Imaging Features of Clavicular Pathologies and Their Articulations: A Pictorial Essay
PICTORIAL ESSAY CME
Hong Kong J Radiol 2025 Jun;28(2):e111-27 | Epub 17 June 2025
Imaging Features of Clavicular Pathologies and Their Articulations: A Pictorial Essay
BWT Cheng, JHM Cheng, KH Chin, CY Chu
Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Correspondence: Dr BWT Cheng, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China. Email: cwt413@ha.org.hk
Submitted: 10 January 2024; Accepted: 1 November 2024.
Contributors: BWTC and JHMC designed the study. BWTC, JHMC and KHC acquired the data. All authors analysed the data. BWTC drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: The study was approved by the Central Institutional Review Board of Hospital Authority, Hong Kong (Ref No.: CIRB-2023-btained from the Board due to the retrospective nature of the study.
INTRODUCTION
The clavicle, the acromioclavicular (AC) joint and the
sternoclavicular joint can be affected by a wide range
of pathologies, including infection, inflammation,
degeneration, metabolic disorders, neoplasms, trauma,
and congenital anomalies. This pictorial essay illustrates
the radiological features of clavicular pathologies to
facilitate accurate diagnosis and management, based on
cases of clavicular, AC and sternoclavicular pathologies
diagnosed in the Hong Kong East Cluster from April
2014 to April 2023.
NORMAL ANATOMY
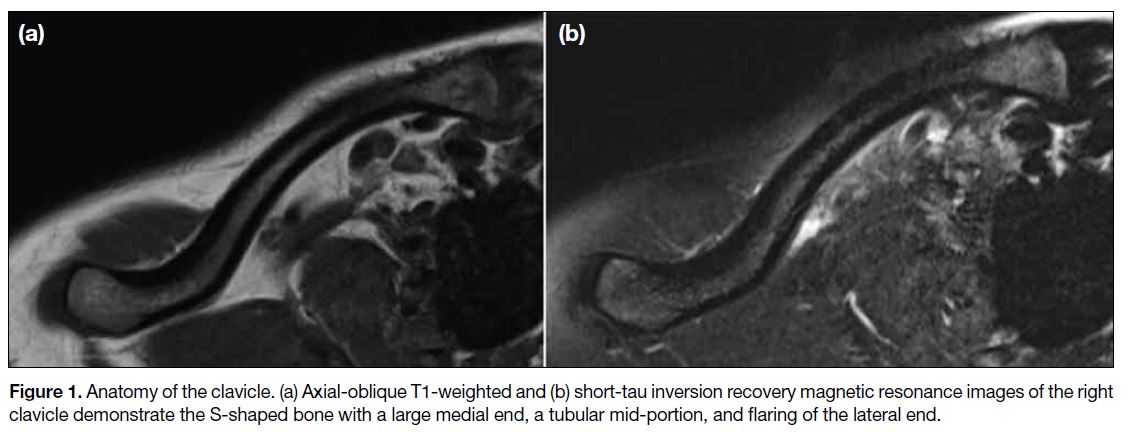
A basic understanding of the anatomy of the clavicle
and its articulations is essential for image interpretation.
The clavicle is a horizontally oriented S-shaped bone
that has a large medial metaphysis articulating with
the sternum, a tubular diaphysis, and a flared lateral
metaphysis that articulates with the acromion (Figure 1). The sternoclavicular joint is a synovial joint formed
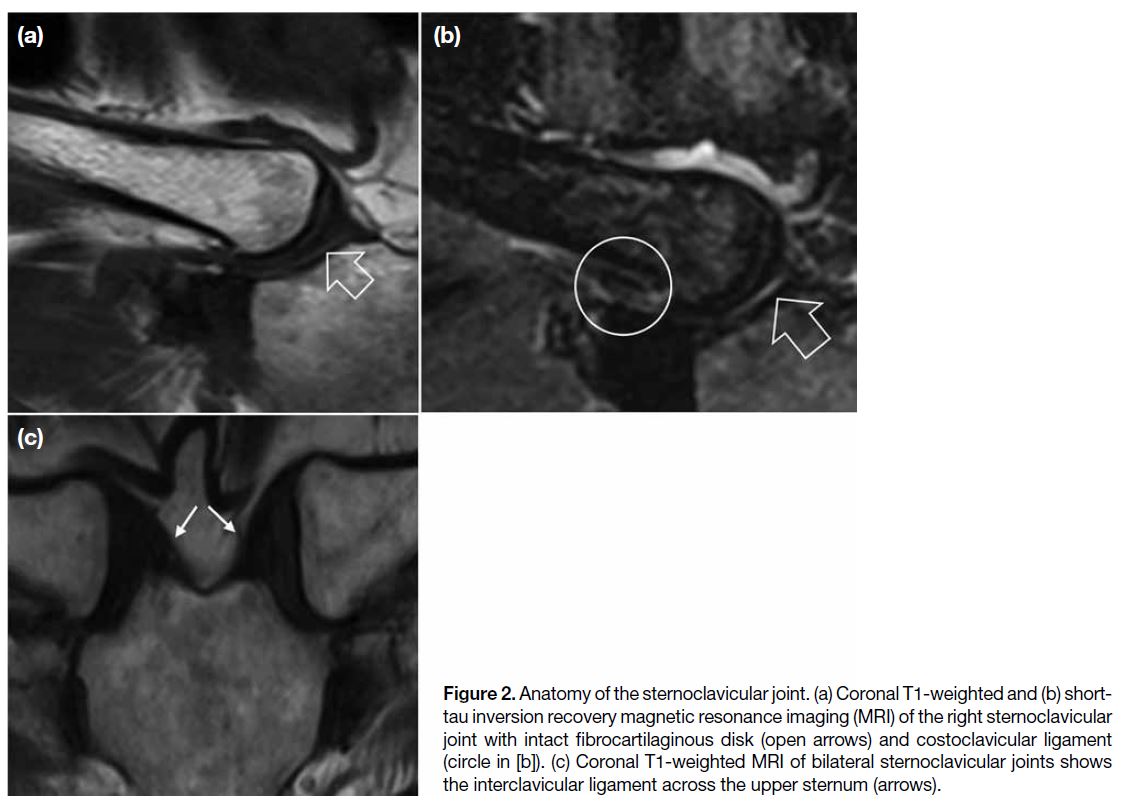
by the medial clavicular metaphysis, the clavicular
notch of the manubrium sterni, and the cartilage of the first rib. The articular surfaces of the clavicle and
manubrium are separated by a fibrocartilaginous disk.[1]
The costoclavicular and sternoclavicular ligaments
(thickenings of the joint capsule), and interclavicular
ligament (located between the superomedial ends of the two
clavicles) provide joint stability (Figure 2).[2] The AC
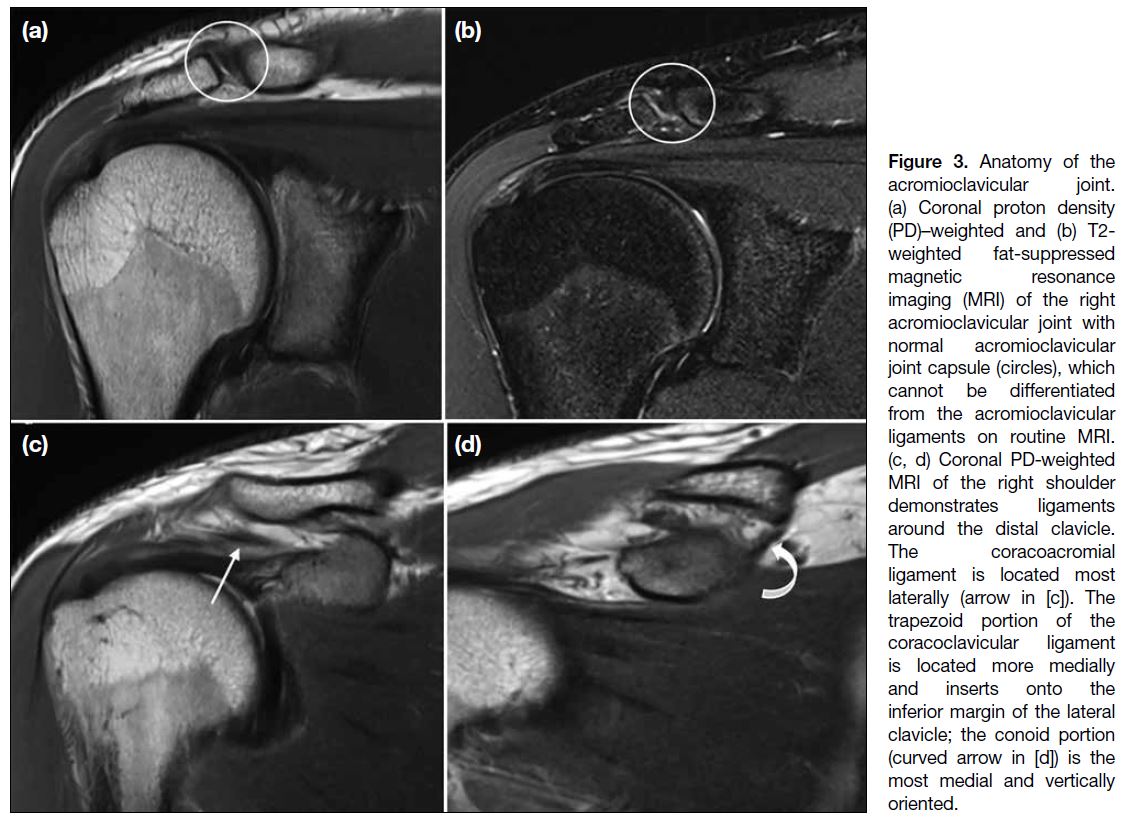
joint is a planar diarthrodial joint located between the
lateral surface of the clavicle and the medial surface
of the acromion. Stabilisers of the joint include the
AC joint capsule and the AC, coracoacromial, and
coracoclavicular (consisting of trapezoid and conoid
ligaments) ligaments. A flexible fibrocartilaginous disk
is peripherally continuous with the joint capsule (Figure 3).[3] There are four types of acromion shape, namely,
flat, curved, hooked, and convex. An unfused acromial
ossification centre (os acromiale) is an anatomical
variant.
