Clinical and Imaging Outcomes of Radiosynoviorthesis in Haemophilic Arthropathy
ORIGINAL ARTICLE
Hong Kong J Radiol 2025;28:Epub 9 December 2025
Clinical and Imaging Outcomes of Radiosynoviorthesis in
Haemophilic Arthropathy
KH Chu1, FY Wan1, L Xu1, TWY Chin1, IWC Wong2, CP Lam3, JSM Lau3, MK Chan1, KC Lai1
1 Department of Diagnostic and Interventional Radiology, Queen Elizabeth Hospital, Hong Kong SAR, China
2 Nuclear Medicine Unit, Queen Elizabeth Hospital, Hong Kong SAR, China
3 Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China
Correspondence: Dr KH Chu, Department of Diagnostic and Interventional Radiology, Queen Elizabeth Hospital, Hong Kong SAR,
China. Email: ckh975@ha.org.hk
Submitted: 12 December 2024; Accepted: 9 May 2025. This version may differ from the final version when published in an issue.
Contributors: KHC and KCL designed the study. All authors acquired and analysed the data. KHC, FYW and LX drafted the manuscript. FYW,
LX, TWYC, IWCW, CPL, JSML, MKC and KCL critically revised the manuscript for important intellectual content. All authors had full access
to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This research was approved by the Central Institutional Review Board of Hospital Authority, Hong Kong (Ref No.: CIRB-2024-113-1). A waiver of informed consent was obtained from the Board due to the retrospective nature of the study, with strict protections in
place to ensure patient privacy and the anonymity of personal data.
Abstract
Introduction
Radiosynoviorthesis, the intra-articular injection of radionuclides, is an established treatment for
haemophilic arthropathy. This study aimed to examine the clinical and imaging outcomes of radiosynoviorthesis
in Hong Kong.
Methods
A retrospective review of the radiosynoviorthesis cases performed from 2014 to 2023 in our tertiary
referral centre was conducted. Patients’ demographics, involved joints, injected radionuclides, technical success,
complications, and clinical outcomes (symptoms and frequency of bleeding) were assessed.
Results
Radiosynoviorthesis was performed on 47 joints (22 knees, 14 elbows, 8 ankles, 2 hips, and 1 shoulder) in
26 patients. Joint injections were performed under fluoroscopic or ultrasound guidance, with a technical success
rate of 98%. Six (13%) joints showed mild systemic absorption, and two (4%) joints developed transient radiation
synovitis. No major complications were encountered. Excellent clinical outcomes were observed, with 83% of cases
demonstrating symptomatic improvement and 91% showing a reduction in bleeding frequency. The mean monthly
bleeding frequency decreased from 2.2 episodes before the procedure to 0.6 episode afterwards (p = 0.005). The
total number of hospitalisations or outpatient clinic visits due to haemarthrosis decreased from 60 to 31 in the year
following the procedure (p = 0.01).
Conclusion
Our case series suggests that radiosynoviorthesis is a safe and effective procedure that can improve
clinical symptoms and reduce bleeding frequency in haemophilic arthropathy. It should be considered as part of a
multidisciplinary management approach.
Key Words: Hemarthrosis; Hemophilia A; Injections; Knee; Radiotherapy
中文摘要
血友病性關節病放射性滑膜切除術的臨床和影像學結果
朱僑栩、尹芳盈、徐璐、錢永恩、黃偉宗、林靖邦、劉詩敏、陳文光、黎國忠
引言
放射性滑膜切除術,即關節內注射放射性核素,是治療血友病性關節病的成熟方法。本研究旨在探討放射性滑膜切除術在香港的臨床與影像學成效。
方法
本研究回顧分析了本中心於2014年至2023年間進行的放射性滑膜切除術病例。評估內容包括患者的人口學特徵、受累關節、注射的放射性核素種類、技術成功率、併發症,以及臨床療效(症狀及出血頻率)。
結果
共為26位患者的47個關節(包括22個膝關節、14個肘關節、8個踝關節、2個髖關節及1個肩關節)進行放射性滑膜切除術。關節注射在透視或超聲影像引導下進行,技術成功率達98%。其中6個關節(13%)出現輕微的全身性放射性物質吸收,2個關節(4%)出現短暫性放射性滑膜炎,未見重大併發症。臨床效果理想,83%的病例症狀有所改善,91%的病例出血頻率下降。平均每月出血次數由術前的2.2次顯著下降至術後的0.6次(p = 0.005)。術後一年內,因關節積血而導致的住院及門診就診總次數由60次減少至31次(p = 0.01)。
結論
本病例系列顯示,放射性滑膜切除術是一項安全且有效的治療方式,能改善血友病性關節病患者的臨床症狀並降低出血頻率,應納入多學科綜合治療方案中。
INTRODUCTION
Patients with haemophilia and von Willebrand disease
show an increased tendency to bleed. These patients can
present with recurrent haemarthrosis.[1] The synovium
becomes hypertrophied due to the inflammatory
response to iron deposition within the joint.[2] Increased
vascularity in the inflamed synovium renders it more
prone to bleeding. This creates a vicious cycle, leading to
cartilage and bone damage and resulting in arthropathy.
