British Society of Neuroradiologists Grand Round — Paediatric Neuroradiology: Brief Communication
BRIEF COMMUNICATION
British Society of Neuroradiologists Grand Round — Paediatric Neuroradiology: Brief Communication
TM Chiu1, LHQ Chin2
1 Department of Radiology, Hong Kong Children Hospital, Hong Kong
2 Department of Radiology, Queen Mary Hospital, Hong Kong
Correspondence: Dr LHQ Chin, Department of Radiology, Queen Mary Hospital, Hong Kong. Email: chin.leanne@gmail.com
Submitted: 10 Apr 2022; Accepted: 30 Jun 2022.
Contributors: Both authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. Both authors had full access to the data, contributed to the study, approved the final version for publication,
and take responsibility for its accuracy and integrity.
Conflicts of Interest: Both authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Acknowledgement: We thank Dr Chris KC Wong (Hong Kong Children Hospital, Hong Kong), Dr Elaine YL Kan (Hong Kong Children Hospital, Hong Kong), Dr Shubhabrata Biswas (The Walton Centre, Liverpool), and Prof Winnie CW Chu (Prince of Wales Hospital, CUHK, Hong Kong) for leading the virtual BSNR Grand Round; and the Hong Kong College of Radiologists (HKCR) and Dr YC Wong (Warden of
HKCR) for the coordination and collaborative hosting with the British Society of Neuroradiology (BSNR).
INTRODUCTION
The British Society of Neuroradiologists (BSNR) Grand
Rounds are webinars held biweekly (every 2nd and
4th Wednesday of the month) that feature interesting
and educational neuroradiology case presentations
from various institutions in the United Kingdom and
around the globe. The Grand Rounds are open to all,
and registration is free of charge (https://bsnr.org.uk/grandround/"). The BSNR regularly post updates of these
sessions and other related educational content via social
media (https://twitter.com/thebsnr).
The Hong Kong College of Radiologists (HKCR)
Paediatric Training Network is composed of all accredited
