Entering the Era of Non-fasting Intravenous Contrast-Enhanced Computed Tomography
PERSPECTVE
Hong Kong J Radiol 2023 Jun;26(2):127-32 | Epub 20 Jun 2023
Entering the Era of Non-fasting Intravenous Contrast-Enhanced Computed Tomography
YS Chan1, CCM Cho1, CSL Tong1, AWH Ng2
1 Department of Imaging and Interventional Radiology, Prince of Wales Hospital, Hong Kong SAR, China
2 AmMed Medical Diagnostic Center, Hong Kong SAR, China
Correspondence: Dr YS Chan, Department of Imaging and Interventional Radiology, Prince of Wales Hospital, Hong Kong SAR, China. Email: juliannayschan@cuhk.edu.hk
Submitted: 2 Mar 2022; Accepted: 17 May 2022.
Contributors: YSC and AWHN designed the study and acquired the data. YSC analysed the data and drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Abstract
An empirical fasting period of at least 4 hours prior to intravenous contrast administration for computed tomography scans has been an age-old practice. This is associated with patient discomfort, adverse effects on diabetic control, and limits the flexibility of scanning arrangements in urgent settings. The effect is further compounded by the rising number of urgent imaging requests with some patients requiring repeated fasting while waiting for scanning slots. International guidelines have been recently updated, stating that with the improved safety profile of contrast media, fasting is no longer routinely required. In this article, we discuss the current evidence and its implications for our local practice. We share our approach of a stepwise policy change with eventual full implementation of non-fasting policy to all eligible patients in our institution, and the safety data we compiled. Adoption of a non-fasting policy for contrast-enhanced computed tomography is a feasible and beneficial practice adhering to international standards.
Key Words: Contrast media; Nausea; Pneumonia, aspiration; Vomiting
中文摘要
進入無需禁食的靜脈顯影電腦斷層掃描的世代
陳奕璇、曹子文、唐倩儂、伍永鴻
電腦斷層掃描靜脈造影劑給藥前至少要求4小時的禁食期一直是一種經驗性做法。這可增加患者不適、不利糖尿病控制,並限制了緊急情況下掃描安排的靈活性。緊急掃描需求數量的增加進一步加劇了這些影響,一些患者在等待掃描時段時需要反覆禁食。最近更新的國際指引指出,隨着造影劑安全性提高,不再需要常規禁食。在本文中,我們討論了當前的證據及其對我們本地實踐的影響。我們分享了我們逐步改變政策的方法最終使我們機構中所有符合條件的患者無需禁食,以及我們收集的安全數據。採用對比顯影掃描的無需禁食政策符合國際標準,且可行有益。
INTRODUCTION
Computed tomography (CT) has been commercially
available since the 1970s and is one of the most widely
used imaging modalities.[1] Conventional intravenous
iodinated contrast emerged in the 1970s to 1980s,
allowing for its application in CT, and is now an almost
indispensable part of daily practice.[2] From then till now,
the contrast agents we use have undergone important
changes.
The intravenous contrast used in CT is iodine-based
and is classified based on osmolality. High-osmolar
contrast media (HOCM) was the first generation of
iodinated intravenous contrast and was associated with
a high rate of adverse events (5%-8% acute adverse
reactions, which essentially encompassed all contrast
reactions, and 1%-2% moderate non–life-threatening
adverse reactions, which included faintness, vomiting
[severe], urticaria [profound], facial edema, laryngeal
edema and bronchospasm [mild]).[3] The majority
of the chemotoxic effects are mainly related to the
hyperosmolality.[3] Nausea and vomiting are common
adverse effects with reported incidences of 4.58% and
1.84%, respectively.[4] Subsequently, since the 1990s,
iso-osmolar contrast media (IOCM) and low-osmolar
contrast media (LOCM), which are associated with
an overall much lower risk of adverse reactions, have
replaced HOCM. A retrospective review by Hunt et al[5]
reported an adverse reaction rate of 0.153% for LOCM
based on 298,491 doses, the prevailing majority of
which were mild reactions not requiring treatment.