Prevention and treatment of musculoskeletal damage are
paramount in the care of patients with bleeding disorders.
Prophylactic measures include coagulation factor
replacement therapy and subcutaneous emicizumab
injections to reduce bleeding and prevent subsequent
haemarthropathy.[3] These measures have provided
greater protection for patients and significantly improved
patients’ quality of life. However, recurrent haemarthrosis
remains an issue for some patients despite advances in
medical treatments.[3] In the past, surgical synovectomy
was employed in patients who failed to respond to
medical treatment.[4] Over time, more studies have
reported favourable clinical outcomes with non-surgical
synovectomy, which includes intra-articular injection of
radioisotopes (radiosynoviorthesis) or antibiotics such as rifampicin.[1] [5] [6] [7] These minimally invasive interventions
have gained popularity and are now considered viable
alternatives to surgery.[8] [9] Surgery is reserved for cases
when intra-articular injections are unsuccessful.
Radiosynoviorthesis, also referred to radiation
synovectomy, involves the injection of radionuclides
into affected joints, leading to fibrosis of the inflamed
and hypertrophied synovium.[10] The primary objectives
of this treatment are to reduce bleeding frequency and
alleviate clinical symptoms such as pain and swelling.
Once absorbed by the synovium, the radionuclides emit
high-energy beta particles that induce cell death and
obliterate the capillary blood supply.[11] This results in
fibrosis and sclerosis of the synovial membrane, as well
as a significant decrease in inflammatory activity and
angiogenesis, ultimately reducing the bleeding tendency.
Although international guidelines and studies are
available for Western populations, there remains a
limited focus on Asian haemophilic patients and our
local population.[12] [13] In this retrospective study, we aimed
to evaluate the technical success, efficacy, and safety
of radiosynoviorthesis in our tertiary referral centre in
Hong Kong.
METHODS
All cases of radiosynoviorthesis performed on patients
with haemophilic arthropathy in Queen Elizabeth
Hospital between 2014 and 2023 were retrospectively
reviewed. Data were collected on patient demographics,
type of bleeding disorder, joints treated, radionuclides
administered, technical success, clinical outcomes, and
complications.
Technical success was defined as successful joint
puncture and intra-articular injection of radionuclides,
confirmed by postprocedural scintigraphy. Clinical
outcomes were assessed by evaluating patient records
for changes in joint pain, swelling, and bleeding
frequency. As transient synovitis could cause temporary
symptoms following the procedure, patients’ symptoms
were evaluated at least 3 months afterwards. Clinical
assessments were performed during follow-up visits 6
to 12 months post procedure. Bleeding frequency was
compared by analysing the monthly bleeding episodes
before the procedure and 12 months after the procedure.
The number of hospitalisations or outpatient clinic
appointments due to haemarthrosis during the same
period was also recorded. Comparisons were analysed
using the Wilcoxon signed-rank test.
Techniques
Patients with disturbing pain and recurrent haemarthrosis
(defined as three or more bleeding episodes in the
same joint over 6 months) despite medical treatment,
and with clinical or radiological evidence of synovitis,
were considered indicated for radiosynoviorthesis
and referred by haematologists.[10] Initial evaluation
was conducted by nuclear medicine physicians.