Figure 1. Anatomy of the clavicle. (a) Axial-oblique T1-weighted and (b) short-tau inversion recovery magnetic resonance images of the right clavicle demonstrate the S-shaped bone with a large medial end, a tubular mid-portion, and flaring of the lateral end.
Figure 2. Anatomy of the sternoclavicular joint. (a) Coronal T1-weighted and (b) short-tau
inversion recovery magnetic resonance imaging (MRI) of the right sternoclavicular joint with intact fibrocartilaginous disk (open arrows) and costoclavicular ligament (circle in [b]). (c) Coronal T1-weighted MRI of bilateral sternoclavicular joints shows the interclavicular ligament across the upper sternum (arrows).
Figure 3. Anatomy of the
acromioclavicular joint. (a) Coronal proton density
(PD)–weighted and (b) T2-weighted fat-suppressed
magnetic resonance imaging (MRI) of the right acromioclavicular joint with normal acromioclavicular joint capsule (circles), which
cannot be differentiated from the acromioclavicular ligaments on routine MRI. (c, d) Coronal PD-weighted MRI of the right shoulder demonstrates ligaments around the distal clavicle. The coracoacromial ligament is located most laterally (arrow in [c]). The trapezoid portion of the coracoclavicular ligament is located more medially and inserts onto the inferior margin of the lateral clavicle; the conoid portion (curved arrow in [d]) is the most medial and vertically oriented.
RADIOLOGICAL FEATURES OF PATHOLOGIES
Congenital Anomalies
Cleidocranial dysostosis is a rare autosomal dominant disease that mainly affects midline skeletal structures,
with features including hypoplasia or aplasia of the
clavicles, large fontanelles, multiple Wormian bones, a widened pubic symphysis, and supernumerary teeth
(Figure 4). Eight cases of cleidocranial dysostosis were
identified during the review period.
Figure 4. A case of cleidocranial dysostosis. (a) Chest X-ray demonstrates aplasia of bilateral clavicles (ellipse). (b) Pelvic X-ray demonstrates
widening of pubic symphysis (arrowheads). Frontal (c) and lateral (d) skull X-rays demonstrate widened sagittal suture (open arrows in [c])
and multiple Wormian bones (arrows in [d]). (e) Orthopantomogram demonstrates supernumerary teeth.
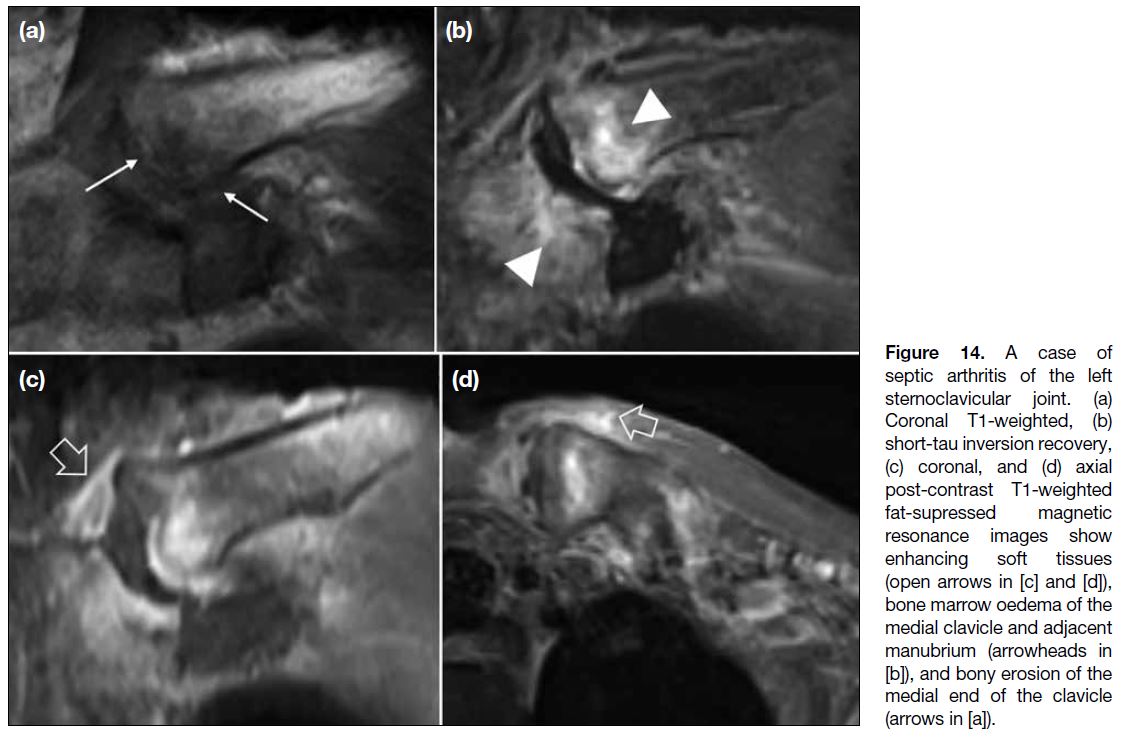
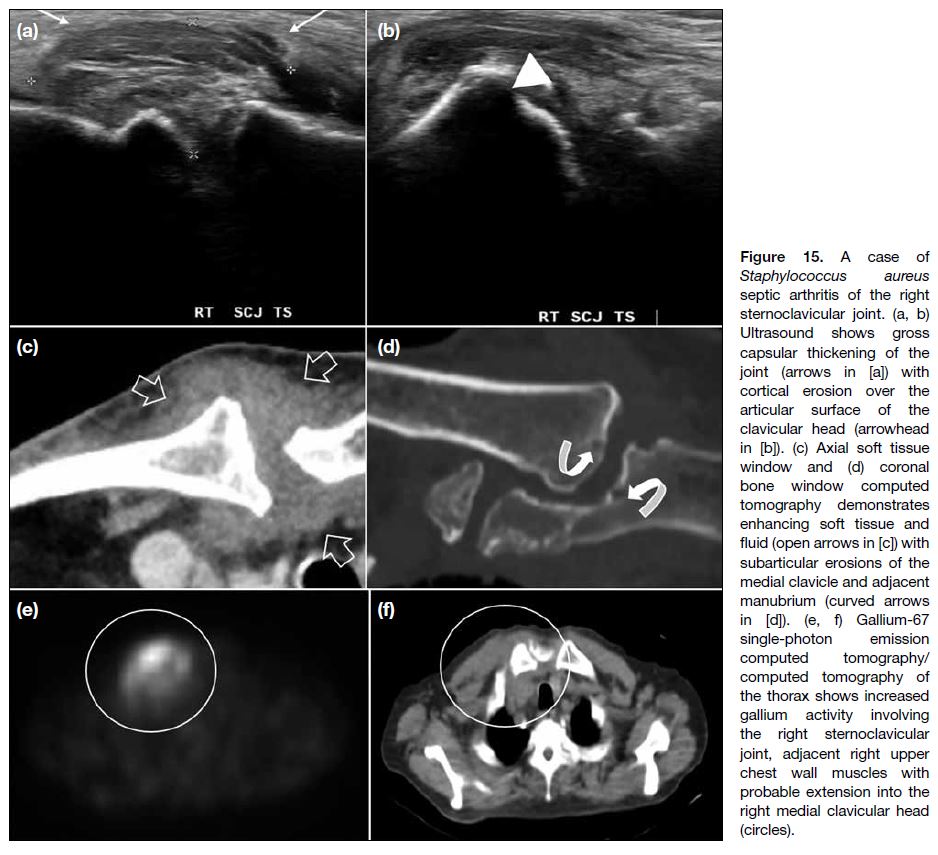
Articular Infection
Septic arthritis of the sternoclavicular joint is uncommon
and is usually monoarticular with an insidious onset.[4]
Radiological features on radiographs and computed
tomography (CT) include subarticular erosions, joint
space widening, and fluid collections. Magnetic
resonance imaging (MRI) features include bone
marrow oedema, bone destruction, joint effusion, and
inflammatory changes of the surrounding soft tissue.