The incidences of nausea and vomiting with the use of
non-ionic contrast media (including IOCM and LOCM)
are also substantially lower than their high-osmolar
counterparts, with a reported incidence of 0.05% to
1.99% for nausea, and 0% to 0.36% for vomiting.[6]
Historically, since the days of HOCM use, fasting
has been practised prior to intravenous contrast
administration due to the established emetic side-effects
of HOCM, based on the hypothesis that there is higher
risk of vomiting with a full stomach and to reduce the
risk of aspiration pneumonia. This practice has not been
changed for more than two decades despite the shift to
IOCM and LOCM, until very recently. To date, it is still
a common practice to adopt a period of fasting prior to
contrast media administration before CT scan in Hong
Kong and worldwide.[7] [8]
There has been increasing recognition of the low risk of gastrointestinal side-effects resulting from IOCM and
LOCM administration irrespective of fasting time, as
well as trials abolishing the empirical implementation of
fasting prior to contrast CT. Lee et al[8] reviewed existing
literature and found no case of aspiration in 2001 patients
who underwent contrast CT with prior fluid intake. A
prospective observational study involving 110,836 cases
found no significant difference in the incidence of nausea
and vomiting between solid food non-fasting and fasting
groups.[9] Prospective randomised controlled trials, each
involving more than 2000 patients, were carried out in
both hospitalised patients and outpatients, and found no
significant difference in incidence of nausea and vomiting
between patients fasted for at least 4 hours and patients
without fasting, and no case of aspiration pneumonitis
was identified.[10] [11] There has been an additional report
of a statistically significant reduction in the incidence
of nausea after changing to a non-fasting policy in an
institution in Japan.[12]
Latest Guidelines on Preparatory Fasting
In 2018, the European Society of Urogenital Radiology
(ESUR) published their Guideline on Contrast Agents
(v10.0), which stated that ‘fasting is not recommended
before administration of low- or iso-osmolar non-ionic
iodine-based contrast media or of gadolinium-based
agents’.[13] Later and most recently in 2021, the American
College of Radiology (ACR) published their latest
Manual on Contrast Media, stating that ‘given the
potential for negative consequences due to fasting and
a lack of evidence that supports the need for fasting,
fasting is not required prior to routine intravascular
contrast material administration’, with additional special
consideration required for patients undergoing conscious
sedation.[14]
Local Practice
Currently in Prince of Wales Hospital, the contrast agents used include iohexol 300 and 350 (LOCM), and iodixanol
(IOCM), all of which have a well-established safety
profile and are known to have a low risk of nausea and
vomiting. As per department protocol of the Department
of Imaging and Interventional Radiology at Prince of
Wales Hospital, patients attending the department for
contrast-enhanced CT were previously required to fast
for at least 4 hours prior to study, unless in emergencies
or other limited special considerations. The fasting status
of hospitalised patients would be confirmed by the ward,
and outpatients would receive written instruction to fast
before the appointment.
A PRACTICAL APPROACH TO POLICY CHANGE: LOCAL EXPERIENCE
With the significant discrepancy between the fasting
policy between Prince of Wales Hospital and
international standards, we saw a pressing need to change
our clinical practice. In view of the potential impact
of policy change in terms of logistics, and potential
doubts or confusion from clinical departments in initial
implementation, we adopted a stepwise approach to
policy change, combined with ongoing data collection
to consolidate the local safety profile of contrast media
use under the new policy. The policy change was
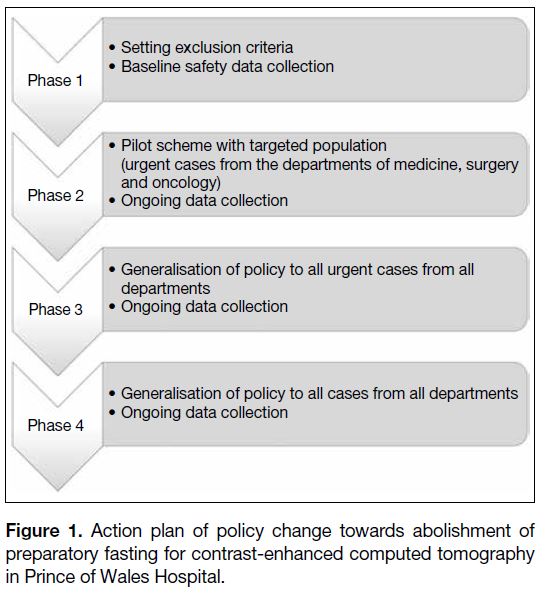
implemented in four phases (Figure 1).
Figure 1. Action plan of policy change towards abolishment of preparatory fasting for contrast-enhanced computed tomography in Prince of Wales Hospital.