Contraindications included pregnancy, breastfeeding,
or local skin infection at the targeted joint.[14] Relative
contraindications included severe joint instability, bony
destruction, or significant cartilage loss. Preprocedural
imaging, including X-rays, ultrasound, and/or magnetic
resonance imaging, was used to assess the severity of
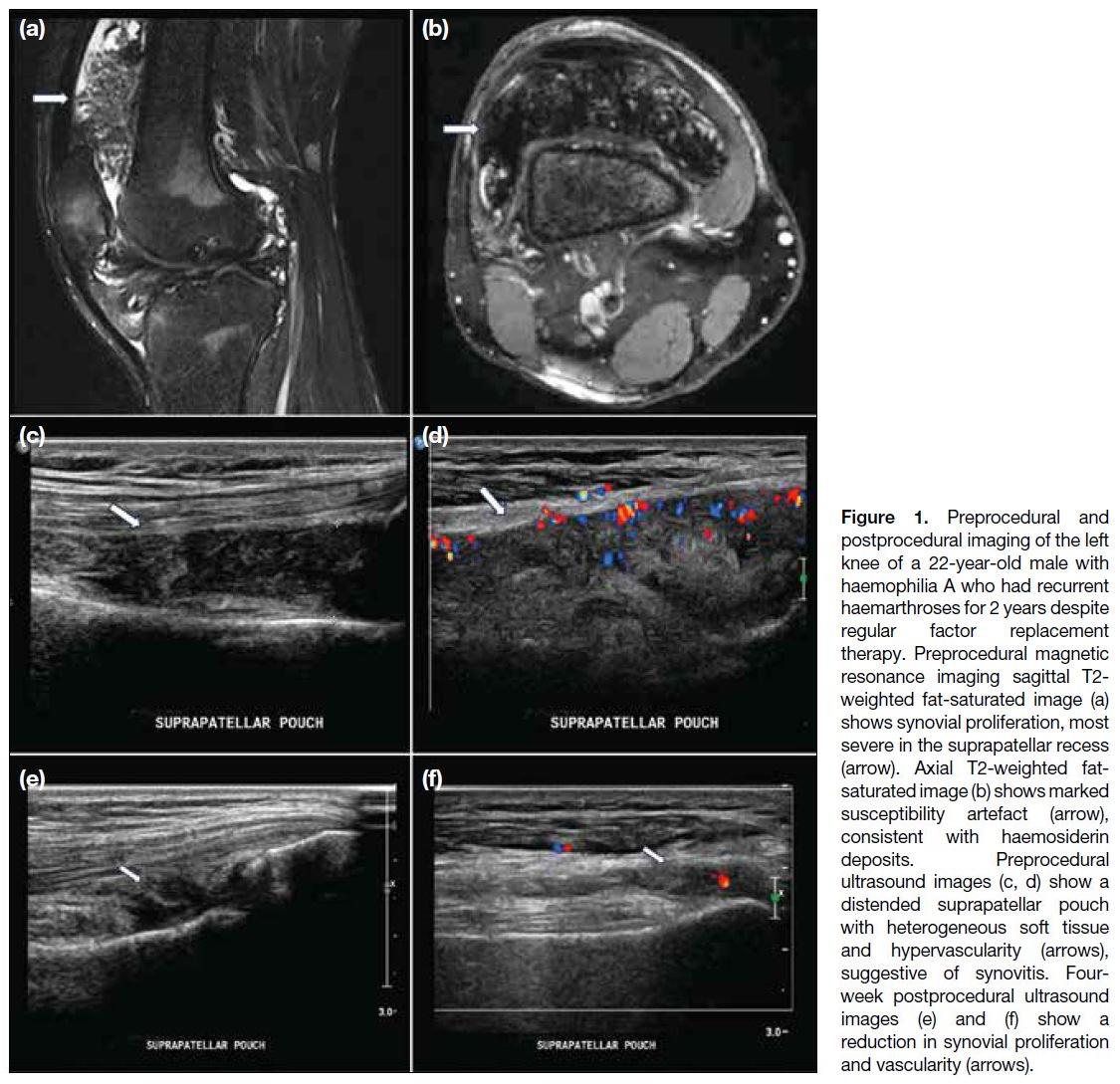
synovitis and arthropathy (Figure 1).