paediatric radiology training centres in Hong Kong.
In collaboration with the HKCR Paediatric Training
Network, two teams of interventional neuroradiologists
and paediatric neuroradiologists were selected to present
BSNR Grand Rounds. The first of these collaborative
BSNR Grand Rounds on neuro-intervention was held on 22 September 2021; the second on paediatric
neuroradiology was held on 26 January 2022.
A total of four cases were presented as part of the BSNR
Grand Round on paediatric neuroradiology. Two cases
covered paediatric stroke: focal cerebral arteriopathy
of childhood presented by Dr Philip Lee (Tuen Mun
Hospital, Hong Kong); and multisystem smooth muscle
dysfunction syndrome presented by Dr Claudia Cheung
(Hong Kong Children Hospital, Hong Kong). In this
report, we provide a summary and discussion of the
other two cases on brain tumour–like mimics.
PRESENTATION EXPERIENCE
Cerebral Phaeohyphomycosis — Presented
by Dr Leanne Chin
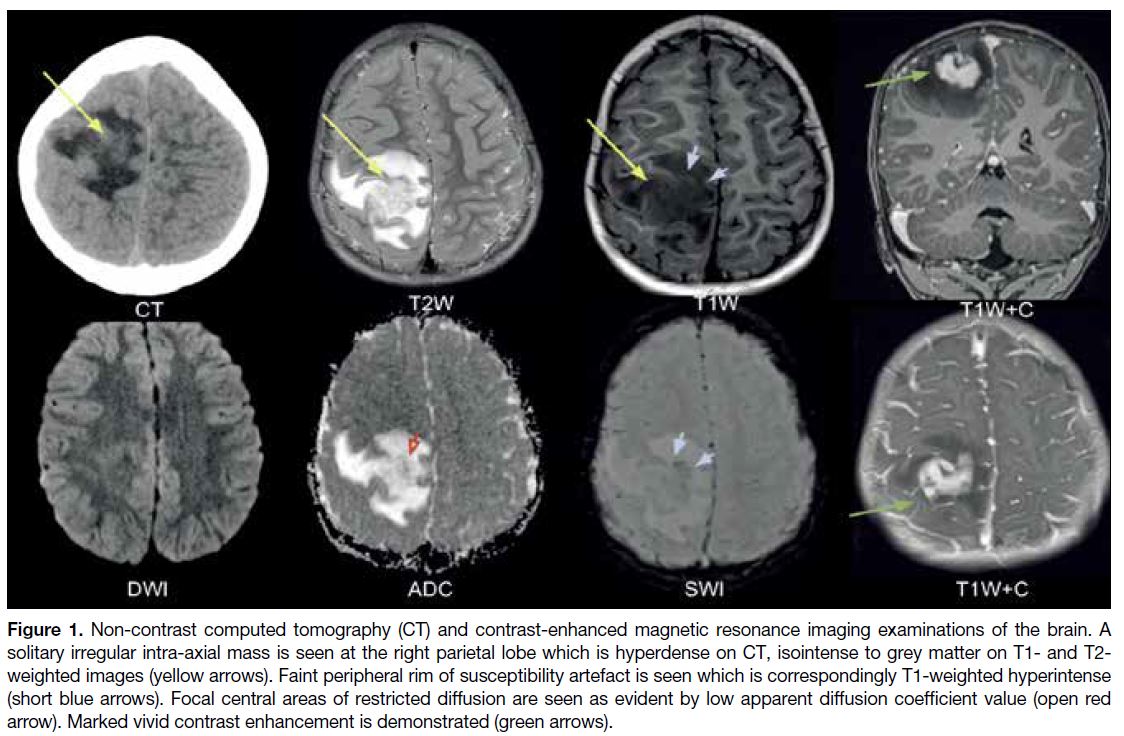
This case highlighted an intriguing and educational
diagnostic challenge provided by an unusual paediatric
cerebral tumour–like mimic in a 6-year-old boy with
recent history of headache, and left upper limb seizure for 1 day. Computed tomography and magnetic
resonance imaging (MRI) examinations of the brain
revealed a solitary intra-axial enhancing T2-weighted
hypointense mass in the right upper parietal lobe
(Figure 1). The mass exhibited a restricted diffusion
pattern, with a susceptibility rim artefact and perilesional
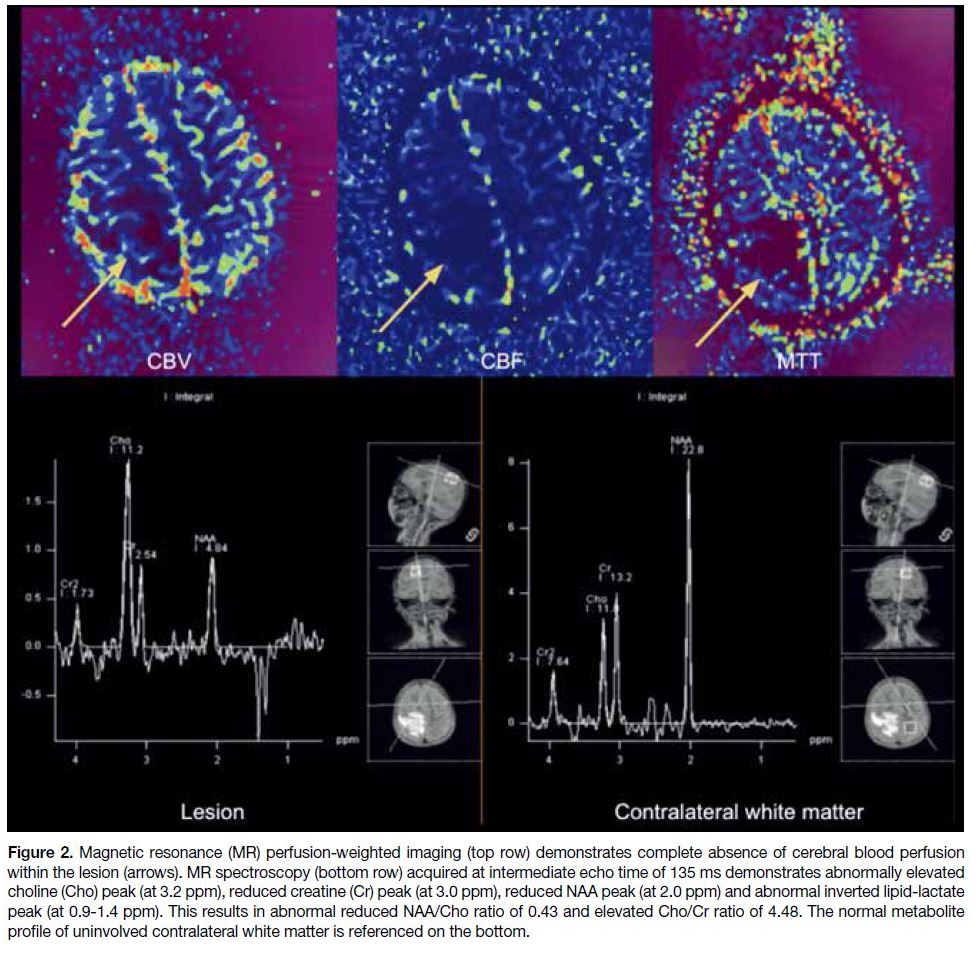
oedema. Subsequent MR spectroscopy of the lesion
revealed an elevated Cho:NAA ratio and abnormal
lipid-lactate peaks, whereas MR perfusion revealed no
perfusion (Figure 2). The working diagnosis at the time
was high-grade glioma, necessitating an emergency
craniotomy. After a successful complete excision,
histology revealed an unexpected diagnosis of cerebral
phaeohyphomycosis.