Both CT and MRI are useful for early diagnosis
and assessment of complications such as associated
osteomyelitis and retrosternal/chest wall abscesses that
may require surgical treatment.
Inflammation
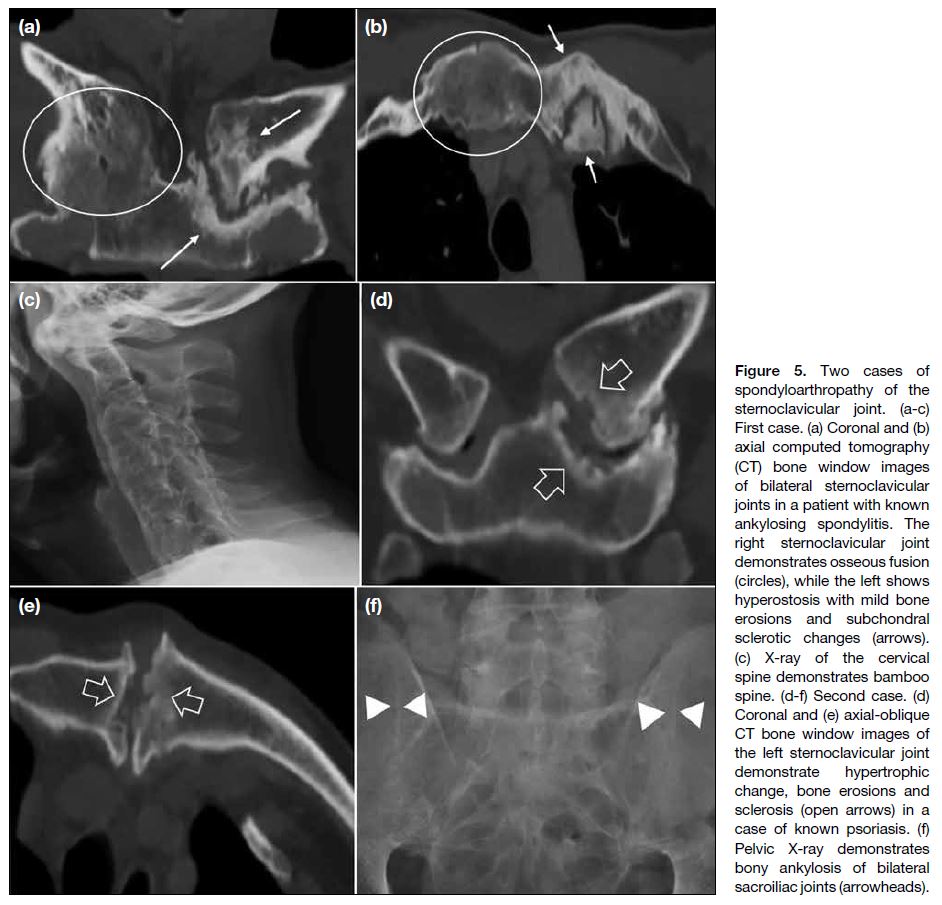
Spondyloarthropathies such as ankylosing spondylitis
and psoriasis can affect the sternoclavicular joint.
Radiographic and CT features include bone erosions, partial or complete fusion of the joint, and hyperostosis
surrounding the joint[2] (Figures 5, 6 and 7). Rheumatoid arthritis
may be accompanied by pannus formation with bony
erosions on imaging.
Figure 5. Two cases of
spondyloarthropathy of the sternoclavicular joint. (a-c) First case. (a) Coronal and (b) axial computed tomography (CT) bone window images of bilateral sternoclavicular joints in a patient with known ankylosing spondylitis. The right sternoclavicular joint demonstrates osseous fusion (circles), while the left shows hyperostosis with mild bone erosions and subchondral sclerotic changes (arrows). (c) X-ray of the cervical spine demonstrates bamboo spine. (d-f) Second case. (d) Coronal and (e) axial-oblique CT bone window images of the left sternoclavicular joint demonstrate hypertrophic change, bone erosions and sclerosis (open arrows) in a case of known psoriasis. (f) Pelvic X-ray demonstrates bony ankylosis of bilateral sacroiliac joints (arrowheads).
Figure 6. Two cases of the SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome. (a, b) First case. (a) Radiograph of
the clavicles demonstrates prominent hyperostosis in both sternoclavicular joints (circle), more on the right, and sclerosis in both distal
clavicles (arrows). (b) Bone scintigraphy demonstrates diffusely increased tracer uptake in both sternocostoclavicular junctions and
medial clavicular ends (open arrows), associated with hyperostosis, compatible with the ‘bull’s head’ sign. (c-e) Second case. (c) X-ray
demonstrates hyperostosis of both medial clavicles (circle). A Ryles tube is noted (arrowheads). (d) Coronal and (e) axial bone window
computed tomography images demonstrate corresponding significant sternoclavicular hyperostosis (open arrows in [e]), marked joint
space narrowing on the right with cortical irregularities (arrowheads in [d]) and complete ankylosis on the left (arrows in [d]).