Figure 1. Preprocedural and
postprocedural imaging of the left knee of a 22-year-old male with haemophilia A who had recurrent haemarthroses for 2 years despite regular factor replacement therapy. Preprocedural magnetic resonance imaging sagittal T2-weighted fat-saturated image (a) shows synovial proliferation, most severe in the suprapatellar recess (arrow). Axial T2-weighted fat-saturated image (b) shows marked susceptibility artefact (arrow), consistent with haemosiderin deposits. Preprocedural ultrasound images (c, d) show a distended suprapatellar pouch with heterogeneous soft tissue and hypervascularity (arrows), suggestive of synovitis. Four-week postprocedural ultrasound images (e) and (f) show a reduction in synovial proliferation and vascularity (arrows).
The choice of radionuclides was based on the size of the
joint and required tissue penetration. Two beta-emitting
isotopes were used, namely, yttrium-90 (90Y) and
rhenium-186 (186Re).[15] These isotopes exhibit different
physical characteristics. 90Y, with a maximum beta
energy of 2.26 MeV and a mean tissue penetration of
3.6 mm, was used for knee joint. 186Re, with a maximum
beta energy of 0.98 MeV and a mean penetration of 1.2
mm, was employed for medium-sized joints including the hip, shoulder, elbow, and ankle. Doses ranged from
4.4 to 5.2 mCi (162.8-192.4 MBq) of 90Y for knees, 2.1
to 2.2 mCi (77.7-81.4 MBq) of 186Re for ankles, and
5.3 mCi (196.1 MBq) of 186Re for shoulders and hips.
All procedures were performed in ambulatory setting.
Under ultrasound or fluoroscopic guidance, the joint was
punctured, and contrast medium was injected to confirm
intra-articular location. The radionuclide was then
administered, along with a long-acting corticosteroid
such as triamcinolone acetonide, to reduce the risk of
radiation-induced synovitis and minimise leakage.[11] The
needle tract was flushed with saline during withdrawal to
prevent radiation necrosis of the puncture site.
After the procedure, the affected joint was immobilised
for 48 hours using a splint to reduce the risk of leakage
into surrounding tissues.[16] Bremsstrahlung imaging was
employed within 24 hours to confirm intra-articular
distribution of the radiopharmaceutical. Patients were
counselled on hygiene precautions due to urinary
excretion of the radionuclide. They were instructed to
flush the toilet twice after each use, wash their hands
thoroughly, avoid soiling underclothing or areas around
the toilet bowl, and wash any soiled garments separately.
Clinical follow-up was carried out by haematologists.
RESULTS
A total of 26 male patients, aged between 10 and 57
years (median, 35), underwent radiosynoviorthesis
during the study period (Table). The mean duration of
follow-up was 76 months (range, 10-116). Among them,
23 patients had haemophilia A, two had haemophilia B,
and one had von Willebrand disease. A total of 47 joints
were injected: 22 (47%) knees, 14 (30%) elbows, eight
(17%) ankles, two (4%) hips, and one (2%) shoulder.
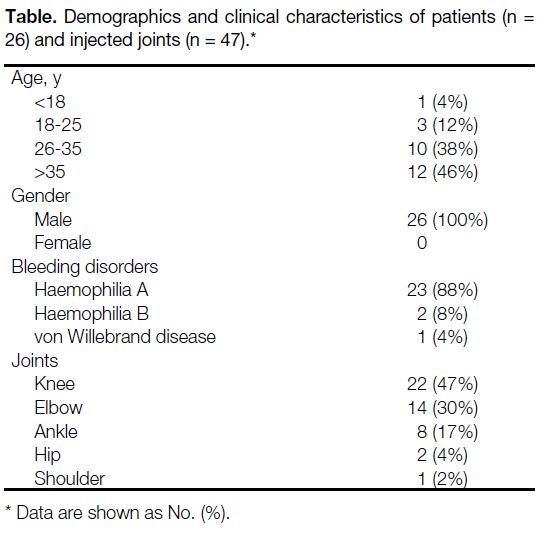
Table. Demographics and clinical characteristics of patients (n = 26) and injected joints (n = 47).