Figure 1. Non-contrast computed tomography (CT) and contrast-enhanced magnetic resonance imaging examinations of the brain. A
solitary irregular intra-axial mass is seen at the right parietal lobe which is hyperdense on CT, isointense to grey matter on T1- and T2-weighted images (yellow arrows). Faint peripheral rim of susceptibility artefact is seen which is correspondingly T1-weighted hyperintense
(short blue arrows). Focal central areas of restricted diffusion are seen as evident by low apparent diffusion coefficient value (open red
arrow). Marked vivid contrast enhancement is demonstrated (green arrows).
Figure 2. Magnetic resonance (MR) perfusion-weighted imaging (top row) demonstrates complete absence of cerebral blood perfusion
within the lesion (arrows). MR spectroscopy (bottom row) acquired at intermediate echo time of 135 ms demonstrates abnormally elevated
choline (Cho) peak (at 3.2 ppm), reduced creatine (Cr) peak (at 3.0 ppm), reduced NAA peak (at 2.0 ppm) and abnormal inverted lipid-lactate
peak (at 0.9-1.4 ppm). This results in abnormal reduced NAA/Cho ratio of 0.43 and elevated Cho/Cr ratio of 4.48. The normal metabolite
profile of uninvolved contralateral white matter is referenced on the bottom.
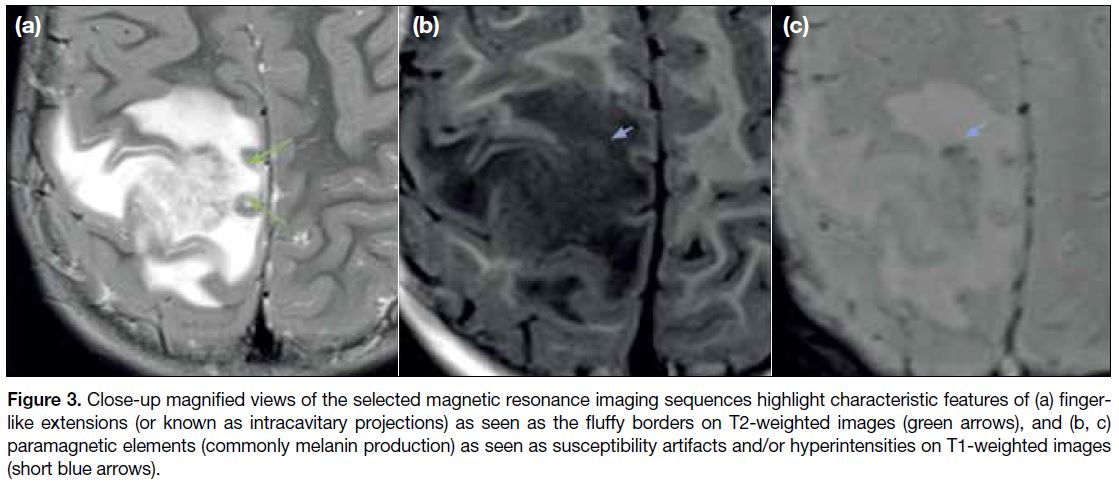
On MRI, aggressive cerebral fungal infections can
closely resemble high-grade brain tumours in terms of
contrast enhancement, restricted diffusion, and vasogenic
oedema.[1] On retrospective radiological review, however,
thorough analysis of the lesion morphology reveals two
characteristic diagnostic features[2]: finger-like extensions
of fungal hyphae and paramagnetic elements of melanin
production (Figure 3). Although abnormal choline and lipid-lactate metabolite peaks are frequently associated
with high-grade malignancies, the absence of lesion
perfusion is sometimes considered to be a paradoxical
finding. Therefore, reliance on MR spectroscopy and
perfusion imaging may not be useful in every case
to differentiate between malignancy from aggressive
fungal infection.[1] [3] [4]
Figure 3. Close-up magnified views of the selected magnetic resonance imaging sequences highlight characteristic features of (a) finger-like
extensions (or known as intracavitary projections) as seen as the fluffy borders on T2-weighted images (green arrows), and (b, c)
paramagnetic elements (commonly melanin production) as seen as susceptibility artifacts and/or hyperintensities on T1-weighted images
(short blue arrows).