Phase 1: Preparatory Phase
We reviewed the potential practical issues to the policy
change. While a generic implementation of the non-fasting
policy would be convenient, we saw that there
would be circumstances and specific indications where
fasting would still be required. As there was no clear
consensus statement or guideline detailing exclusion
criteria to non-fasting policy, we decided on a list
of exclusion criteria based on consensus opinion of
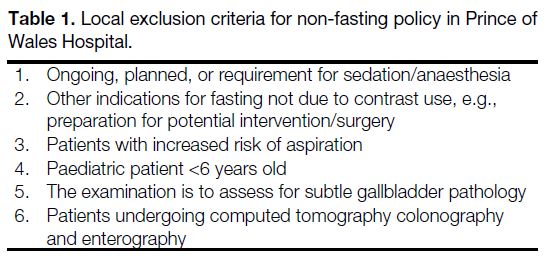
specialists from our local institutes (Table 1).
Table 1. Local exclusion criteria for non-fasting policy in Prince of Wales Hospital.
We gathered data on the fasting time and any occurrence
of vomiting after contrast scanning for the patients coming to the radiology department at Prince of Wales
Hospital for 25 working days through a questionnaire
filled in by attending radiographers and nurses. The
electronic patient record of the patients who experienced
vomiting and their available subsequent chest
radiographs were reviewed to identify any aspiration
pneumonia complications. This served to establish a
baseline of our performance and compile a local safety
profile of contrast media use for CT. After confirming
a comparable incidence of vomiting and aspiration
pneumonia to international published data, we proceeded
with our pilot scheme, continuing to collect data through
all four phases.
Phase 2: Pilot Scheme
We identified the departments of medicine, surgery
and oncology at Prince of Wales Hospital as the three
main sources of referrals to the radiology department
for contrast-enhanced CT. A pilot scheme was then
implemented with these three departments, during
which the referred eligible patients (i.e., those not
under the pre-set exclusion criteria) undergoing urgent
contrast-enhanced CT were not required to fast prior to
examination.
Phase 3: Generalisation of Non-fasting Policy
to Urgent Cases
Subsequent to the pilot scheme, which was well-received
with smooth operation, we proceeded with Phase 3,
which was generalisation of the non-fasting policy
to all urgent cases from all departments. The eligible
patients referred from all departments undergoing urgent
contrast-enhanced CT were not required to fast prior to
examination.
Phase 4: Generalisation of Non-fasting Policy
to All Cases
After allowing for a period of familiarisation of all
departments with the new policy, we entered Phase 4, extending the non-fasting policy to all cases, irrespective
of urgent or elective setting. Previously, all patients
booked for elective contrast-enhanced CT would receive
fasting instructions. After the new policy was enforced,
newly booked patients would no longer receive fasting
instructions unless they fell into the exclusion criteria.
No specific instructions were given to previously booked
patients who had an appointment date after the new
policy launch in order to avoid unnecessary confusion.
For previously booked patients who arrived for contrast-enhanced
CT without adequate fasting but who were not
required to fast under the new policy, the scans were
performed without delay.
Establishing a Local Safety Profile for Intravenous Contrast for Computed Tomography
The same duration (25 working days) and methods of
data collection (questionnaire, electronic patient record,
and chest radiograph review) were applied to Phases 2
through 4.