Technical success was achieved in 46 (98%) out of the
47 joints. In one case, the right hip joint could not be
accessed due to advanced degenerative changes.
Improvement in symptoms, specifically pain
and swelling, was observed in 38 (83%) joints
(95% confidence interval [95% CI] = 69%-92%).
Eight (17%) joints showed no change in symptoms
(95% CI = 8%-31%), and no joint demonstrated
worsening. Three patients experienced partial symptom
relief after the first injection and subsequently underwent
a second injection 6 months later, after which all
reported further improvement. Although routine
follow-up imaging was not conducted for every patient, ultrasound in selected cases showed reduced synovial
proliferation and vascularity, indicating improvement
(Figure 1).
A reduction in bleeding frequency was noted in 42
(91%) joints (95% CI = 79%-98%), while four (9%)
joints showed no change (95% CI = 2%-21%). No
joint exhibited increased bleeding frequency. The mean
monthly bleeding frequency decreased from 2.2 episodes
(range, 0.5-6) before the procedure to 0.6 episode
(range, 0-4) afterwards (p = 0.005). Hospitalisations and
outpatient clinic visits due to haemarthrosis decreased from 60 to 31 in the year following the procedure (p = 0.01).
There were no major complications or procedure-related
mortality. There were no documented cases of bleeding,
infection, or necrosis.[17] [18] Minor complications or side-effects
were observed in eight cases. Six (13%) joints
showed postprocedural scintigraphic uptake in the liver
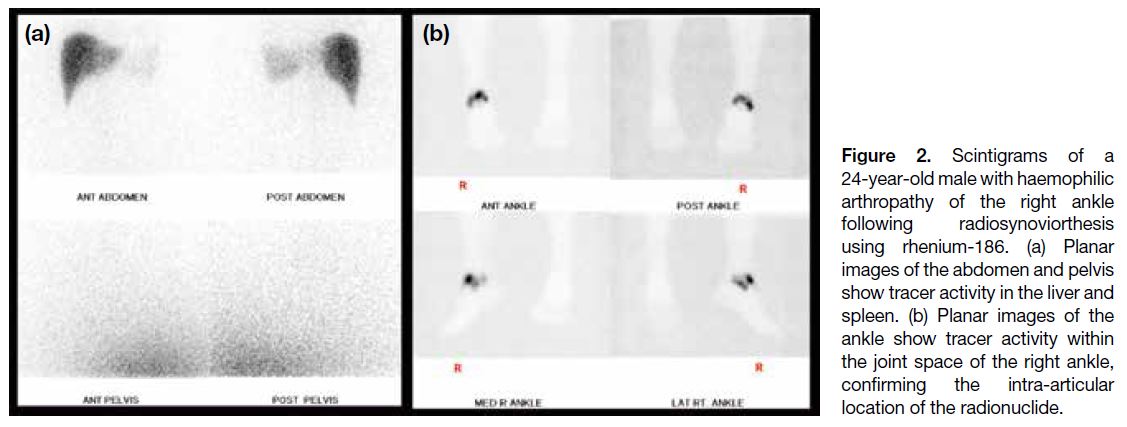
and spleen, suggestive of systemic absorption (95% CI = 5%-26%) [Figure 2]. Liver function tests during follow-up
were normal, and these patients still experienced
clinical improvement.
Figure 2. Scintigrams of a
24-year-old male with haemophilic
arthropathy of the right ankle
following radiosynoviorthesis
using rhenium-186. (a) Planar
images of the abdomen and pelvis
show tracer activity in the liver and
spleen. (b) Planar images of the
ankle show tracer activity within
the joint space of the right ankle,
confirming the intra-articular
location of the radionuclide.