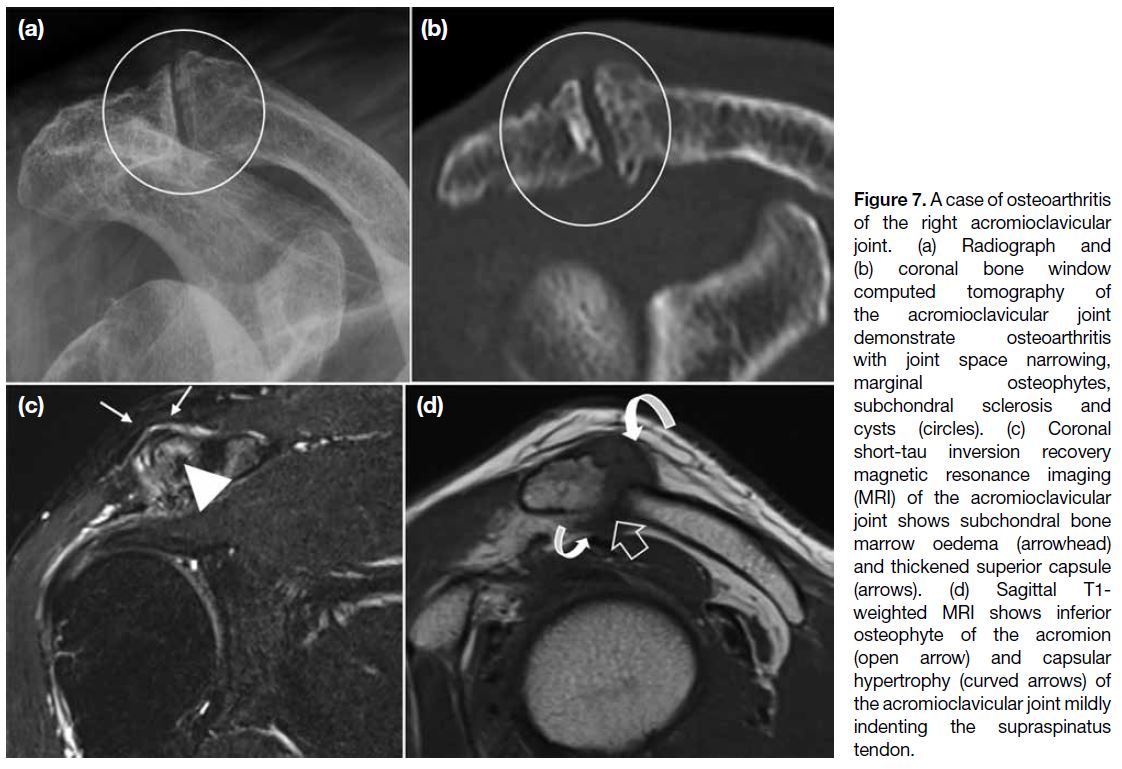
Figure 7. A case of osteoarthritis of the right acromioclavicular joint. (a) Radiograph and (b) coronal bone window computed tomography of the acromioclavicular joint demonstrate osteoarthritis with joint space narrowing, marginal osteophytes, subchondral sclerosis and cysts (circles). (c) Coronal short-tau inversion recovery magnetic resonance imaging (MRI) of the acromioclavicular joint shows subchondral bone marrow oedema (arrowhead) and thickened superior capsule (arrows). (d) Sagittal T1-weighted MRI shows inferior osteophyte of the acromion (open arrow) and capsular hypertrophy (curved arrows) of the acromioclavicular joint mildly indenting the supraspinatus tendon.
The SAPHO (synovitis, acne, pustulosis, hyperostosis,
and osteitis) syndrome is an inflammatory condition with
aseptic osteoarticular involvement and characteristic skin
lesions. In adults, it usually involves the anterior chest
wall (60%-95%), particularly the sternocostoclavicular
junction, followed by the axial skeleton, such as the spine
and sacroiliac joints. Features of SAPHO on radiographs
and CT include bony sclerosis, cortical thickening,
and narrowing of the medullary canal. Adjacent
changes include joint space narrowing and periarticular
osteopenia, as well as ligamentous ossification with bony
bridging across the joint. CT is good for detecting the
osteoarticular manifestations, while MRI is sensitive in detecting early disease with bone and soft tissue oedema.
On bone scintigraphy, SAPHO in the anterior chest wall
typically manifests as the ‘bull’s head’ sign, with mostly
symmetrical increased uptake in the sternoclavicular
regions.[5] The radiological differential diagnosis includes
sternoclavicular osteoarthritis, condensing osteitis of the
clavicle, osteonecrosis, and septic arthritis (Figure 6).
Six cases of SAPHO were identified during the review
period.
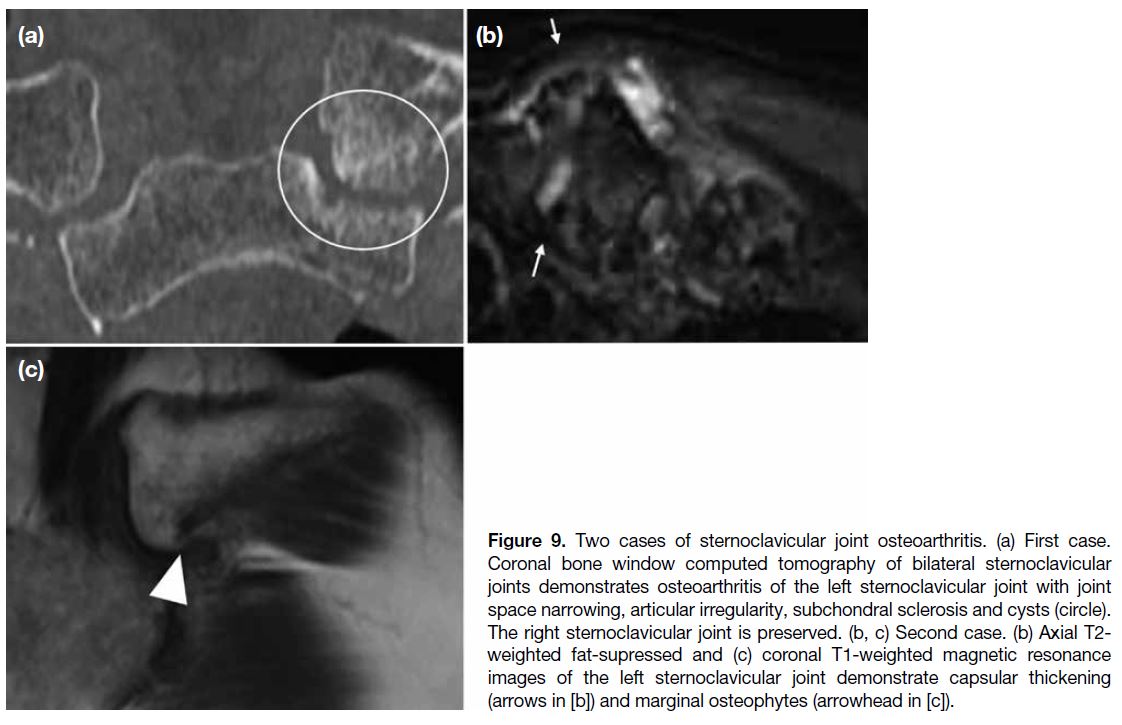
Degenerative Joint Disease
Osteoarthritis is a common cause of pain at the AC
and sternoclavicular joints (Figures 7, 8 and 9). Radiological
features include narrowing of the joint space, marginal
osteophytes, capsular hypertrophy, subchondral
sclerosis, cysts, and bone marrow oedema.
Figure 8. Two cases of complete chronic supraspinatus tear with geyser sign. (a-d) First case. (a) Radiograph shows a soft tissue shadow
(arrows) above the acromioclavicular joint with mild osteoarthritic change. Superior migration of the humeral head and subacromial
acetabularisation are noted, highly suggestive of chronic supraspinatus tear. (b) Transverse ultrasound demonstrates a cystic lesion with
low-level echoes above the acromioclavicular joint (white star). Corresponding coronal (c) and sagittal (d) T2-weighted fat-supressed
magnetic resonance images show complete supraspinatus tendon tear (open arrows in [c]) with uncovering and superior migration of the
humeral head, disrupted inferior capsule (circle in [c]), and a well-defined homogenous cystic lesion resembling the geyser sign (black
stars). Incidental findings include a subcortical bone cyst (arrowhead in [c]) and enchondroma (curved arrow in [d]) at the humeral head. (e,
f) Second case. (e) Axial and (f) coronal T1-weighted fat-supressed volumetric interpolated breath-hold examination magnetic resonance
arthrogram images of the right shoulder demonstrate a full-thickness tear of the supraspinatus-infraspinatus interdigitation (circle in [f]) with
superior migration of the humeral head. There is contrast extension via the subacromial subdeltoid bursa to the acromioclavicular joint
(arrows).
