simard S, Larivière MM.
Evaluation of the ulnopalmar arterial arches with pulse oximetry
and plethysmography: comparison with the Allen’s Test in 1010
patients. Am Heart J. 2004;147:489-93. Crossref
7. Titano JJ, Biederman DM, Zech J, Korff R, Ranade M, Patel R,
et al. Safety and outcomes of transradial access in patients with
international normalized ratio 1.5 or above. J Vasc Interv Radiol.
2018;29:383-8. Crossref
8. Yamada R, Bracewell S, Bassaco B, Camacho J, Anderson MB,
Conrad A, et al. Transradial versus transfemoral arterial access
in liver cancer embolization: randomized trial to assess patient
satisfaction. J Vasc Interv Radiol. 2018;29:38-43. Crossref
9. Patel VG, Brayton KM, Kumbhani DJ, Banerjee S, Brilakis ES. Meta-analysis of stroke after transradial versus transfemoral artery
catheterization. Int J Cardiol. 2013;168:5234-8. Crossref
10. Posham R, Biederman DM, Patel RS, Kim E, Tabori NE,
Nowakowski FS, et al. Transradial approach for noncoronary
interventions: a single-center review of safety and feasibility in
the first 1500 cases. J Vasc Interv Radiol. 2016;27:159-66. Crossref
11. Rashid M, Kwok CS, Pancholy S, Chugh S, Kedev SA, Bernat I,
et al. Radial artery occlusion after transradial interventions:
a systematic review and meta-analysis. J Am Heart Assoc.
2016;5:e002686. Crossref
12. Kiemeneij F. Left distal transradial access in the anatomical
snuffbox for coronary angiography (LdTRA) and interventions
(LdTRI). EuroIntervention. 2017;13:851-7. Crossref
13. Pua U, Sim JZ, Quek LH, Kwan J, Lim GH, Huang IK. Feasibility
study of “Snuffbox” radial access for visceral interventions. J Vasc
Interv Radiol. 2018;29:1276-80. Crossref
14. Sanmartin M, Gomez M, Rumoroso JR, Sadaba M, Martinez M,
Baz JA, et al. Interruption of blood flow during compression and
radial artery occlusion after transradial catheterization. Catheter
Cardiovasc Interv. 2007;70:185-9. Crossref