An important take-away message from this case is that the
occurrence of an isolated cerebral phaeohyphomycosis in
an otherwise immunocompetent patient should prompt
an active search for underlying CARD9 deficiency, as
was confirmed in this patient via genetic testing. The
case report by Lai et al[5] provides further detail on this
patient and outcome.
As a result of our experience presenting this case at the
BSNR Grand Round, we have gained new knowledge
and skills in developing effective and systematic
diagnostic pathways while avoiding radiological
pitfalls. The differential diagnosis and case summaries
of the pathologies were also well appreciated by the
audience.
Multiple Cerebral Cavernoma — Presented
by Dr Milly Chiu
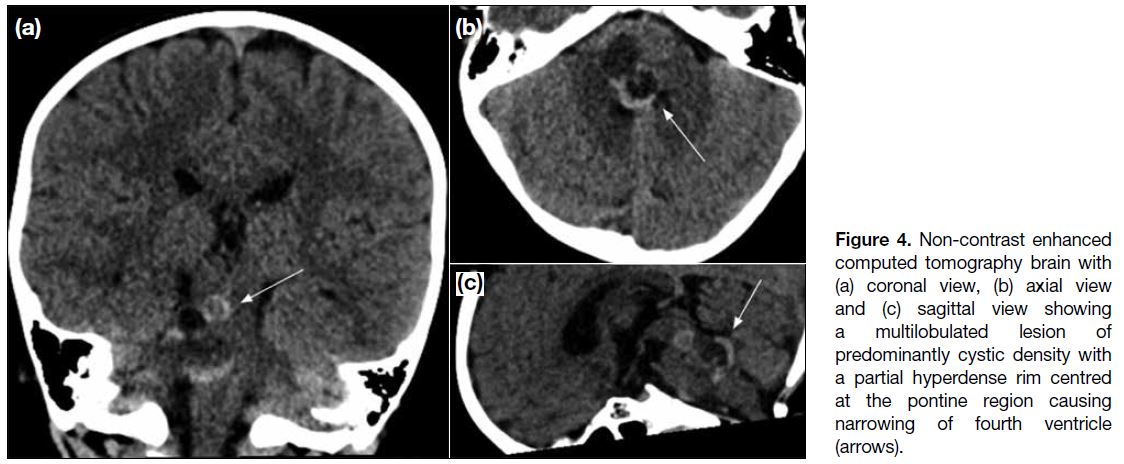
This case provided another illustration of a brain
tumour–like mimic, featuring a 4-year-old girl with
good past health who was referred to the paediatric
oncology team for suspected diffuse intrinsic pontine
glioma. She presented with a 2-week history of gaze
palsy. Initial computed tomography scan of the brain
revealed a solitary lesion centred at the pons, which
appeared multiloculated with predominantly hypodense
content and a partial hyperdense rim suspicious of
blood product or calcification (Figure 4). MRI was performed shortly afterwards, and the lesion appeared
predominantly hyperintense on T1- and T2-weighted
images with internal dependent hypointense contents.
No significant solid enhancing component was seen
(Figure 5). The initial imaging differentials considered
were brainstem gliomas, possibly complicated with
haemorrhage, or lesions that contain calcification,
including ganglioglioma, rosette-forming glioneuronal
tumour, or pilocytic astrocytoma.