Figure 9. Two cases of sternoclavicular joint osteoarthritis. (a) First case.
Coronal bone window computed tomography of bilateral sternoclavicular
joints demonstrates osteoarthritis of the left sternoclavicular joint with joint space narrowing, articular irregularity, subchondral sclerosis and cysts (circle). The right sternoclavicular joint is preserved. (b, c) Second case. (b) Axial T2-weighted fat-supressed and (c) coronal T1-weighted magnetic resonance images of the left sternoclavicular joint demonstrate capsular thickening (arrows in [b]) and marginal osteophytes (arrowhead in [c]).
A chronic large full-thickness supraspinatus tendon
tear can lead to superior migration of the humeral head, which may erode the subacromial-subdeltoid bursa and
inferior AC capsule, forming a communication between
the glenohumeral and AC joints. This may lead to a
sizeable fluid pouch over the AC joint, giving rise to
the geyser sign (Figure 8). During the review period, six
such cases were identified.
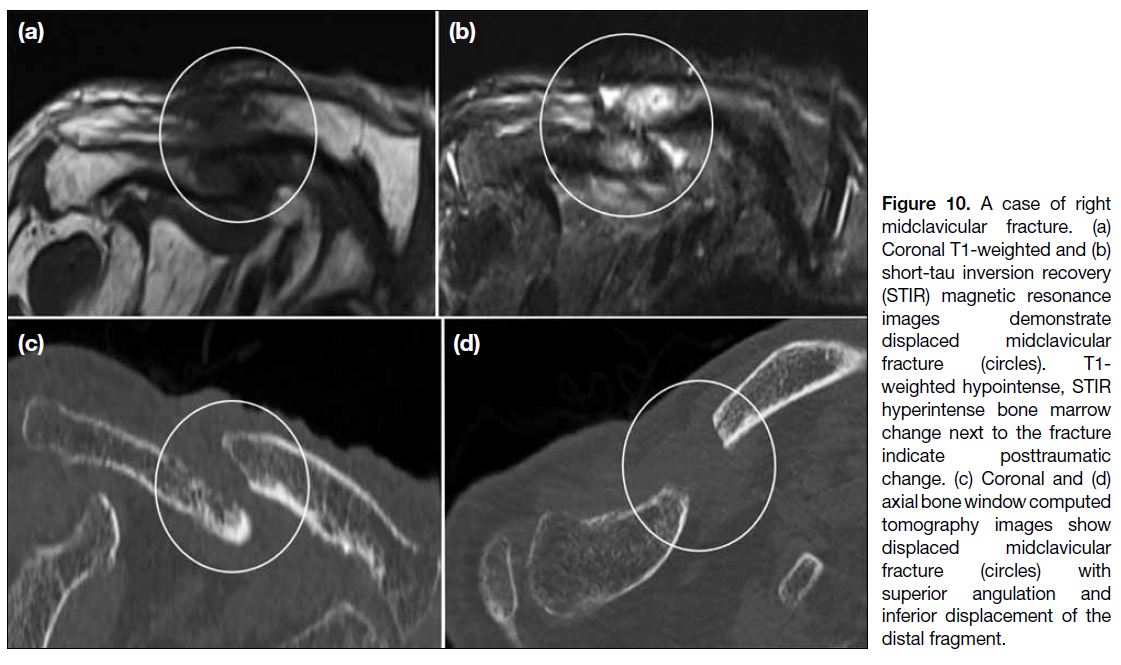
Trauma
Clavicular fractures (Figures 10, 11 and 12) are common and
represent 2.6% to 5% of all fractures, with the vast
majority occurring in the mid clavicle (69%-82%).[6]
Apart from location, alignment of the clavicle with
the AC and sternoclavicular joints should be assessed,
since malalignment may signify significant ligamentous
injury.
Figure 10. A case of right
midclavicular fracture. (a) Coronal T1-weighted and (b) short-tau inversion recovery (STIR) magnetic resonance images demonstrate displaced midclavicular fracture (circles). T1-weighted hypointense, STIR hyperintense bone marrow change next to the fracture indicate posttraumatic change. (c) Coronal and (d) axial bone window computed tomography images show displaced midclavicular fracture (circles) with superior angulation and inferior displacement of the distal fragment.
Figure 11. Two cases of acromioclavicular joint injury. (a-d) First case. (a)
Radiograph of the left acromioclavicular joint demonstrates slight superior displacement of the clavicle (arrows). (b-d) Sagittal and coronal T2-weighted fat-suppressed magnetic resonance imaging (MRI) of the left shoulder demonstrates increased signal in the coracoclavicular ligament (circle) and acromioclavicular ligament/joint capsule (open arrows), suggestive of Rockwood type II left acromioclavicular joint injury. (e-g) Second case. (e, f) Radiographs of the right acromioclavicular joint show markedly elevated clavicle with increased coracoclavicular distance, consistent with Rockwood type V right acromioclavicular joint injury. (g) Post–open reduction radiograph shows satisfactory joint alignment.
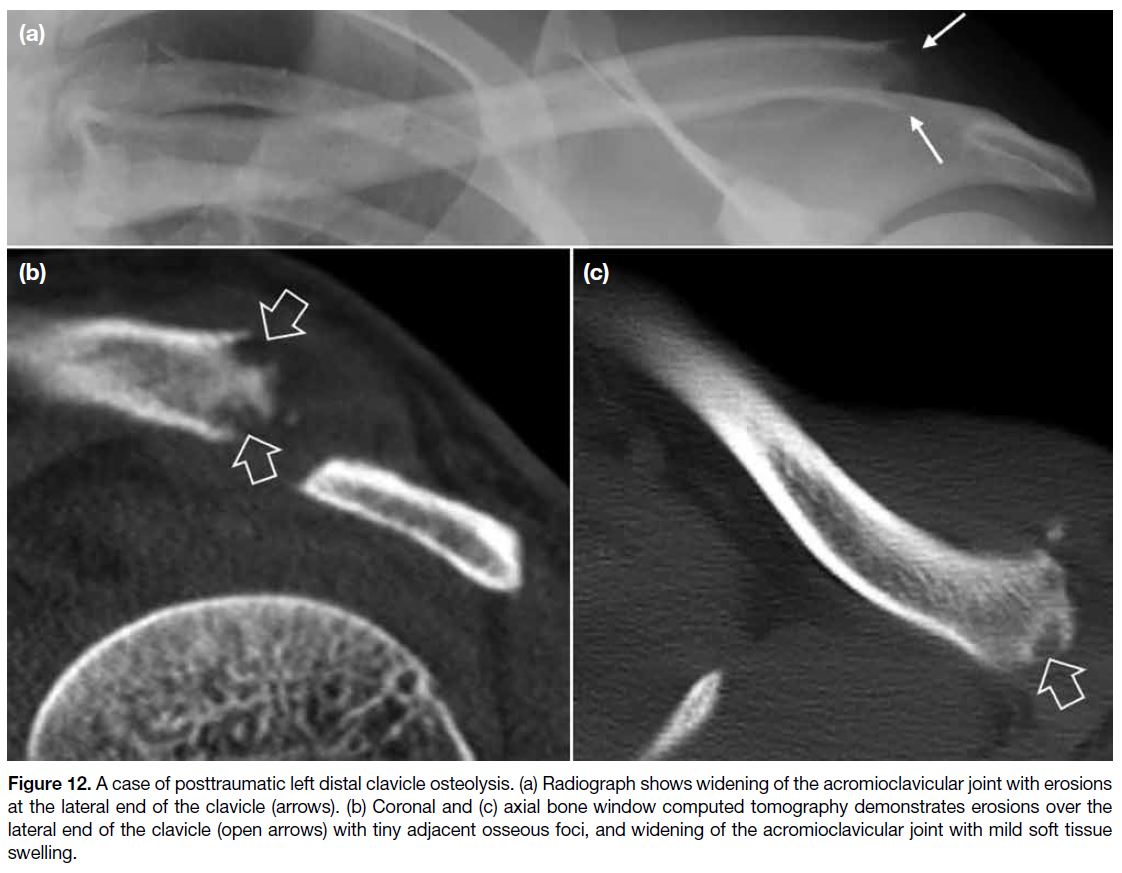
Figure 12. A case of posttraumatic left distal clavicle osteolysis. (a) Radiograph shows widening of the acromioclavicular joint with erosions
at the lateral end of the clavicle (arrows). (b) Coronal and (c) axial bone window computed tomography demonstrates erosions over the
lateral end of the clavicle (open arrows) with tiny adjacent osseous foci, and widening of the acromioclavicular joint with mild soft tissue
swelling.