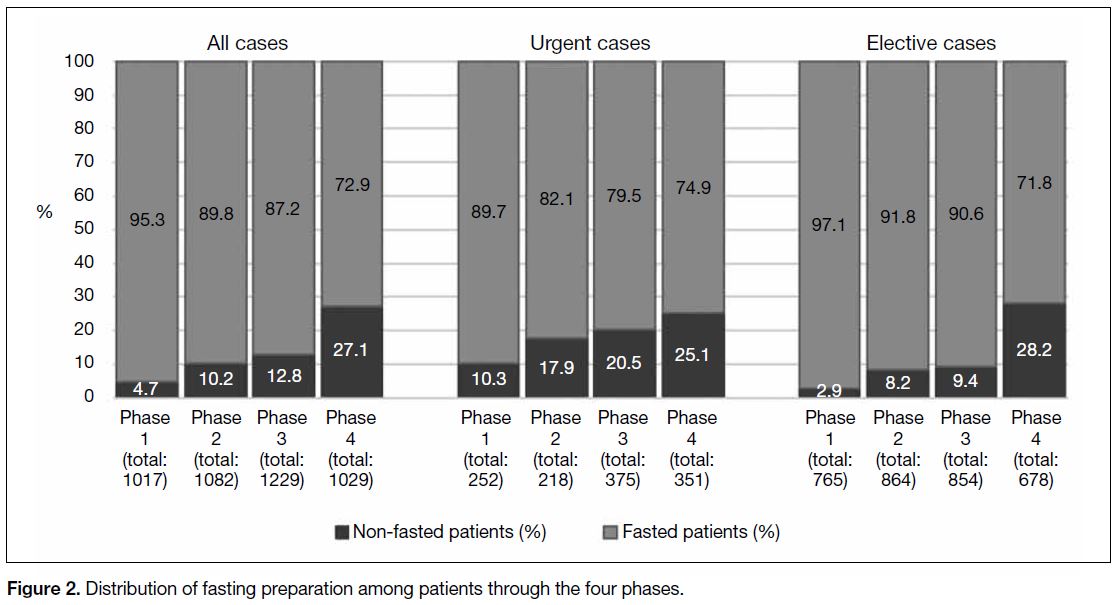
A total of 4357 attendances were recorded during our data collection through the four phases. There was a steady
increase in the proportion of non-fasted attendances
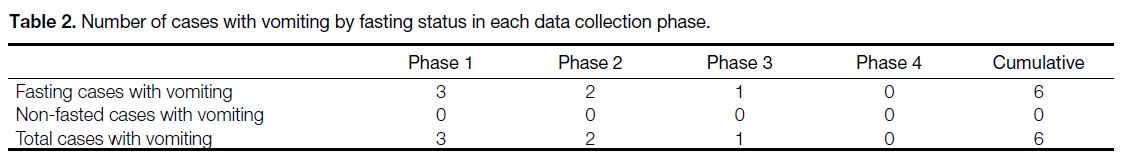
(Figure 2). The incidence of vomiting remained low.
There was a total of six patients who vomited (0.13%),
all of whom had fasted and did not have documented
clinical or radiological evidence of aspiration pneumonia.
A total of 594 patients were non-fasted and no vomiting
occurred (Table 2).
Figure 2. Distribution of fasting preparation among patients through the four phases.
Table 2. Number of cases with vomiting by fasting status in each data collection phase.
DISCUSSION
Internationally, there is a shifting paradigm towards
abolishment of routine preparatory fasting before
intravenous contrast administration for CT scans. The
recent updates in the ESUR guidelines and the ACR
contrast manual provide a clear new international
standard. There is also abundant evidence and
international data confirming the safety profile of use of
IOCM and LOCM, which are the agents used locally. Our
experience with converting to a non-fasting preparation
for contrast-enhanced CT is concordant with the findings of published studies, with a low incidence of vomiting
and no occurrence of aspiration pneumonia. From
a very early study by Oowaki et al[15] to a recent study
by Tsushima et al,[12] longer fasting times were found to
be associated with an increase in the adverse effect of
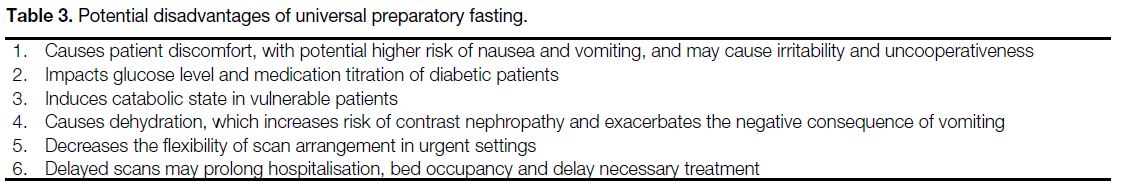
nausea.[15] There are a number of potential disadvantages
of universal preparatory fasting, which are summarised
in Table 3. Fasting creates patient discomfort, disturbs
nutritional balance in the weak, especially older
adult and oncology patients, and potentially causes
negative impact on diabetic control and medication
titration. Fasting may also create dehydration, which
is contradictory to the need of adequate hydration
for prevention of contrast nephropathy, and further
exacerbates the negative fluid balance should vomiting
occur. For inpatients, dehydration can be avoided by
administration of intravenous fluid. For outpatients,
however, intravenous fluid is not a reasonable option.