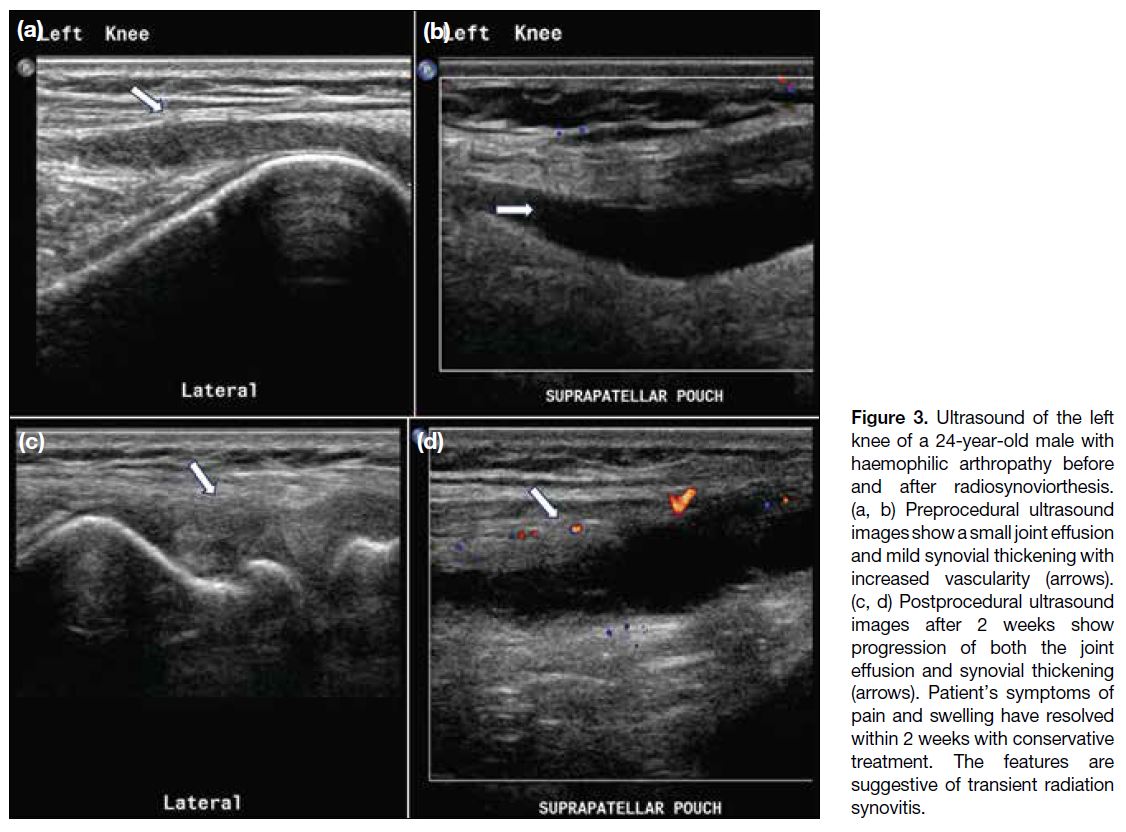
Two (4%) joints developed transient radiation
synovitis (95% CI=0.5%-15%), characterised by pain
and swelling shortly after the procedure. Ultrasound
confirmed increased joint effusion and synovitis (Figure 3). These symptoms resolved within 2 weeks following
conservative treatment with ice packs and nonsteroidal
anti-inflammatory drugs.
Figure 3. Ultrasound of the left
knee of a 24-year-old male with
haemophilic arthropathy before
and after radiosynoviorthesis.
(a, b) Preprocedural ultrasound
images show a small joint effusion
and mild synovial thickening with
increased vascularity (arrows).
(c, d) Postprocedural ultrasound
images after 2 weeks show
progression of both the joint
effusion and synovial thickening
(arrows). Patient’s symptoms of
pain and swelling have resolved
within 2 weeks with conservative
treatment. The features are
suggestive of transient radiation
synovitis.
DISCUSSION
This study demonstrated that most patients with bleeding
disorders and recurrent haemarthrosis responded well
to radiosynoviorthesis. Our findings are consistent with previous international studies. A systematic review
and a meta-analysis reported an overall response rate
of 72.5%.[19] Radiosynoviorthesis can be performed in
paediatric patients with appropriate selection and dosage
adjustment,[20] as shown by the successful treatment of
a 10-year-old in our cohort. It offers the advantages of
reduced hospital stays and lower costs compared with
surgical synovectomy. Moreover, it can be repeated up to
three times per joint, with intervals of at least 6 months.[21]
It can be difficult to perform intra-articular injection,
particularly in patients with severely deformed joints.