AC joint injury is a common injury, occurring in 9% to
12% of shoulder injuries. The Rockwood classification is the most widely used classification system for AC joint
injuries. It is classified into six types, depending on the
direction and degree of clavicular displacement, which
correlates with the severity of injury and involvement
of the AC and coracoclavicular ligaments, and the
deltotrapezial complex (Table).
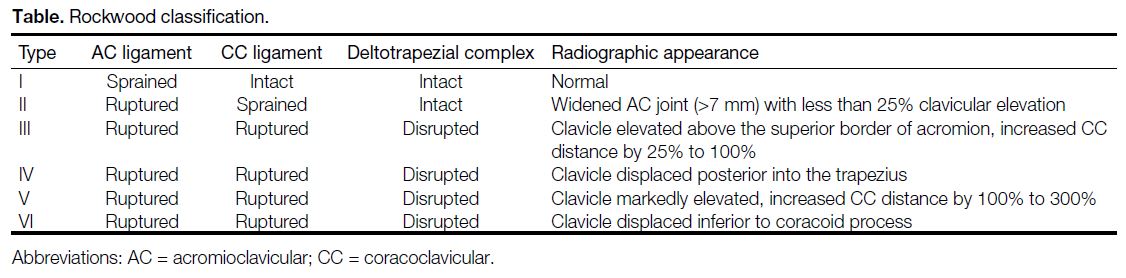
Table. Rockwood classification.
Sternoclavicular joint dislocations are classified as
anterior or posterior, and posterior dislocation has
potentially serious complications due to the risk of injury
to mediastinal structures such as the trachea and great
vessels. On non-rotated radiographs, a difference in the
relative craniocaudal positions of the medial clavicles
exceeding 50% of the width of the clavicular heads
suggests dislocation. However, diagnosis by radiographs
may be difficult due to anatomical superimposition. CT
is required for definitive diagnosis and to assess potential
mediastinal injury.
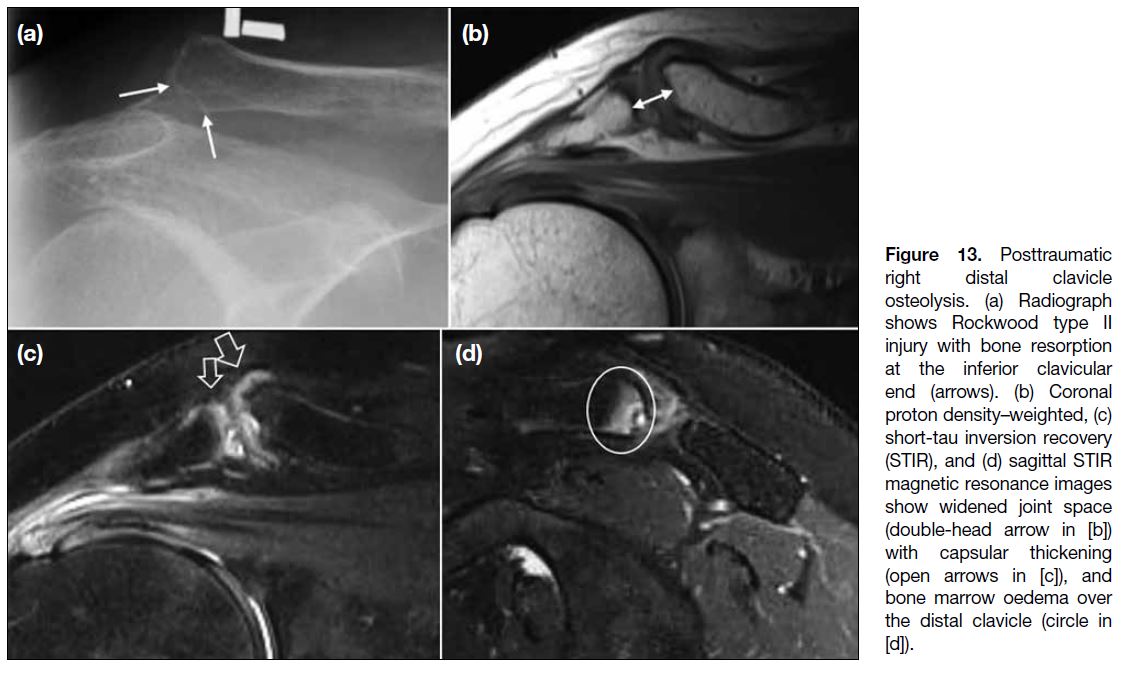
Distal Clavicle Osteolysis
Distal clavicle osteolysis (Figure 13) is painful bone
resorption of the distal clavicle, most common in young
adults with male predominance. It can be categorised into
posttraumatic or overuse forms, which share identical
imaging findings. Radiological features on radiographs and CT include cortical irregularity, ‘flame-shaped’
bony resorption, and subchondral cysts involving the
distal clavicle. MRI is most sensitive in demonstrating
clavicular marrow oedema in the early phase of the
disease. Effusion and capsular oedema are other features
on MRI.
Figure 13. Posttraumatic
right distal clavicle osteolysis. (a) Radiograph shows Rockwood type II injury with bone resorption at the inferior clavicular end (arrows). (b) Coronal proton density–weighted, (c) short-tau inversion recovery (STIR), and (d) sagittal STIR magnetic resonance images show widened joint space (double-head arrow in [b]) with capsular thickening (open arrows in [c]), and bone marrow oedema over the distal clavicle (circle in [d]).
The differential diagnoses of distal clavicle erosion
include rheumatoid arthritis, hyperparathyroidism, and
scleroderma.