Figure 4. Non-contrast enhanced computed tomography brain with (a) coronal view, (b) axial view and (c) sagittal view showing a multilobulated lesion of predominantly cystic density with a partial hyperdense rim centred at the pontine region causing narrowing of fourth ventricle (arrows).
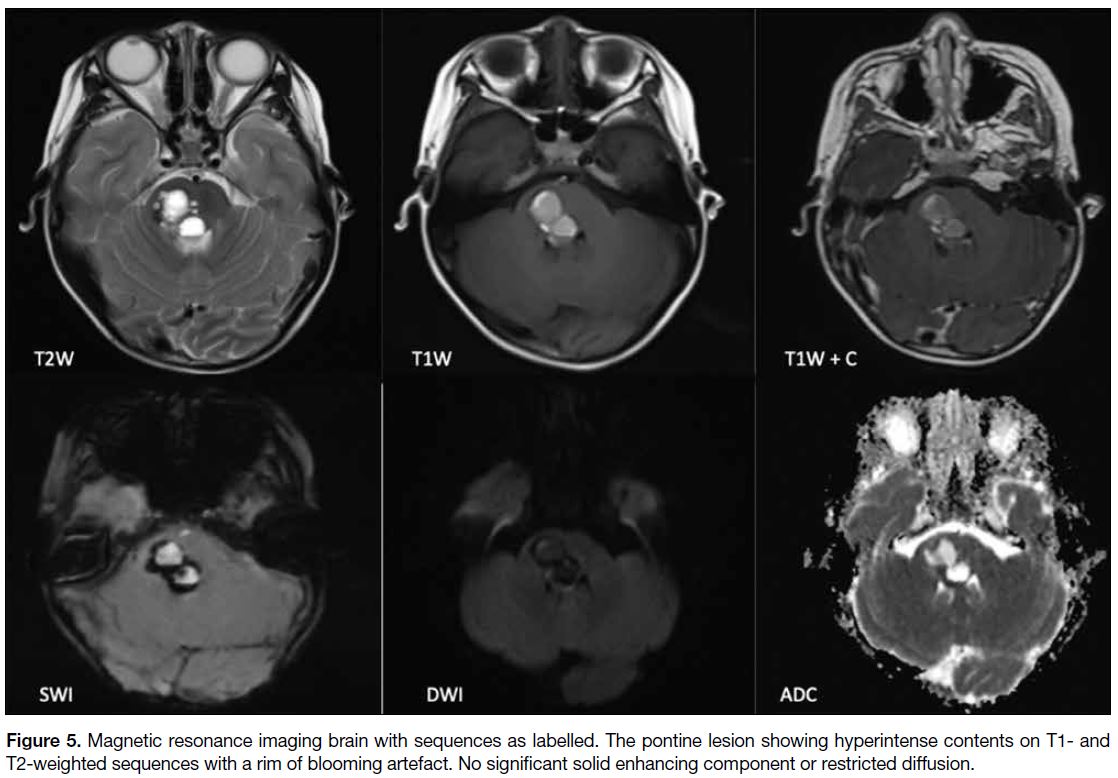
Figure 5. Magnetic resonance imaging brain with sequences as labelled. The pontine lesion showing hyperintense contents on T1- and T2-weighted sequences with a rim of blooming artefact. No significant solid enhancing component or restricted diffusion.
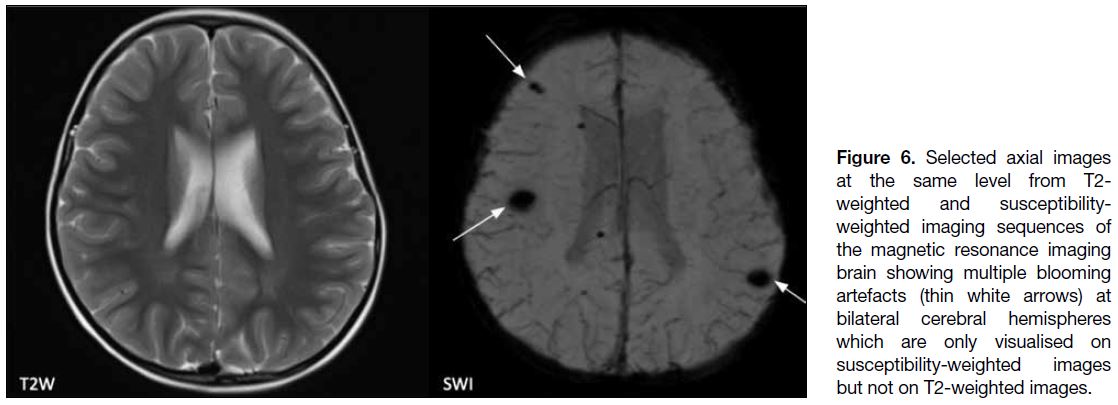
However, on further review of the susceptibility weighted imaging sequence, there were numerous small intra-axial blooming foci in bilateral cerebral hemispheres.