According to the literature, the best clinical improvement
was identified in patients with high inflammatory
activity in an early phase of arthropathy.[22] Therefore,
this procedure is expected to have maximal benefit in
patients in the earlier stages of arthropathy.
Radiosynoviorthesis is well tolerated, with a low
incidence of side-effects or complications. Extra-articular
activity was uncommon and was not accompanied by
clinically significant side-effects. Direct leakage out of
the joint space was rare, but systemic absorption could
occur due to uptake by the lymphatic circulation and,
subsequently, the bloodstream. This may be reduced by
immobilisation of the joints. Patients were encouraged
to increase their fluid intake and to void frequently.
Two patients experienced radiation-induced synovitis in
our review. It was a clinical manifestation of rapid and
extensive synovial tissue necrosis that can occur 6 to
48 hours after the procedure.[23] The joint pain, swelling,
and effusion are usually self-limiting and can be treated
conservatively by cooling the joint with ice packs and, if necessary, with anti-inflammatory drugs. Intra-articular
corticosteroid injection during the procedure can reduce
inflammation and decrease leakage of the radioisotope
through dilated capillaries of the synovium into the
systemic circulation.
Limitations
There are several limitations in this study. First, it
was retrospective in nature, with a relatively small
cohort size, and no control arm was available for
comparison. Nonetheless, this study still offered
results in our local population that were in line with
other studies demonstrating the efficacy and safety of
radiosynoviorthesis.[5] [6] [7] [10] [22] Another limitation was the
heterogeneous study population, with different joints
involved and varying severity of arthropathy. In general,
most patients still showed favourable clinical outcomes.
Subgroup analysis may be considered in the future with
a larger number of patients.
There was no objective pain scoring system in place to
provide a quantitative assessment of clinical symptoms,
nor was there a standardised magnetic resonance imaging
protocol to exclude patients with severe cartilage loss or
degenerative joint conditions that could contribute to
pain. A prospective study would be ideal for recruiting
patients and conducting assessments using an objective
scoring system for symptoms and a standard follow-up
protocol. Radiological investigations, such as ultrasound,
can be used to assess for synovitis and serve as another
objective parameter in evaluating outcomes. This
approach would also facilitate longitudinal comparisons
to investigate long-term efficacy and allow monitoring
of disease progression. Lastly, there may be potential
confounders such as the co-injection of steroid with the
radionuclides. The use of steroids may have caused a
period of analgesia and helped bridge the gap between
the administration of the radiopharmaceutical and the
onset of the effects of radiosynoviorthesis. However, such an effect was expected to be short term and unlikely
to persist beyond 3 months, when our clinical assessment
was conducted.
CONCLUSION
Radiosynoviorthesis is a safe and effective procedure
which can contribute to symptomatic improvement
and a reduction in bleeding frequency in patients with
haemophilic arthropathy. It should be considered as part
of a multidisciplinary management approach.
REFERENCES
1. van Galen KP, Mauser-Bunschoten EP, Leebeek FW. Hemophilic
arthropathy in patients with von Willebrand disease. Blood Rev.
2012;26:261-6. Crossref
2. Hoots WK, Rodriguez N, Boggio L, Valentino LA. Pathogenesis
of haemophilic synovitis: clinical aspects. Haemophilia. 2007;13
Suppl 3:4-9. Crossref
3. Oldenburg J. Optimal treatment strategies for hemophilia:
achievements and limitations of current prophylactic regimens.