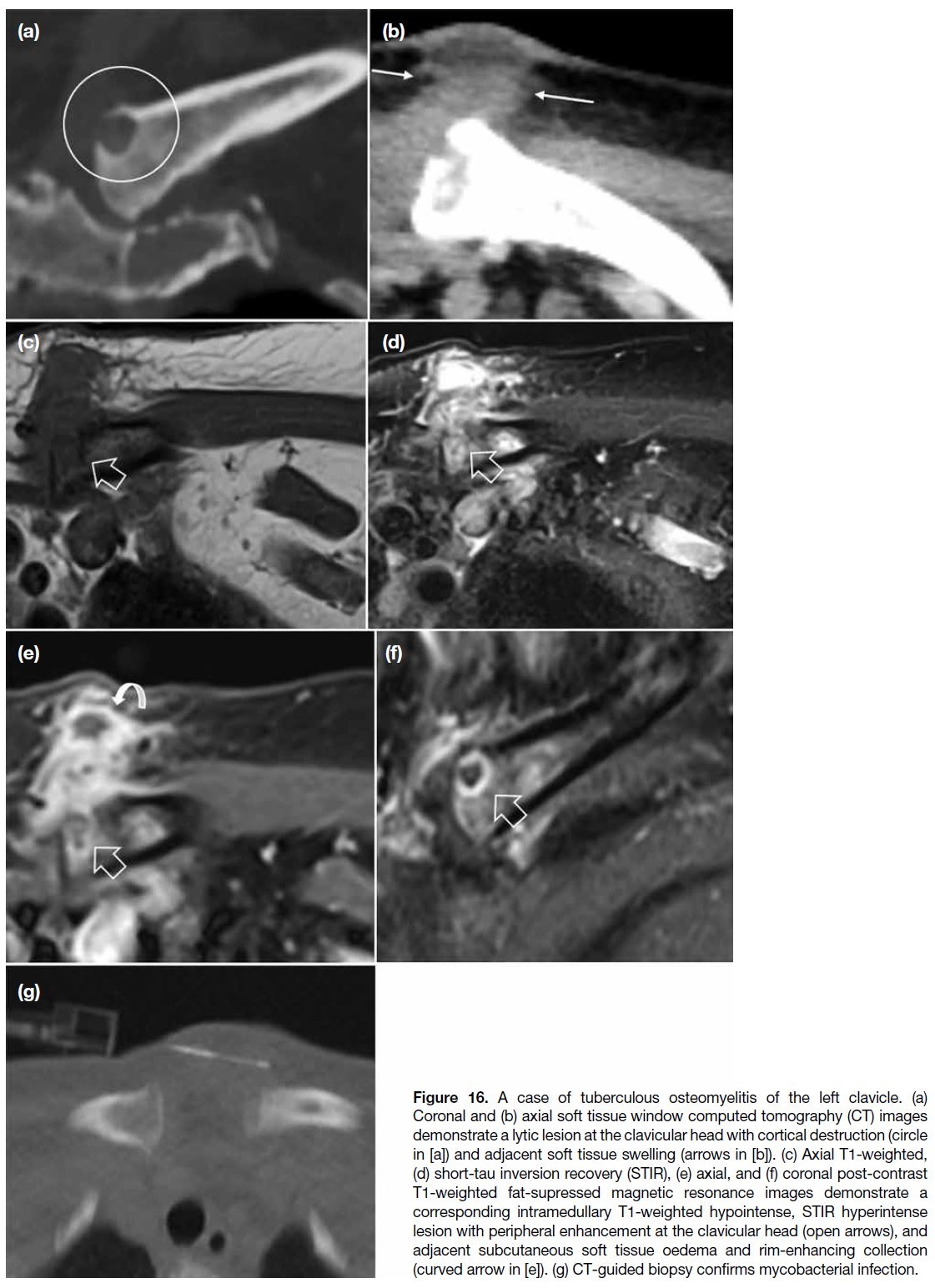
Non-Articular Infection
Radiological features of clavicular osteomyelitis on
radiographs and CT include cortical erosion, regional
osteopenia, periosteal reaction, and adjacent soft
tissue swelling (Figures 14, 15 and 16). On MRI, features of
osteomyelitis typically include bone marrow oedema
and surrounding soft tissue inflammatory change or collection. With time, an intraosseous abscess may
form, typically seen as a focal intramedullary T2-weighted hyperintensity with variable rim enhancement.
Subsequently, other osteomyelitic features such as
sequestrum, involucrum, and cloaca formation may also
become apparent.
Figure 14. A case of
septic arthritis of the left sternoclavicular joint. (a) Coronal T1-weighted, (b) short-tau inversion recovery, (c) coronal, and (d) axial post-contrast T1-weighted fat-supressed magnetic resonance images show enhancing soft tissues (open arrows in [c] and [d]), bone marrow oedema of the medial clavicle and adjacent manubrium (arrowheads in [b]), and bony erosion of the medial end of the clavicle (arrows in [a]).
Figure 15. A case of
Staphylococcus aureus septic arthritis of the right sternoclavicular joint. (a, b) Ultrasound shows gross capsular thickening of the joint (arrows in [a]) with cortical erosion over the articular surface of the clavicular head (arrowhead in [b]). (c) Axial soft tissue window and (d) coronal bone window computed tomography demonstrates enhancing soft tissue and fluid (open arrows in [c]) with subarticular erosions of the medial clavicle and adjacent manubrium (curved arrows in [d]). (e, f) Gallium-67 single-photon emission computed tomography/computed tomography of the thorax shows increased gallium activity involving the right sternoclavicular joint, adjacent right upper chest wall muscles with probable extension into the right medial clavicular head (circles).
Figure 16. A case of tuberculous osteomyelitis of the left clavicle. (a)
Coronal and (b) axial soft tissue window computed tomography (CT) images
demonstrate a lytic lesion at the clavicular head with cortical destruction (circle
in [a]) and adjacent soft tissue swelling (arrows in [b]). (c) Axial T1-weighted,
(d) short-tau inversion recovery (STIR), (e) axial, and (f) coronal post-contrast
T1-weighted fat-supressed magnetic resonance images demonstrate a
corresponding intramedullary T1-weighted hypointense, STIR hyperintense
lesion with peripheral enhancement at the clavicular head (open arrows), and
adjacent subcutaneous soft tissue oedema and rim-enhancing collection
(curved arrow in [e]). (g) CT-guided biopsy confirms mycobacterial infection.
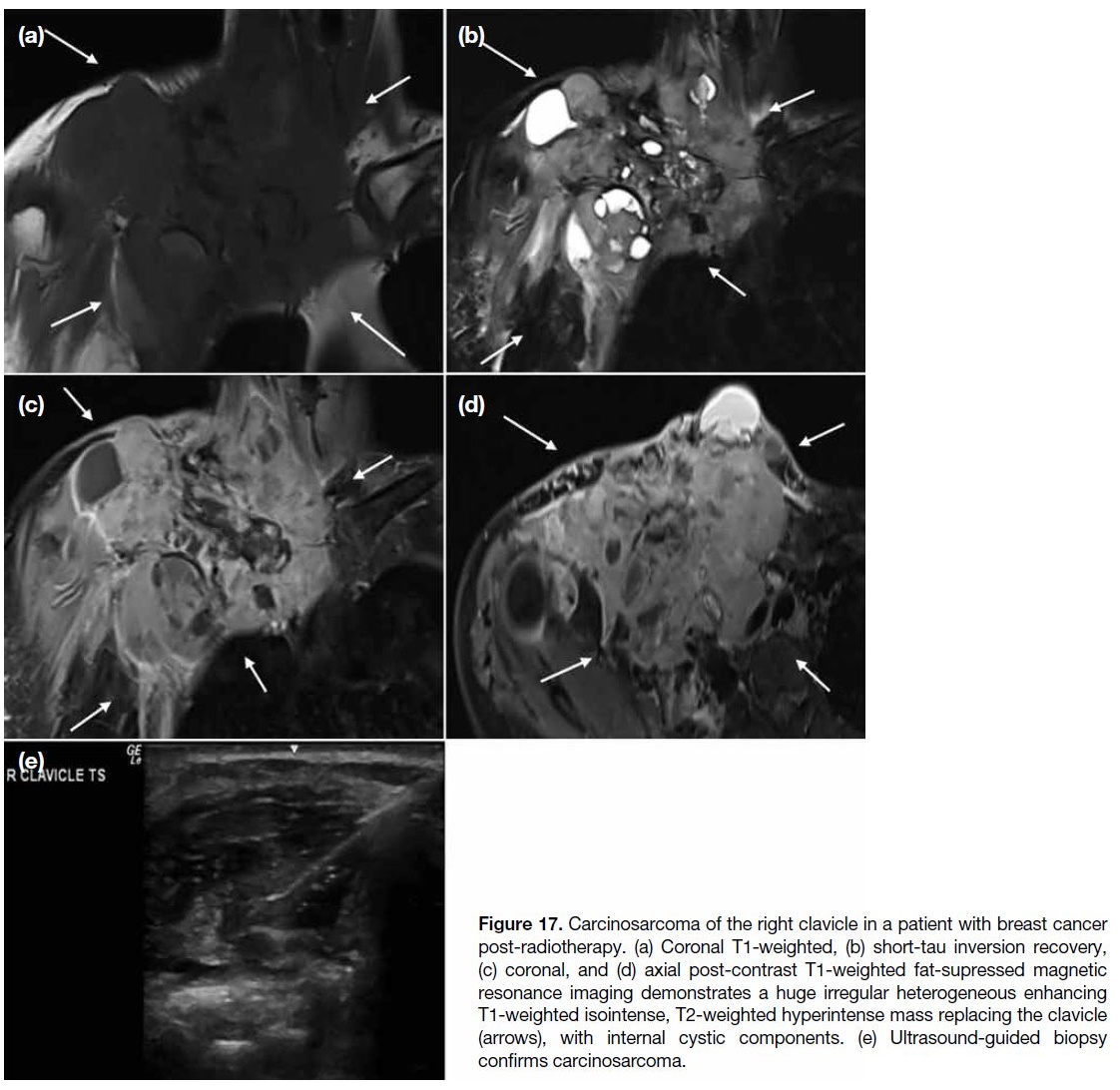
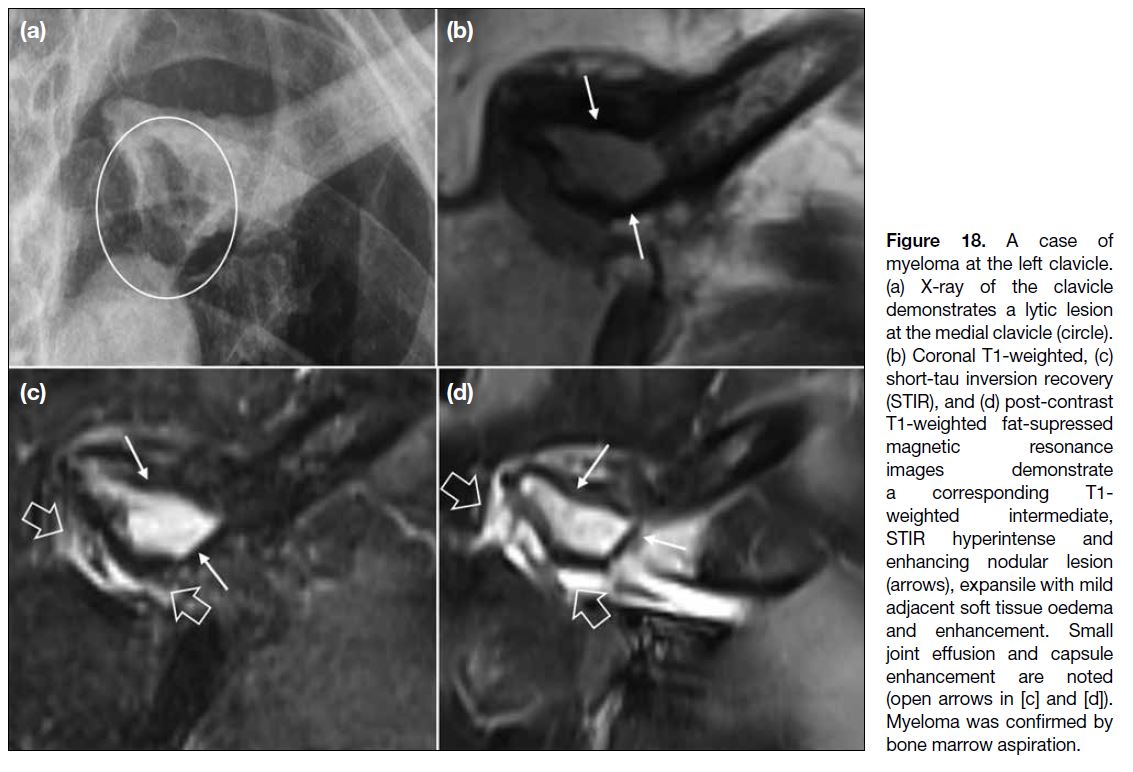
Neoplasm
Bone tumours of the clavicle are rare, with a reported
frequency of less than 1% of all bone tumours.[6] While
primary bone tumour of the clavicle is uncommon, the majority are malignant and include plasmacytoma,
osteosarcoma, and Ewing’s sarcoma (Figures 17, 18 and 19).
Bone metastases can involve the clavicle, with breast,
lung, and prostate cancer being the more common
primaries. Radiological features of aggressive bone
tumours on radiographs and CT include a wide zone of
transition, cortical destruction, and periosteal reaction.
On MRI, there is invariably marrow replacement,
sometimes with bony destruction, extraosseous extension, and perilesional oedema.