These lesions were inconspicuous on all other sequences
(Figure 6). The final radiological diagnosis of multiple
cavernoma was made, which was concordant with
subsequent intraoperative and histopathological findings.
Figure 6. Selected axial images at the same level from T2-weighted and susceptibility-weighted
imaging sequences of the magnetic resonance imaging brain showing multiple blooming artefacts (thin white arrows) at bilateral cerebral hemispheres which are only visualised on susceptibility-weighted images but not on T2-weighted images.
The most classically quoted description of cerebral
cavernoma would perhaps be a “popcorn-appearance”—with a multilobulated lesion of heterogeneous signal
intensity with a prominent hypointense rim on
T2-weighted images, representing multiloculated
haemorrhages of different ages.[6] This appearance was not appreciated in this case, such that the possibility of
brainstem tumours was cautiously raised. The diagnosis
of multiple cerebral cavernoma was made almost certain
upon subsequently reviewing the susceptibility weighted
images, the less likely differential being haemorrhagic
metastases in the absence of a primary malignancy.
Presence of multiple cavernomas raises the concern of
familial cerebral cavernoma malformation, and this
is highlighted by this case where two disease-causing
mutations — KRIT1 and CCM2 — were eventually
confirmed on genetic studies.[7]
It was gratifying to receive a significant positive response
from the audience, with the majority of them finding this
case to be highly unusual, interesting, and educational to
their training and practice.
CONCLUDING REMARKS
It was a rewarding experience to present at the BSNR
Grand Round, to have received an overwhelming amount
of support from seniors and colleagues and constructive feedback from the international audience. We hope that
the audience appreciated these two fascinating cases
and learned that not all disease processes that result
in mass formation are indicative of brain tumours. A
wide spectrum of pseudotumour-like mimics exists
with overlapping clinical and radiological features, but
scrutiny of their unique imaging features will aid in the
radiological diagnosis.
Similar to the BSNR Grand Rounds, the HKCR
Paediatric Training Network is excited to launch regular
online teaching rounds and webinars in the near future,
with the goal of expanding professional training, learning
opportunities, and collaboration between Hong Kong
and international radiologists.
REFERENCES
1. Hauck EF, McGinnis M, Nauta HJ. Cerebral phaeohyphomycosis mimics high-grade astrocytoma. J Clin Neurosci. 2008;15:1061-6. Crossref
2. Luthra G, Parihar A, Nath K, Jaiswal S, Prasad KN, Husain N, et al.
Comparative evaluation of fungal, tubercular, and pyogenic brain
abscesses with conventional and diffusion MR imaging and proton
MR spectroscopy. AJNR Am J Neuroradiol. 2007;28:1332-8. Crossref
3. Santosh V, Mahadevan A, Chickabasaviah YT, Bharath RD,
Krishna SS. Infectious lesions mimicking central nervous system
neoplasms. Semin Diagn Pathol. 2010;27:122-35. Crossref
4. Jung NY, Kim E. Cerebral phaeohyphomycosis: a rare cause of
brain abscess. J Korean Neurosurg Soc. 2014;56:444-7. Crossref
5. Lai SH, Duque JS, Chung BH, Chung TW, Leung D, Ho RS, et al.
Invasive cerebral phaeohyphomycosis in a Chinese boy with
CARD9 deficiency and showing unique radiological features,
managed with surgical excision and antifungal treatment. Int J
Infect Dis. 2021;107:59-61. Crossref
6. Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J,
Drayer BP, et al. The natural history of familial cavernous
malformations: results of an ongoing study. J Neurosurg.
1994;80:422-32. Crossref
7. Zafar A, Quadri SA, Farooqui M, Ikram A, Robinson M, Hart BL,
et al. Familial cerebral cavernous malformations. Stroke.
2019;50:1294-301. Crossref