Blood. 2015;125:2038-44. Crossref
4. Llinás A. The role of synovectomy in the management of a target
joint. Haemophilia. 2008;14 Suppl 3:177-80. Crossref
5. Querol-Giner M, Pérez-Alenda S, Aguilar Rodríguez M,
Carrasco JJ, Bonanad S, Querol F. Effect of radiosynoviorthesis
on the progression of arthropathy and haemarthrosis reduction in
haemophilic patients. Haemophilia. 2017;23:e497-503. Crossref
6. Desaulniers M, Paquette M, Dubreuil S, Senta H, Lavallée É,
Thorne JC, et al. Safety and efficacy of radiosynoviorthesis: a
prospective Canadian multicenter study. J Nucl Med. 2024;65:1095-100. Crossref
7. Kavakli K, Aydoğdu S, Omay SB, Duman Y, Taner M, Capaci K,
et al. Long-term evaluation of radioisotope synovectomy with
yttrium 90 for chronic synovitis in Turkish haemophiliacs: Izmir
experience. Haemophilia. 2006;12:28-35. Crossref
8. van Vulpen LF, Thomas S, Keny SA, Mohanty SS. Synovitis and
synovectomy in haemophilia. Haemophilia. 2021;27 Suppl 3:96-102. Crossref
9. Rodriguez-Merchan EC, Wiedel JD. General principles
and indications of synoviorthesis (medical synovectomy) in
haemophilia. Haemophilia. 2001;7 Suppl 2:6-10. Crossref
10. Kampen WU, Boddenberg-Pätzold B, Fischer M, Gabriel M, Klett R, Konijnenberg M, et al. The EANM guideline for
radiosynoviorthesis. Eur J Nucl Med Mol Imaging. 2022;49:681-708. Crossref
11. Fischer M, Mödder G. Radionuclide therapy of inflammatory joint diseases. Nucl Med Commun. 2002;23:829-31. Crossref
12. Hanley J, McKernan A, Creagh MD, Classey S, McLaughlin P,
Goddard N, et al. Guidelines for the management of acute joint
bleeds and chronic synovitis in haemophilia: A United Kingdom
Haemophilia Centre Doctors’ Organisation (UKHCDO) guideline.
Haemophilia. 2017;23:511-20. Crossref
13. Srivastava A, Santagostino E, Dougall A, Kitchen S, Sutherland M,
Pipe SW, et al. WFH Guidelines for the Management of
Hemophilia, 3rd edition. Haemophilia. 2020;26 Suppl 6:1-158. Crossref
14. Chojnowski MM, Felis-Giemza A, Kobylecka M. Radionuclide
synovectomy—essentials for rheumatologists. Reumatologia.
2016;54:108-16. Crossref
15. Knut L. Radiosynovectomy in the therapeutic management of arthritis. World J Nucl Med. 2015;14:10-5. Crossref
16. Ahmad I, Nisar H. Dosimetry perspectives in radiation synovectomy. Phys Med. 2018;47:64-72. Crossref
17. Kampen WU, Matis E, Czech N, Soti Z, Gratz S, Henze E. Serious
complications after radiosynoviorthesis. Survey on frequency and
treatment modalities. Nuklearmedizin. 2006;45:262-8. Crossref
18. Infante-Rivard C, Rivard GE, Derome F, Cusson A, Winikoff R,
Chartrand R, et al. A retrospective cohort study of cancer incidence
among patients treated with radiosynoviorthesis. Haemophilia.
2012;18:805-9. Crossref
19. van der Zant FM, Boer RO, Moolenburgh JD, Jahangier ZN,
Bijlsma JW, Jacobs JW. Radiation synovectomy with (90)yttrium,
(186)rhenium and (169)erbium: a systematic literature review with
meta-analyses. Clin Exp Rheumatol. 2009;27:130-9.
20. Manco-Johnson MJ, Nuss R, Lear J, Wiedel J, Geraghty SJ,
Hacker MR, et al. 32P radiosynoviorthesis in children with
hemophilia. J Pediatr Hematol Oncol. 2002;24:534-9. Crossref
21. Clunie G, Fischer M; EANM. EANM procedure guidelines for radiosynovectomy. Eur J Nucl Med Mol Imaging. 2003;30:BP12-6. Crossref
22. Kresnik E, Mikosch P, Gallowitsch HJ, Jesenko R, Just H,
Kogler D, et al. Clinical outcome of radiosynoviorthesis: a
meta-analysis including 2190 treated joints. Nucl Med Commun.
2002;23:683-8. Crossref
23. Pirich C, Schwameis E, Bernecker P, Radauer M, Friedl M,
Lang S, et al. Influence of radiation synovectomy on articular
cartilage, synovial thickness and enhancement as evidenced by MRI
in patients with chronic synovitis. J Nucl Med. 1999;40:1277-84.