Figure 17. Carcinosarcoma of the right clavicle in a patient with breast cancer
post-radiotherapy. (a) Coronal T1-weighted, (b) short-tau inversion recovery, (c) coronal, and (d) axial post-contrast T1-weighted fat-supressed magnetic resonance imaging demonstrates a huge irregular heterogeneous enhancing T1-weighted isointense, T2-weighted hyperintense mass replacing the clavicle (arrows), with internal cystic components. (e) Ultrasound-guided biopsy confirms carcinosarcoma.
Figure 18. A case of
myeloma at the left clavicle. (a) X-ray of the clavicle demonstrates a lytic lesion at the medial clavicle (circle). (b) Coronal T1-weighted, (c) short-tau inversion recovery (STIR), and (d) post-contrast T1-weighted fat-supressed magnetic resonance images demonstrate a corresponding T1-weighted intermediate, STIR hyperintense and enhancing nodular lesion (arrows), expansile with mild adjacent soft tissue oedema and enhancement. Small joint effusion and capsule enhancement are noted (open arrows in [c] and [d]). Myeloma was confirmed by bone marrow aspiration.
Figure 19. Two cases of bone metastases to the clavicle. (a-d) First case. (a) Radiograph of the left clavicle demonstrates an expansile
destructive lytic lesion at the clavicular head with indistinct superior cortex (circle). (b) Axial soft tissue window computed tomography
demonstrates a suspicious irregular hypoenhancing lung lesion in the lingula (open arrow), subsequently diagnosed as epidermal growth
factor receptor mutation–positive lung carcinoma. (c) Axial bone window computed tomography (CT) and (d) positron emission tomography/CT demonstrate an expansile destructive lesion in the left clavicular head with pathological fracture and increased 18F-fluorodeoxyglucose
uptake (arrows), compatible with bone metastasis. The right clavicular head is unremarkable. (e-g) Second case. (e, f) Axial bone window CT
of bilateral clavicles of a patient with known prostate cancer demonstrate sclerotic lesions in the distal clavicle diaphyses (arrowheads). (g) Bone scan demonstrates innumerable foci of increased uptake, including the corresponding distal clavicles (circles), indicating disseminated bone metastasis.
CONCLUSION
The clavicle, AC joint, and sternoclavicular joint are
important structures of the upper extremity. To make an
accurate diagnosis for treatment guidance, radiologists
need to be familiar with the normal anatomy as well as
the radiological features of abnormalities across different
imaging modalities.
REFERENCES
1. Klein MA, Miro PA, Spreitzer AM, Carrera GF. MR imaging of
the normal sternoclavicular joint: spectrum of findings. AJR Am J
Roentgenol. 1995;165:391-3. Crossref
2. Olivier T, Kasprzak K, Herteleer M, Demondion X, Jacques T,
Cotten A. Anatomical study of the sternoclavicular joint using
high-frequency ultrasound. Insights Imaging. 2022;13:66. Crossref
3. Flores DV, Goes PK, Gómez CM, Umpire DF, Pathria MN.
Imaging of the acromioclavicular joint: anatomy, function,
pathologic features, and treatment. Radiographics. 2020;40:1355-82. Crossref
4. Restrepo CS, Martinez S, Lemos DF, Washington L, McAdams HP,
Vargas D, et al. Imaging appearances of the sternum and
sternoclavicular joints. Radiographics. 2009;29:839-59. Crossref
5. Depasquale R, Kumar N, Lalam RK, Tins BJ, Tyrrell PN, Singh J,
et al. SAPHO: what radiologists should know. Clin Radiol.
2012;67:196-206. Crossref
6. Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007;15:239-48. Crossref