At an administrative level, the need for consideration of
fasting duration also reduces flexibility in appointment
arrangement. Empirical adherence to preparatory fasting
can lead to unnecessary delays in management, as well
as prolonged hospitalisation and bed occupancy. With
the compelling evidence, a change in local practice is
imperative.
Table 3. Potential disadvantages of universal preparatory fasting.
Practically, the implementation of the non-fasting
policy is not as simple as a one-off policy change, for
two main reasons. First, it is a deeply rooted concept
well-accepted by clinicians in Hong Kong that fasting
has a protective effect against contrast-induced emesis
and lowers the risk of aspiration pneumonia. It is also
a convenient practice as an admission order for the
majority of inpatients to avoid delay in investigations or
potential procedures. However, this practice is not in the
best interest of all patients, especially for the weak and
fragile. In our experience, many inpatients underwent
repeated episodes of prolonged fasting while waiting
for urgent contrast-enhanced CT examinations. Due to
rising demand despite limited resources, this would be
seen more frequently if the policy had not been changed.
Second, it is a general statement that fasting is no longer required prior to contrast administration. There are no
specific exclusion criteria stated by ESUR guidelines,
whereas the ACR manual on contrast media touched
upon that ‘for patients receiving conscious sedation,
anaesthesia guidelines should be consulted’.[13] [14] Despite
the lack of specific instructions, it is imaginable that there
are specific scenarios where fasting may be necessary or
have added benefits. We devised our set of exclusion
criteria locally based on the consensus opinion of our
institutes’ specialists (Table 1). Each institution may
consider a variation of the exclusion criteria tailored to
the demographics of their patients. Our exclusion criteria
have two main bases: (1) There are patients at higher risk
of aspiration; and (2) There are specific needs for fasting
for image optimisation and interpretation.
Specific to certain risk groups, fasting may still be
required. Adding to the ACR manual’s note on patients
undergoing conscious sedation, we expanded the
exclusion to all patients receiving sedation/anaesthesia in
accordance with anaesthesia guidelines for preoperative
fasting, and for those expecting or potentially requiring
sedation/anaesthesia in order to avoid potential delay in
management. A similar rationale was used for patients
expecting to undergo intervention or surgery. On the
other hand, there is a group of patients who are inherently
at higher risk of aspiration, e.g., those with bulbar palsy
with impaired gag reflexes, and those with impaired
consciousness levels. In these groups, the preparatory
fasting aims mainly to reduce the volume of aspirate
should the rare event of vomiting occur, as they are more
vulnerable to the aftermath of vomiting. Another group of
patients requiring special consideration is the paediatric
population. ESUR guidelines[13] and the ACR contrast
manual[14] did not specify a need for special consideration
for the paediatric population. Compared with the adult
population, there are, however, fewer published data
evaluating the risk of vomiting with contrast media use.
A small study by Ha et al[16] involving 864 patients aged
from 1 day to 19 years (mean age = 8.4 ± 5.7 years) found the incidence of vomiting was 2.1% in the study group
with no occurrence of aspiration pneumonia. In Prince
of Wales Hospital, we used the age of 6 years as a cut-off
for the need for fasting in the paediatric population,
based on the need for sedation prior to CT for patients
under this age as suggested by our paediatric radiologist.
Specific to the potential impact on image interpretation,
there has not been any specific dedicated study to
evaluate the effect of a non-fasting policy on image
quality. The gallbladder is known to distend with
fasting, which may allow for better evaluation of
subtle gallbladder pathology, e.g., small polyps. Gross
changes in the gallbladder, e.g., acute cholecystitis,
do not require fasting preparation for assessment. In
addition, the duration of fasting may not necessarily
correlate with the degree of gallbladder distension. We
therefore only limited exclusion to indications to look
for subtle gallbladder pathology. CT enterography and
colonography require bowel preparation for optimal
image quality and accurate image interpretation and
were therefore excluded from the non-fasting policy.
So far, with these exclusion criteria in place, we did not
encounter any case where the interpretation has been
hindered by the non-fasting state.
Combining international guidelines and local consensus
opinion, we have implemented the non-fasting policy to
all patients undergoing iodinated contrast-enhanced CT
examinations in the radiology department with a set of
limited exclusion criteria. Through a stepwise approach,
we allowed time for adaptation and familiarisation by
the clinical departments, and the policy has been met
with a positive response with smooth transition. To our
knowledge, preparatory fasting is still practised in many
local institutions. We hope to advocate the implementation
of a non-fasting policy for eligible patients across centres
in order to provide patient-centred and evidence-based
care, adhering to international standards.
CONCLUSION
Non-fasting contrast-enhanced CT is a safe and
internationally recognised practice supported by evidence
and international guidelines. Our experience showed a
comparable safety profile with that of published studies
in terms of low incidence of vomiting and aspiration
pneumonia. Policy implementation is achievable through
a stepwise approach with need for consideration of pre-set
exclusion criteria.
REFERENCES
1. Schulz RA, Stein JA, Pelc NJ. How CT happened: the early development of medical computed tomography. J Med Imaging (Bellingham). 2021;8:052110. Crossref
2. Nyman U, Ekberg O, Aspelin P. Torsten Almén (1931–2016): the father of non-ionic iodine contrast media. Acta Radiol. 2016;57:1072-8. Crossref
3. Bush WH, Swanson DP. Acute reactions to intravascular contrast
media: types, risk factors, recognition, and specific treatment. AJR
Am J Roentgenol. 1991;157:1153-61. Crossref
4. Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P,
Matsuura K. Adverse reactions to ionic and nonionic contrast
media. A report from the Japanese Committee on the Safety of
Contrast Media. Radiology. 1990;175:621-8. Crossref
5. Hunt CH, Hartman RP, Hesley GK. Frequency and severity of
adverse effects of iodinated and gadolinium contrast materials:
retrospective review of 456,930 doses. AJR Am J Roentgenol.
2009;193:1124-7. Crossref
6. Kim YS, Yoon SH, Choi YH, Park CM, Lee W, Goo JM. Nausea
and vomiting after exposure to non-ionic contrast media: incidence
and risk factors focusing on preparatory fasting. Br J Radiol.
2018;91:20180107. Crossref
7. Liu H, Liu Y, Zhao L, Li X, Zhang W. Preprocedural fasting for
contrast-enhanced CT: when experience meets evidence. Insights
Imaging. 2021;12:180. Crossref
8. Lee BY, Ok JJ, Abdelaziz Elsayed AA, Kim Y, Han DH. Preparative fasting for contrast-enhanced CT: reconsideration.
Radiology. 2012;263:444-50. Crossref
9. Li X, Liu H, Zhao L, Liu J, Cai L, Zhang L, et al. The effect of
preparative solid food status on the occurrence of nausea, vomiting
and aspiration symptoms in enhanced CT examination: prospective
observational study. Br J Radiol. 2018;91:20180198. Crossref
10. Neeman Z, Abu Ata M, Touma E, Saliba W, Barnett-Griness O, Gralnek IM, et al. Is fasting still necessary prior to contrast-enhanced computed tomography? A randomized clinical study.
Eur Radiol. 2020;31:1451-9. Crossref
11. Barbosa PN, Bitencourt AG, Tyng CJ, Cunha R, Travesso DJ, Almeida MF, et al. Journal club: preparative fasting for contrast-enhanced CT in a cancer center: a new approach. AJR Am J
Roentgenol. 2018;210:941-7. Crossref
12. Tsushima Y, Seki Y, Nakajima T, Hirasawa H, Taketomi-Takahashi
A, Tan S, et al. The effect of abolishing instructions to fast prior to
contrast-enhanced CT on the incidence of acute adverse reactions.
Insights Imaging. 2020;11:113. Crossref
13. European Society of Urogenital Radiology. Guidelines on Contrast
Agents. 10th ed. Available from: https://adus-radiologie.ch/files/ESUR_Guidelines_10.0.pdf. Accessed 5 Jun 2023.
14. ACR Committee on Drugs and Contrast Media. American College of Radiology. ACR Manual on Contrast Media. 2023. Available from: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf. Accessed 16 Apr 2021.
15. Oowaki K, Saigusa H, Ojiri H, Ariizumi M, Yamagisi J, Fukuda K, et al. Relationship between oral food intake and
nausea caused by intravenous injection of iodinated contrast
material [in Japanese]. Nihon Igaku Hoshasen Gakkai Zasshi.
1994;54:476-9.
16. Ha JY, Choi YH, Cho YJ, Lee S, Lee SB, Choi G, et al. Incidence
and risk factors of nausea and vomiting after exposure to lowosmolality
iodinated contrast media in children: a focus on
preparative fasting. Korean J Radiol. 2020;21:1178-86. Crossref